Purpose
The adaptable health alert below is for health departments to notify local public health practitioners, clinicians, public health laboratories, and public information officers about a case, cluster or isolate of DGI in their jurisdiction. Use data from your jurisdiction to make it relevant to your community. You can customize this document further by including further epidemiologic details, reporting requirements, and health department activities.
Customizable template
Summary
- As of [date], [number] cases of disseminated gonococcal infections (DGI) have been diagnosed in [state].
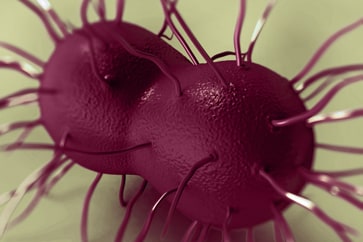
- DGI occurs when the sexually transmitted pathogen Neisseria gonorrhoeae invades the bloodstream and spreads to distant sites in the body, leading to clinical findings such as septic arthritis, polyarthralgia, tenosynovitis, petechial/pustular skin lesions, bacteremia, or, on rare occasions, endocarditis or meningitis.
- If there is clinical suspicion for DGI, nucleic acid amplification test (NAAT) and culture specimens from urogenital and extragenital (e.g., pharyngeal and rectal) mucosal site(s), as applicable, should be collected and processed, in addition to culture specimens from disseminated sites of infection (e.g., skin, synovial fluid, blood, or cerebrospinal fluid [CSF]).
- Management of DGI cases should be guided by the CDC STI Treatment Guidelines. Hospitalization and consultation with an infectious disease specialist are recommended for initial therapy.
- Providers should instruct patients to refer sex partners with whom they have had sexual contact in the past 60 days for evaluation, testing, and presumptive treatment for gonorrhoeae.
- Report all laboratory confirmed and clinically suspected cases of DGI to the [State/local] health department within 24 hours of identification. [Add reporting information here]
- All gonorrhoeae isolates in DGI cases should be tested for antimicrobial susceptibility, which requires culture. Please contact your local health department for guidance and approval to send specimens to the State lab for additional testing.
Background
DGI occurs when the sexually transmitted pathogen Neisseria gonorrhoeae invades the bloodstream and spreads to distant sites in the body, leading to clinical manifestations, such as septic arthritis, polyarthralgia, tenosynovitis, petechial/pustular skin lesions, bacteremia, or, on rare occasions, endocarditis or meningitis. DGI is uncommon and thought to occur in 0.5-3% of untreated gonorrhea cases.
Cultures from disseminated sites of infection are often negative and mucosal sites of infection (e.g. urogenital, rectal, or pharyngeal) are often asymptomatic and not tested before empiric antimicrobial treatment is started despite having a higher diagnostic yield. As a result, DGI is usually a clinical diagnosis without microbiologic confirmation, which likely contributes to underdiagnosis and treatment delays.
Recommendations
If there is clinical suspicion for DGI, NAAT and culture specimens from urogenital and extragenital mucosal site(s), as applicable, should be collected and processed, in addition to culture specimens from disseminated sites of infection (e.g., skin, synovial fluid, blood, or CSF). All N. gonorrhoeae isolates in DGI cases should be tested for antimicrobial susceptibility, which requires culture.
Obtaining a behavioral risk assessment, including a nonjudgmental sexual history, providing STI/HIV prevention counseling, and appropriately treating patients and their sex partners are all necessary to interrupt disease transmission. Management of DGI cases should be guided by the CDC STI Treatment Guidelines. Hospitalization and consultation with an infectious disease specialist are recommended for initial therapy.
Clinical consultation for DGI management is available through the STD Clinical Consultation Network.
CDC is interested in receiving all clinical isolates from DGI cases for additional testing. Please work with your laboratory facility to ensure all available isolates from DGI cases are not discarded and are sent to [the state health laboratory].
[Include further epi details, reporting requirements, and health department activities here, as available.]
