Key points
- CDC tracks invasive pneumococcal disease (IPD) using 2 surveillance systems.
- Invasive bacterial disease refers to when bacteria invade parts of the body, like blood, that are normally free from germs.
- CDC doesn't track non-invasive pneumococcal disease, such as pneumococcal ear infections.

Data systems
National Notifiable Diseases Surveillance System
Invasive diseases, such as meningitis and bacteremia (bloodstream infections), are the only nationally notifiable diseases caused by Streptococcus pneumoniae bacteria.
CDC collects national information about IPD through the National Notifiable Diseases Surveillance System (NNDSS). CDC receives NNDSS data each week.
Active Bacterial Core surveillance
CDC collaborates with some state health departments to conduct IPD surveillance. Examples of IPD include:
- Meningitis
- Bacteremia
- Osteomyelitis
- Septic arthritis
Information is collected through Active Bacterial Core surveillance (ABCs), which is part of CDC's Emerging Infections Program.
How the data are interpreted
Disease trends
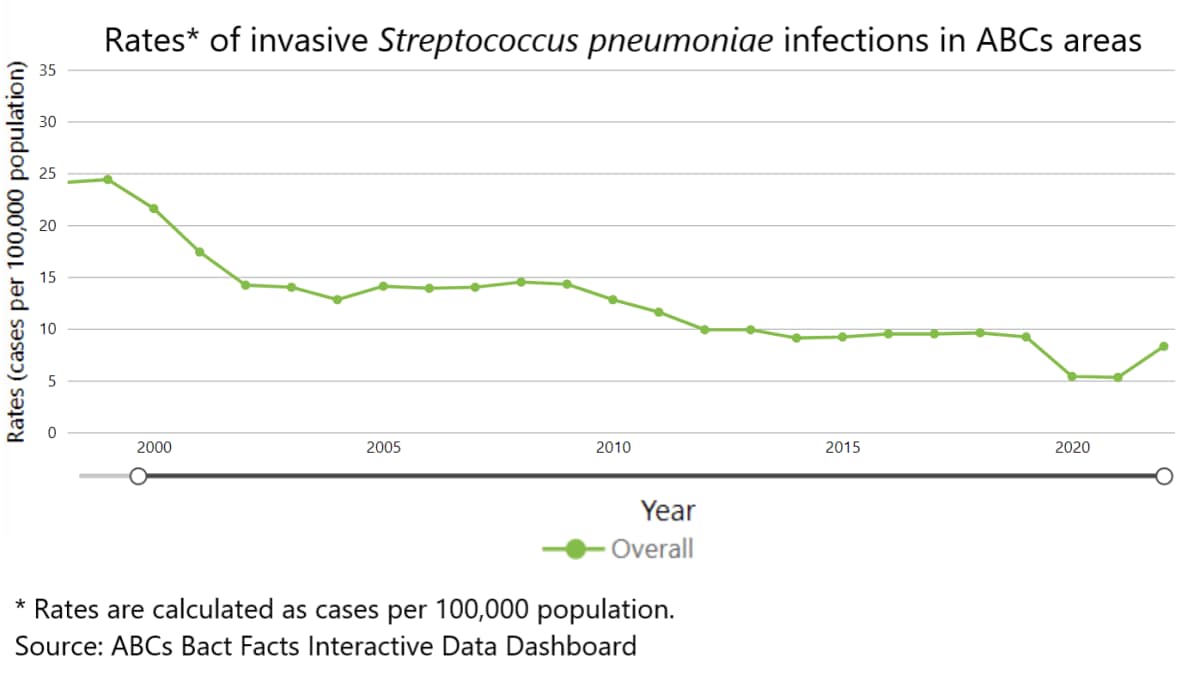
IPD surveillance in the United States began in 1998. IPD rates dramatically declined in children and adults after the United States began using pneumococcal conjugate vaccines (PCVs) in 2000.
Temporal pattern
Pneumococcal infections are more common during the winter and in early spring when respiratory diseases are more prevalent.
Antibiotic resistance
Pneumococcal bacteria that cause IPD are resistant to one or more classes of antibiotics in more than 40% of cases.
Vaccination impact
CDC data show that IPD rates in the United States decreased dramatically after introduction of PCVs.
Childhood vaccination and disease trends
From 1998 through 2021, IPD rates among children less than 5 years old decreased by
- 95% overall
- 99% for disease caused by serotypes covered by PCV13
Adult vaccination and disease trends
IPD rates in adults decreased after PCVs were used in children. PCV use in children can provide herd immunity and decrease IPD rates in adults.
IPD caused by the serotypes covered by 23-valent pneumococcal polysaccharide vaccine (PPSV23) also declined during this time. However, these reductions were due to declines in IPD caused by serotypes in common with PCV13. PPSV23 has been available since 1984.
Data definitions
The Council of State and Territorial Epidemiologists (CSTE) released the most recent case definition for IPD in 2017.
Global trends
The World Health Organization (WHO) estimates that S. pneumoniae kills about 300,000 children under 5 years old worldwide every year. Most of these deaths occur in developing countries.
Leading cause
S. pneumoniae is the leading cause of bacterial pneumonia globally. It accounted for more deaths than all other causes combined in 2016. Most of these deaths occur in countries in Africa and Asia.
Declining rates
Gavi, The Vaccine Alliance, has helped many low-income countries introduce a PCV into their national immunization programs. Countries that introduced a PCV have seen large reductions in IPD and pneumonia.
Resources
Domestic
Pneumococcal disease chapter of the Manual for the Surveillance of Vaccine-Preventable Diseases
Report: Antibiotic Resistance Threats in the United States, 2019
CDC
Global
Current PCV introduction status of countries worldwide
Pneumonia in children fact sheet
WHO
Position paper on pneumococcal conjugate vaccine for childhood immunization
WHO
