At a glance
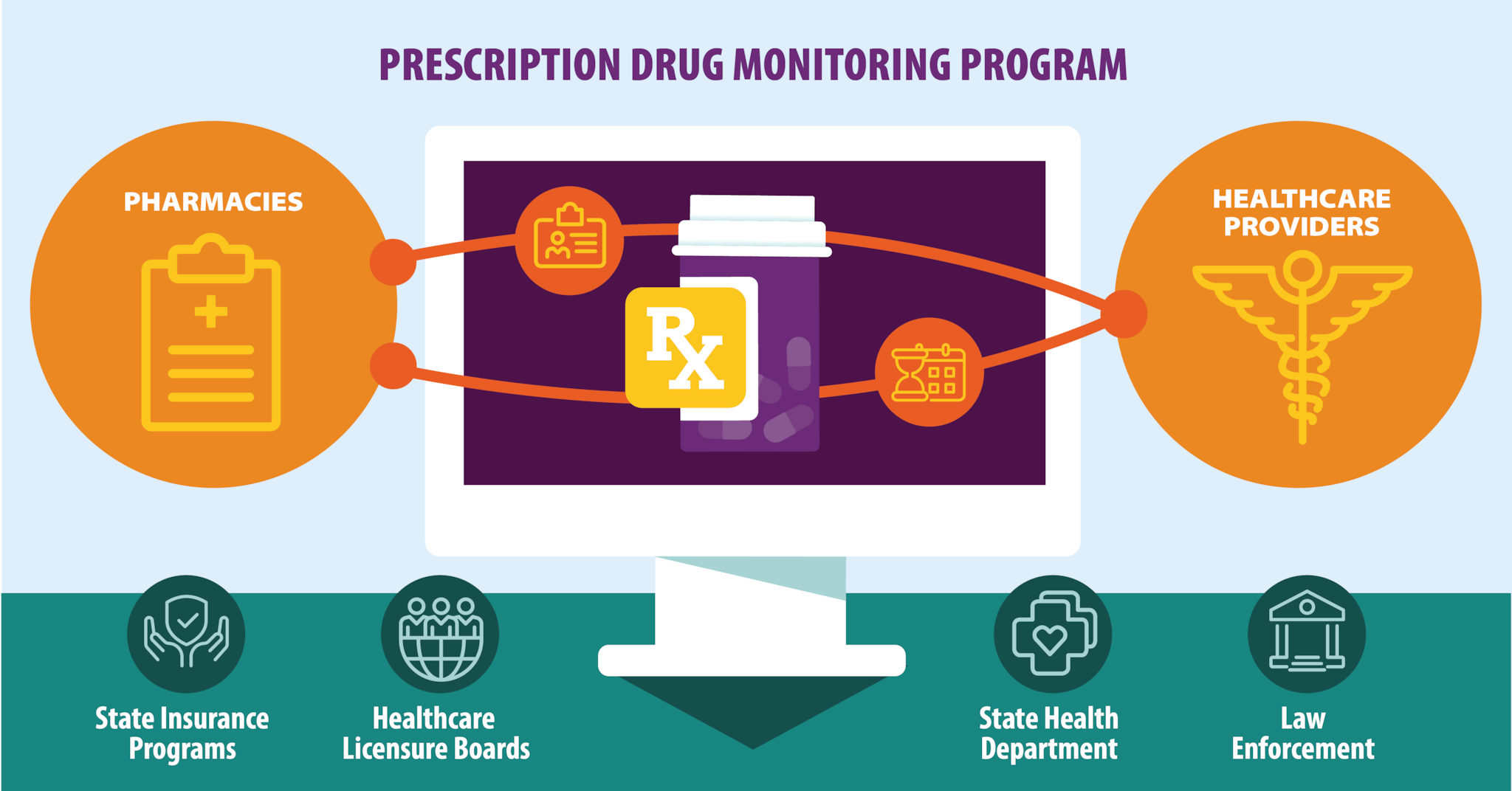
- A prescription drug monitoring program (PDMP) is an electronic database that tracks controlled substance prescriptions in a state.
- PDMPs can provide health authorities timely information about prescribing and patient behaviors that contribute to the epidemic and facilitate a nimble and targeted response.
- View a key resource to learn how PDMPs can support and inform public health interventions and clinical decision-making.
What states need to know
Prescription drug monitoring programs (PDMPs) continue to be among the most promising state-level interventions to improve opioid prescribing, inform clinical practice, and protect patients at risk. Although findings are mixed, evaluations of PDMPs have illustrated changes in prescribing behaviors, use of multiple providers by patients, and decreased substance use treatment admissions.1 States have implemented a range of ways to make PDMPs easier to use and access, and these changes have significant potential for ensuring that the utility and promise of PDMPs are realized.
Key resource
This resource highlights the value of PDMPs as public health tools that can support and inform public health interventions and clinical decision-making. Find key information about PDMP history, importance of PDMP data access, considerations for increasing access to and utilization of PDMP data, implications for PDMPs located within and outside of the state health department, and examples of PDMP use in overdose prevention and response work.
Leveraging Prescription Drug Monitoring Program (PDMP) Data in Overdose Prevention and Response
Promising features of PDMPs
Universal Use
PDMPs are promising tools for healthcare providers to see patients' prescribing histories to inform their prescribing decisions. However, a PDMP is only useful to healthcare providers if they check the system before prescribing. Some states have implemented polices that require providers to check a state PDMP prior to prescribing certain controlled substances and in certain circumstances, and these policies have significant potential for ensuring that the utility and promise of PDMPs are maximized.2
Real-Time
When pharmacists dispense controlled substances to patients, they have to enter the prescription into the state PDMP. However, pharmacies submit this data to state PDMPs at varying intervals—ranging from monthly to daily or even in "real-time," i.e., under five minutes. If there is a long interval between dispensing and submission into the state PDMP, providers and other PDMP users will not have information on patients' most recent prescriptions. Timely data, like in a "real-time" PDMP, maximizes the utility of the prescription history data, with significant implications for patient safety and public health.3
Actively Managed
PDMPs are more than just passive databases. As a public health tool, PDMPs can be used by state health departments to understand the behavior of the epidemic and inform and evaluate interventions. PDMPs can also be used to send "proactive" reports to authorized users to protect patients at the highest risk and identify inappropriate prescribing trends.
Easy to Use and Access
States have taken a number of steps to make PDMPs easier to use and access. Promising practices include integrating PDMPs into electronic health record (EHR) systems,45 permitting physicians to delegate PDMP access to other allied health professionals in their office (e.g., physician assistants and nurse practitioners), and streamlining the process for providers to register with the PDMP.3
Continued state-level evaluation of PDMPs can lead to greater identification and implementation of promising practices.
- Haegerich TM, Jones CM, Cote PO, Robinson A, Ross L. Evidence for state, community and systems-level prevention strategies to address the opioid crisis. Drug Alcohol Depend. 2019 Nov 1;204:107563. doi: 10.1016/j.drugalcdep.2019.107563. Epub 2019 Sep 19. PMID: 31585357; PMCID: PMC9286294.
- Gail KS, Kun Z, John FH, Amy SBB, Grant TB, Peter WK. Effects of mandatory prescription drug monitoring program (PDMP) use laws on prescriber registration and use and on risky prescribing. Drug Alcohol Depend. Volume 199. 2019, Pages 1-9. ISSN 0376-8716. https://doi.org/10.1016/j.drugalcdep.2019.02.010.
- Martin HD, Modi SS, Feldman SS. Barriers and facilitators to PDMP IS Success in the US: A systematic review. Drug Alcohol Depend. 2021 Feb 1;219:108460. doi: 10.1016/j.drugalcdep.2020.108460. Epub 2020 Dec 19. PMID: 33387937.
- Calcaterra SL, Butler M, Olson K, Blum J. The Impact of a PDMP-EHR Data Integration Combined With Clinical Decision Support on Opioid and Benzodiazepine Prescribing Across Clinicians in a Metropolitan Area. J Addict Med. 2022 May-Jun 01;16(3):324-332. doi: 10.1097/ADM.0000000000000905. PMID: 34392255; PMCID: PMC8831644.
- Neprash HT, Vock DM, Hanson A, Elert B, Short S, Karaca-Mandic P, Rothman AJ, Melton GB, Satin D, Markowitz R, Golberstein E. Effect of Integrating Access to a Prescription Drug Monitoring Program Within the Electronic Health Record on the Frequency of Queries by Primary Care Clinicians: A Cluster Randomized Clinical Trial. JAMA Health Forum. 2022 Jun 5;3(6):e221852. doi: 10.1001/jamahealthforum.2022.1852. PMID: 35977248; PMCID: PMC9168784.
