Key points
- Heroin is a highly addictive, dangerous opioid drug.
- Using heroin with other drugs or alcohol increases the risk of an overdose, which can lead to coma or death.
- After rising steadily beginning in 2010, the rate of heroin overdose deaths has been decreasing since 2018.
What is heroin?
Heroin is a highly addictive, illegal opioid drug. The seed pods of opium poppy plants make morphine, which is used to create heroin. It is considered highly addictive because all the ways of taking heroin flood the brain very quickly.1
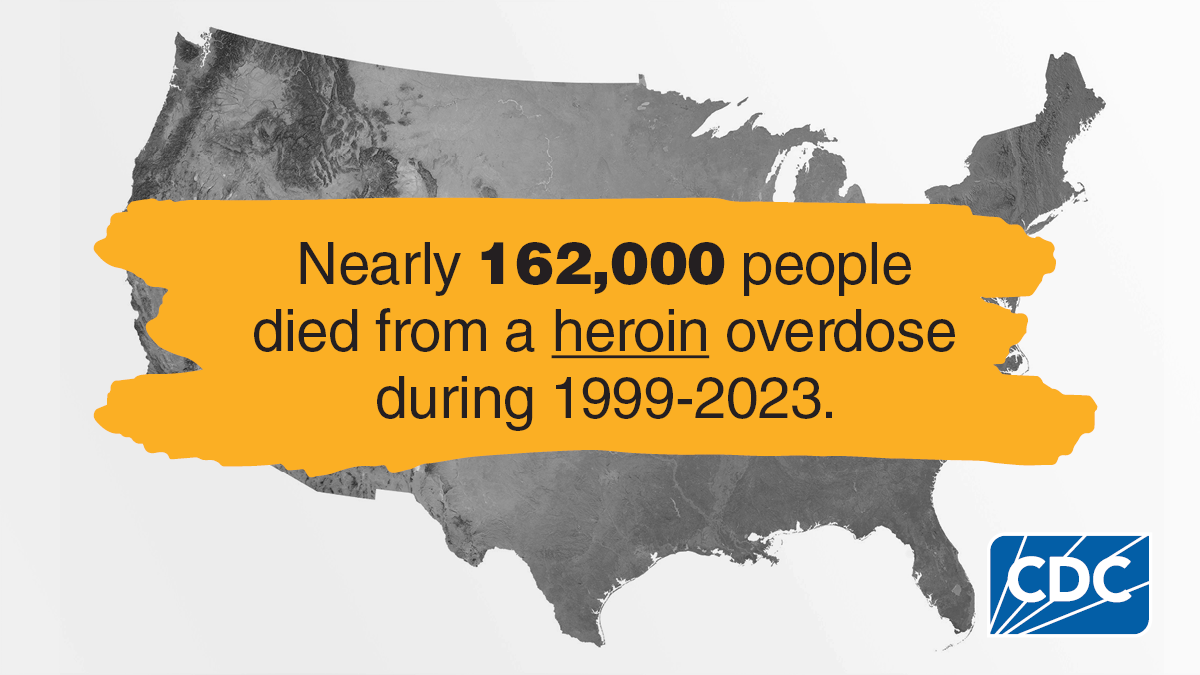
Rates of overdose deaths involving heroin
Approximately 5% of all opioid overdose deaths in 2023 involved heroin,2 while nearly 92% involved synthetic opioids - mainly illegally made fentanyl (IMF) and fentanyl analogs. Heroin has largely been replaced by IMF in the illegal drug supply and most heroin now available in the United States is combined with IMF.3
From 2022 to 2023, the heroin overdose death rate decreased approximately 33%.2 Factors that may contribute to the decrease in heroin-involved deaths include fewer people initiating heroin use and shifts from a heroin-based market to a fentanyl-based market.45
Learn more about Fentanyl Facts
How is heroin harmful?
Heroin can be injected, smoked, and snorted. People who inject drugs are also at risk of getting serious, long-term viral infections such as HIV, Hepatitis C, and Hepatitis B, as well as bacterial infections of the skin, bloodstream, and heart (endocarditis).6789
Repeated use of heroin can lead to tolerance. Opioid tolerance occurs when a person using opioids begins to experience a reduced response to medication or a drug, requiring more opioids to experience the same effect. At higher doses over time, the body can experience opioid dependence. If someone who is dependent on heroin stops using it, they can have withdrawal symptoms.
Risks of Opioid Use Disorder (OUD) and Overdose
Opioid Use Disorder (OUD), often known as addiction, is a problematic pattern of opioid use that causes significant impairment or distress. OUD is considered a medical condition that can affect anyone. Repeated use of heroin can lead to an OUD. This is more than physical dependence and it is a chronic (long-lasting) brain disorder.
A diagnosis is based on specific criteria such as unsuccessful efforts to cut down or control use, or use resulting in social problems and a failure to fulfill obligations at work, school, or home, among other criteria.
Like many other medical conditions, evidence-based treatments are available for OUD, but seeking treatment remains stigmatized. Stigma can be a major barrier to how well prevention and treatment programs work against the opioid crisis.
A heroin overdose can cause slow and shallow breathing, coma, and death. People often use heroin along with other drugs or alcohol. This practice is especially dangerous because it increases the risk of overdose.
Reversing an opioid overdose
Naloxone is a safe medication that can quickly reverse an overdose from opioids like heroin if it is given in time. It works by blocking the effects of the opioid on the body. Start by administering one dose of naloxone and wait 2-3 minutes to see if normal breathing returns before giving a second dose. Giving more than one dose of naloxone may not be necessary. It can restore normal breathing within 2 to 3 minutes in a person whose breath has slowed, or even stopped, as a result of opioid overdose. Naloxone won't harm someone if they're overdosing on drugs other than opioids, so it's always best to use it if you think someone is overdosing.
There are two forms of naloxone, (pre-filled nasal spray and injectable) that anyone can use without medical training or authorization. Naloxone is easy to use and small to carry. People at risk of an overdose are encouraged to carry naloxone with them. You can buy naloxone over the counter at a pharmacy.
OUD Treatment
Treatments for OUD include medicines to treat withdrawal symptoms, medicine to block the effects of opioids, and behavioral treatments.
OUD treatment can vary depending on the patient's individual needs, occur in a variety of settings, take many different forms, and last for varying lengths of time.
Evidence-based approaches to treating OUD include medications sometimes used in combination with behavioral therapy. People getting treatment for OUD can talk to their health care provider to come up with a treatment plan that fits their needs. A recovery plan that includes medication for opioid use disorder increases the chance of success.5
- Fareed A, Kim J, Ketchen B, Kwak WJ, Wang D, Shongo-Hiango H, Drexler K. Effect of heroin use on changes of brain functions as measured by functional magnetic resonance imaging, a systematic review. Journal of addictive diseases. 2017 Apr 3;36(2):105-16
- Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2003–2023. NCHS Data Brief, no 522. Hyattsville, MD: National Center for Health Statistics. 2024. DOI: https://dx.doi.org/10.15620/cdc/170565.
- Department of Justice, Drug Enforcement Administration. 2024 national drug threat assessment. Washington, DC. 2024.
- Substance Abuse and Mental Health Services Administration. (2024). Key substance use and mental health indicators in the United States: Results from the 2023 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/release/2023-national-survey-drug-use-and-health-nsduh-releases
- Substance Abuse and Mental Health Services Administration. Overdose Prevention and Response Toolkit.
- Des Jarlais DC, Kerr T, Carrieri P, Feelemyer J, Arasteh K. HIV infection among persons who inject drugs: ending old epidemics and addressing new outbreaks. AIDS 2016; 30:815–26.
- Degenhardt L, Charlson F, Stanaway J, et al. Estimating the burden of disease attributable to injecting drug use as a risk factor for HIV, hepatitis C, and hepatitis B: findings from the Global Burden of Disease Study 2013. Lancet Infect Dis 2016; 16:1385–98.
- McCarthy NL, Baggs J, See I, et al. Bacterial infections associated with substance use disorders, large cohort of United States hospitals, 2012–2017 [manuscript published online ahead of print 7 January 2020]. Clin Infect Dis 2020; ciaa008. doi:10.1093/cid/ciaa008.
- Larney S, Peacock A, Mathers BM, Hickman M, Degenhardt L. A systematic review of injecting-related injury and disease among people who inject drugs. Drug Alcohol Depend 2017; 171:39–49
