Key points
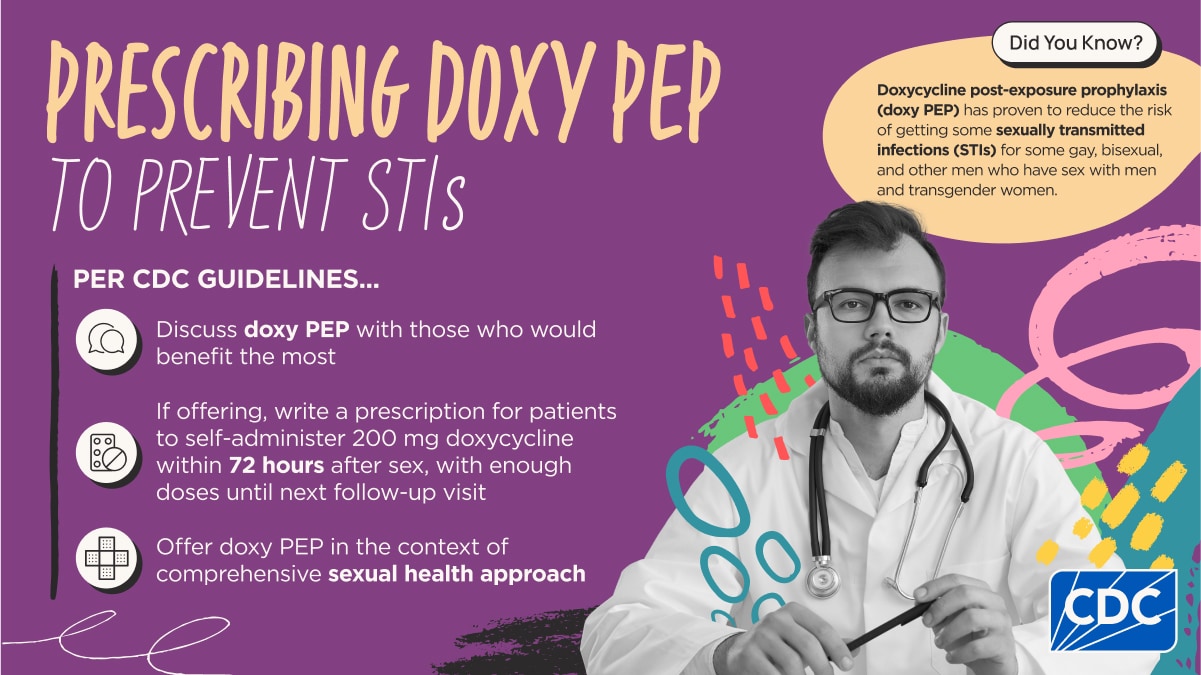
- Healthcare providers can use CDC guidelines to prescribe doxycycline post-exposure prophylaxis (doxy PEP) to prevent bacterial STIs
- Discuss the pros and cons of doxy PEP with gay, bisexual, and other men who have sex with men and transgender women who had a bacterial STI in the last year
- If offering doxy PEP, write a prescription for patients to self-administer 200 mg of doxycycline as soon as possible within 72 hours after sex
- Offer doxy PEP in the context of comprehensive sexual health approach
Overview
CDC encourages providers to use Clinical Guidelines on the Use of Doxycycline Post-exposure Prophylaxis for Bacterial STI Prevention to inform doxy PEP practices. These guidelines were developed as part of a comprehensive review of available research, as well as extensive internal and external consultation.
Did you know?
Doxy PEP may improve the health and wellbeing of some patients more likely to get STIs and help combat the rising toll of these infections in the United States.
Doxy PEP is generally well-tolerated and can reduce the likelihood of getting a bacterial STI, though researchers are still studying the long-term effects of doxy PEP. As additional data are available, CDC will update these guidelines.
What you can do
Discuss doxy PEP with patients who would benefit most
CDC recommends healthcare providers discuss doxy PEP with all gay, bisexual, and other men who have sex with men and transgender women with a history of at least one bacterial STI (gonorrhea, chlamydia, and syphilis) in the last 12 months.
Although not directly assessed in the research studies, providers may also wish to discuss doxy PEP with other gay, bisexual, and other men who have sex with men and transgender women who have not had a bacterial STI in the past year but who will be participating in sexual activities known to pose an increased risk of infection.
Providers should discuss the proven benefits of doxy PEP in reducing STIs, as well as the known and unknown risks of this strategy. Implement doxy PEP in the context of comprehensive sexual health counseling.
Prescribe doxy PEP, as appropriate
- Write a prescription for self-administration of doxycycline 200 mg (any formulation) as soon as possible, within 72 hours after oral, vaginal, or anal sex. Patients should not take more than 200 mg every 24 hours. Provide enough doses until next follow up visit.
- Help patients minimize doxycycline side effects by advising that they:
- Take doxy PEP with at least 8 ounces of water and food. This can help reduce side effects like nausea, upset stomach, and esophageal irritation
- Do not lie down for one hour after taking doxycycline
- Do not take doxycycline within two hours of having any dairy products, antacids and supplements with iron, calcium, or magnesium
- Wear sunscreen or cover up to stay protected from the sun while taking doxycycline
- Take doxy PEP with at least 8 ounces of water and food. This can help reduce side effects like nausea, upset stomach, and esophageal irritation
- Set up routine follow-up visits at intervals that align with the patient’s existing HIV and STI screening recommendations based on their chosen HIV prevention strategy, as recommended intervals differ for individuals on HIV PrEP. Patients on doxy PEP should test for STI and HIV every 3 - 6 months as appropriate. During these visits, reassess whether there is an ongoing need for doxy PEP.
Offer doxy PEP in the context of comprehensive sexual health
CDC recommends the following procedures at the initial and follow-up visits for a comprehensive sexual health approach.
When prescribing doxy PEP
- Screen for and treat STIs, including viral hepatitis and HIV, as indicated
- For those without HIV who are receiving HIV PrEP, screen per HIV PrEP guidelines at 3 month intervals
- Discuss and facilitate access to HIV pre-exposure prophylaxis (PrEP) for those who are HIV negative, not on HIV PrEP, and at risk for HIV
- Discuss prevention strategies (condoms, HIV PEP, HIV PrEP, HIV treatment, vaccinations for hepatitis A, hepatitis B, mpox, and human papillomavirus); link to health and social services as indicated
- Review patient's medication list, including over the counter medications, to assess for potential drug interactions
- Provide information on how to take doxy PEP, including how to minimize side effects
- Provide enough doses to last until next follow-up visit based on individual sexual frequency
At follow-up visits every 3 to 6 months
- Continue screening for gonorrhea, chlamydia, and syphilis
- Continue screening and testing for HIV
- Continue to discuss other prevention strategies and link to health and social services as indicated
- Assess doxy side effects
- Re-assess need for doxy PEP
- Provide enough doses until next follow up based on individual sexual frequency
What researchers are still learning
CDC, along with federal partners and other research organizations, is leveraging existing data systems to monitor the uptake of doxy PEP and how this impacts bacterial STI rates, understand national doxycycline prescribing rates, and identify potential development of antimicrobial resistance.
Effectiveness of doxy PEP for other populations
To date, doxy PEP has only proven effective among gay, bisexual, and other men who have sex with men and transgender women at increased risk for STIs, and this is the group for whom CDC recommends counseling.
There is insufficient evidence to assess the balance of benefits and harms of the use of doxy PEP in other populations. Studies in other populations, including cisgender women are vital, and CDC will update the guidelines as additional data are available.
Potential long-term concerns
Questions remain about potential long-term development of antimicrobial resistance and impacts on the microbiome.
CDC's guidelines reviewed available data to date, but studies are currently insufficient to assess the impact of long-term doxy PEP use on the development of antimicrobial resistance, both in bacterial STIs, as well as other common bacterial pathogens, such as Staphylococcus aureus. Additionally, there are few studies to date on the long-term impact on the microbiome (such as the “good” bacteria in our intestines or those that live on our skin).
To help minimize the potential for antimicrobial resistance while maximizing benefits, CDC's guidelines focus on the specific groups for whom doxy PEP has been proven effective for STI prevention and for whom modeling suggests the impact will be most substantial. CDC will continue to use multiple data systems to help monitor for any increases in antimicrobial resistance associated with doxy PEP implementation. As additional data are available from CDC systems and any other research in the field, CDC will update the guidelines.
Suggested citation
Bachmann LH, Barbee LA, Chan P, et al. CDC Clinical Guidelines on the Use of Doxycycline Postexposure Prophylaxis for Bacterial Sexually Transmitted Infection Prevention, United States, 2024. MMWR Recomm Rep 2024;73(No. RR-2):1–8. DOI: http://dx.doi.org/10.15585/mmwr.rr7302a1.
