Key points
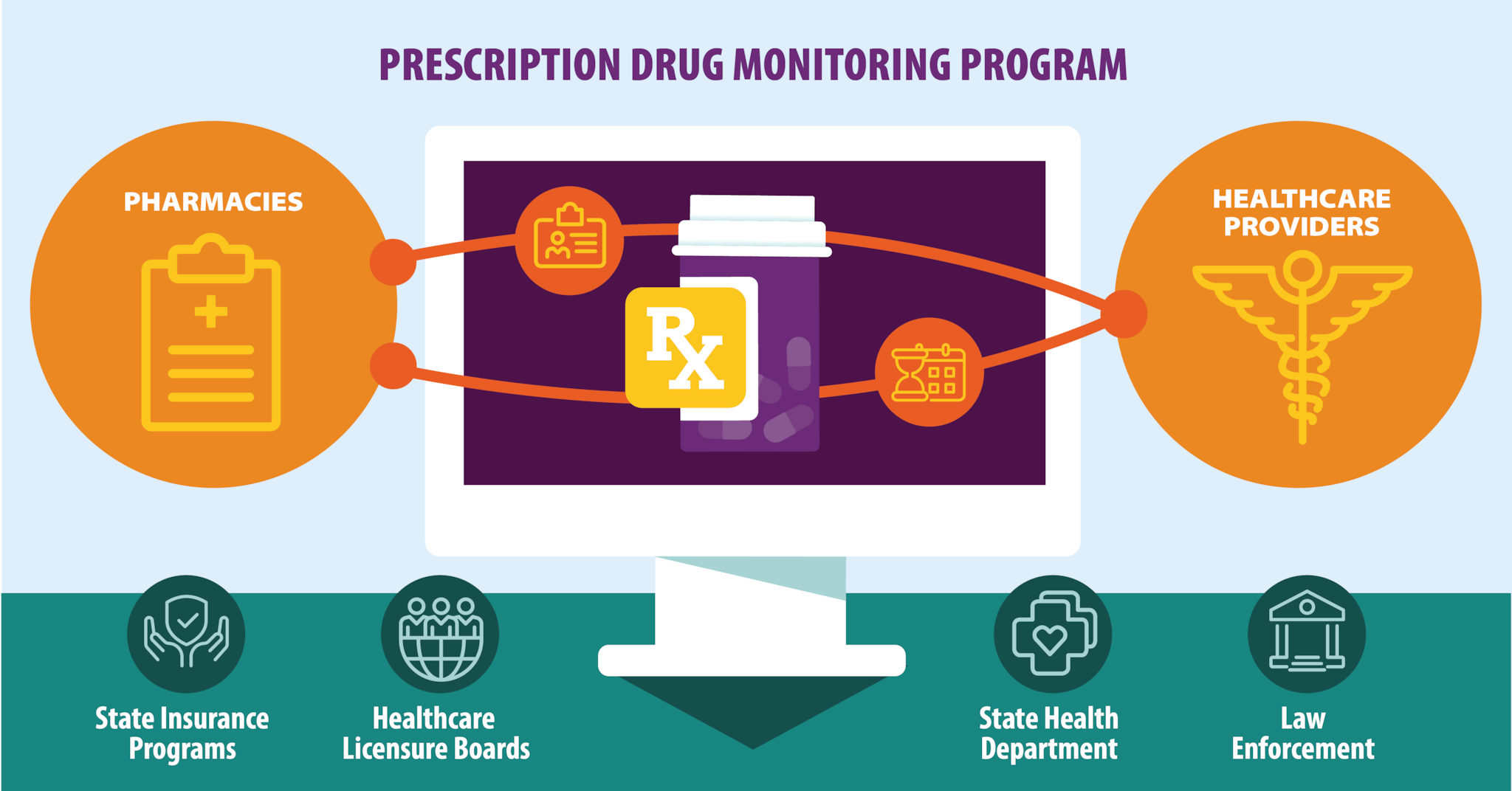
A prescription drug monitoring program (PDMP) is an electronic database that tracks controlled substance prescriptions. Information from PDMPs can help clinicians identify patients who may be at risk for overdose and provide potentially lifesaving information and interventions. PDMP data also can be helpful when patient medication history is unavailable and when care transitions to a new clinician.
When to check the PDMP
Checking the PDMP is an important step to improve opioid prescribing practices.
Check the PDMP:
- When initiating opioid therapy for acute, subacute, or chronic pain.
- Every 3 months or more frequently when continuing opioid therapy.
Ideally, PDMP data should be reviewed before every opioid prescription for acute, subacute, or chronic pain.
Clinicians who are prescribing initial opioid therapy should first review a patient's history of controlled substance prescriptions using a state PDMP (Recommendation 9 in the 2022 Clinical Practice Guideline for Prescribing Opioids for Pain).
PDMPs can help inform point-of-care clinical decision-making to improve patient care and safety. Clinicians should check PDMP data for prescription opioids and other controlled medications patients have received from other clinicians to determine whether a patient is receiving opioid dosages or combinations (e.g., opioids combined with benzodiazepines) that put the patient at high risk for overdose.
What to consider when using the PDMP
Use PDMP data in the context of other clinical information including patient history, physical findings, and relevant testing and screening to help with patient communication and to improve patient safety.
- Calculate the total morphine milligram equivalents (MME)/day for concurrent opioid prescriptions to help assess the patient's overdose risk.
- Do not include buprenorphine in the total MME/day calculations.
- The 2022 Clinical Practice Guideline does not specify a limit for total MME/day.
- Many patients do not experience benefit in pain relief or function from increasing opioid dosages to greater than or equal to 50 MME/day, but are exposed to progressive increases in risk for opioid-related harms as dosage increases.
- Before increasing total opioid dosage to greater than or equal to 50 MME/day, carefully reassess evidence of individual benefits and risks.
- Many patients do not experience benefit in pain relief or function from increasing opioid dosages to greater than or equal to 50 MME/day, but are exposed to progressive increases in risk for opioid-related harms as dosage increases.
- Use caution when prescribing opioid medications and benzodiazepines concurrently. Clinicians should also consider whether benefits outweigh risk of concurrent prescribing of opioids and other central nervous system depressants (e.g., muscle relaxants, non-benzodiazepine sedative hypnotics, potentially sedating anticonvulsant medications such as gabapentin and pregabalin) (Recommendation 11).
- PDMP-generated risk scores are created by algorithms in software applied to patient information. Such scores have not been validated against clinical outcomes such as overdose and should not take the place of clinical judgment.
- Do not include buprenorphine in the total MME/day calculations.
How to use information from the PDMP
A key aim of pain management is the provision of person-centered care built on a foundation of trust between patients and clinicians. Such care includes proper evaluation to identify potentially reversible causes of pain and establish a diagnosis and measurable treatment outcomes that focus on optimizing function and quality of life.1
- Confirm PDMP information with your patient.
- Provide potentially life-saving information and interventions.
- Talk with your patient about the findings and any safety concerns, including increased risk for respiratory depression and overdose if they are receiving overlapping prescription opioids from multiple clinicians who are not coordinating the patient's care, or receiving medications that increase risk when combined with opioids (e.g., benzodiazepines) (Recommendation 11).
- Offer naloxone as part of your patient's management plan to mitigate risk (Recommendation 8).
- Talk with your patient about the findings and any safety concerns, including increased risk for respiratory depression and overdose if they are receiving overlapping prescription opioids from multiple clinicians who are not coordinating the patient's care, or receiving medications that increase risk when combined with opioids (e.g., benzodiazepines) (Recommendation 11).
- Discuss safety concerns with other clinicians who are prescribing controlled substances for your patient.
- Ideally, first discuss concerns with the patient and inform them of your plan to coordinate care with the patient's other clinicians to improve their safety.
- If you think your patient might be sharing or selling prescription opioids and not taking them, consider toxicology testing to help determine whether prescription opioids can be discontinued without causing withdrawal (Recommendation 5). A negative toxicology test might indicate the patient is not taking prescribed opioids, although clinicians should consider other possible reasons for this test result, such as false negative results or misinterpretation of results (Recommendation 10).
- Ideally, first discuss concerns with the patient and inform them of your plan to coordinate care with the patient's other clinicians to improve their safety.
- Do not dismiss patients from care based on PDMP information. Doing so can adversely affect patient safety and could result in missed opportunities to provide potentially lifesaving information (e.g., about risks of prescription opioids and overdose prevention) and interventions (e.g., safer prescriptions, nonopioid pain treatment [Recommendations 1 and 2], naloxone [Recommendation 8], and effective treatment for substance use disorders [Recommendations 8 and 12]).
- PDMP information can be most helpful when results are unexpected, and clinicians should minimize bias in application. Clinicians should apply the practice of checking PDMP data (Recommendation 9) when feasible to all patients rather than differentially based on assumptions about what they will learn about different patients.
- Screen for substance use when appropriate and discuss with your patient in a non-judgmental manner (Recommendations 8 and 12).
Related resources
To find out more and get training on your state's PDMP, visit the PDMP Training and Technical Assistance Center.
- Skelly AC, Chou R, Dettori JR, et al. Noninvasive nonpharmacological treatment for chronic pain: a systematic review. Comparative Effectiveness Review No. 209. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2015-00009-I.) AHRQ Publication No 18-EHC013-EF. Rockville, MD: Agency for Healthcare Research and Quality; June 2018. https://doi.org/10.23970/AHRQEPCCER209
