Key points
- Some Streptococcus pneumoniae isolates are resistant to one or more antibiotics.
- S. pneumoniae resistance can lead to treatment failures.
- Vaccination helps prevent resistant pneumococcal infections.

Trends
How common antibiotic-resistant S. pneumoniae is varies throughout the United States.
Today, S. pneumoniae resistant to at least one antibiotic causes more than 2 in 5 infections. New pneumococcal vaccines will be critical as the proportion of resistance to some important antibiotics continues to increase.
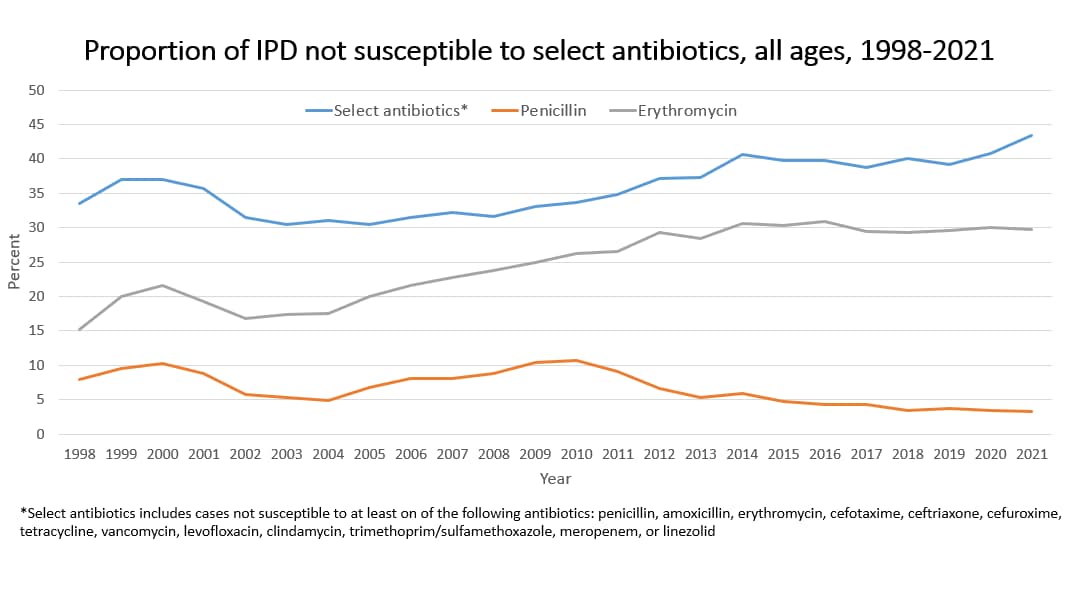
The proportion of IPD not susceptible to select antibiotics has remained relatively steady over time.
Threats report
CDC's Antibiotic Resistance Threats in the United States, 2019 identifies antibiotic-resistant S. pneumoniae as a serious threat. The report includes the latest national death and infection estimates that underscore the continued threat of antimicrobial resistance.
Vaccine impact
Pneumococcal vaccines provide serotype-specific protection. Pneumococcal conjugate vaccines (PCVs) include protection against serotypes that cause the majority of antibiotic-resistant invasive pneumococcal disease (IPD). As a result, introduction of PCVs caused a significant reduction in resistant IPD in the United States.
The number of antibiotic-nonsusceptible IPD cases also decreased greatly following a change in definition of non-susceptibility (resistance) to penicillin in 2008.
PCVs have reduced pneumococcal infections caused by vaccine serotypes, most of which were resistant to antibiotics. Invasive pneumococcal infections caused by vaccine serotypes have decreased by 90% in children and 60% in adults.
Before 2000: Seven serotypes caused most antibiotic-resistant S. pneumoniae in the United States. They were 6A, 6B, 9V, 14, 19A, 19F, and 23F. Rates of disease caused by these serotypes (except 19A) decreased after the introduction of PCV7. PCV7 included six of the seven (not 19A) serotypes.
Between 2000 and 2010: Rates of disease and antibiotic-resistant S. pneumoniae caused by serotype 19A increased. However, rates of disease caused by serotype 19A have greatly decreased since then due to use of PCV13 (includes 19A). No new serotype causing most antibiotic-resistant IPD has emerged in its place in the United States.
The impact PCV15, PCV20, and PCV21 will have on antibiotic-resistant pneumococcal serotypes is yet to be determined.
Surveillance
CDC uses U.S. surveillance data to estimate how many cases of invasive pneumococcal disease (including resistant cases) occur each year.
Several private-sector systems also track antibiotic-resistant S. pneumoniae.
Outbreaks
State and local health departments have reported outbreaks of antibiotic-resistant S. pneumoniae in long-term care settings and childcare centers.
Risk groups
People with pneumococcal infections who recently used antibiotics are more likely to have a resistant infection than those who haven't.
People who attend or work at childcare centers are at increased risk for infection with antibiotic-resistant S. pneumoniae.
Other risk factors for having a resistant S. pneumoniae infection include hospitalization and immunosuppression.
Costs
Antibiotic-resistant S. pneumoniae is associated with increased costs compared to infections caused by non-resistant (susceptible) pneumococcus. This is because of
- More expensive antibiotics needed
- Costs associated with antibiotic drug development
- Surveillance costs to track resistance patterns
- Repeat disease due to treatment failures
- Educational requirements for patients, clinicians, and microbiologists
Challenges and opportunities
Challenges
There are several factors that create challenges for preventing emerging antibiotic resistance of pneumococcus, including:
- Unnecessary use of antibiotics
- Nonuniversal adoption of standard methods (CLSI guidelines) to identify and define antibiotic-resistant S. pneumoniae
- Spread of resistant serotypes
- Lack of a vaccine that can protect against all serotypes of pneumococcus
Opportunities
Improving appropriate antibiotic use and expanding use of pneumococcal vaccines may slow or reverse emerging antibiotic resistance. Expanded use of recommended vaccines could also prevent more infections.
