The David J. Sencer CDC Museum will re-open with new visitation protocols on January 2nd, 2026. All visitors must make advanced reservations. Walk-in visits are no longer permitted.
The following information is required while making reservations:
- Visitors to provide first, middle, and last name
Visitors 18 and over will also need to submit:
- Date of birth
- Citizenship (Select U.S. or non-U.S. citizen)
- Government-issued valid (not expired) REAL ID number or passport number
Bring confirmation email(s) for museum visit.
Teen Newsletter: Women’s Health
October 2022
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each newsletter focuses on a different public health topic that CDC studies. Newsletter sections include: Introduction, CDC’s Work, The Public Health Approach, Out of the CDC Museum Collection, and Teen Talk.
Women’s health is an important topic when examining public health as a whole. According to the U.S. Census, roughly 51% of the U.S. population are women. In this month’s newsletter, we will examine health topics that disproportionately or uniquely affect women and girls.
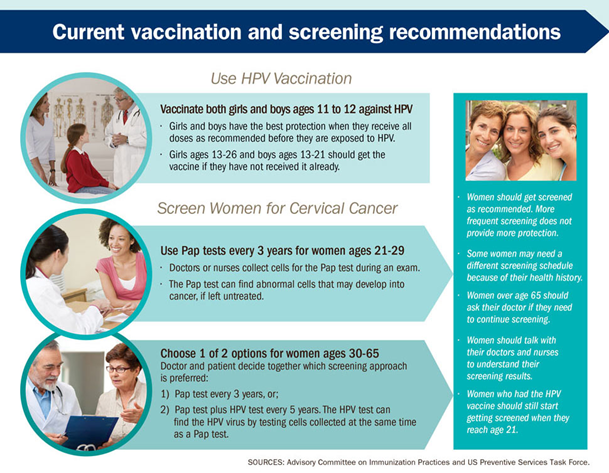
Cervical cancer is the fourth most common cancer in women worldwide. Cervical cancer is a preventable and curable disease if detected early and managed effectively. While all women are at risk for cervical cancer, data show it occurs most often in women over the age of 30. Black and Hispanic women experience higher rates of HPV-associated cervical cancer than women of other races and ethnicities. Check out the Teen Newsletter about HPV to learn more about human papillomavirus.
Many health issues uniquely affect the organs and tissues of the female reproductive system.
- Endometriosis is when the kind of tissue that normally lines the uterus grows somewhere else, like on the ovaries or behind the uterus. This “misplaced” tissue can cause pain, infertility, and heavy periods.
- Polycystic ovary syndrome (PCOS) occurs when a woman’s ovaries or adrenal glands produce more male hormones than normal. One result is when fluid-filled sacs called cysts develop on the ovaries. Symptoms may include infertility, pelvic pain, or irregular menstrual periods.
- Uterine fibroids are the most common noncancerous tumors in women of childbearing age. Fibroids are masses of muscle cells and other tissues that grow in and around the wall of the uterus. Symptoms of fibroids include heavy or painful periods, bleeding between periods, and other reproductive problems, such as infertility, multiple miscarriages, or early labor. While these symptoms can be helpful indicators, some women will have no symptoms, which is why it is important to see your health care provider for routine exams.
In addition to reproductive health issues that impact women, there are other health concerns that disproportionately affect women, including but not limited to:
- Depression – A CDC study shows that about one 1 out of 10 women in the U.S. reported symptoms of depression in the last year. Women were almost twice as likely as men to have had depression. Furthermore, CDC’s Pregnancy Risk Assessment Monitoring System (PRAMS) shows that nationally about 1 in 8 women experience symptoms of postpartum depression.
- Intimate Partner Violence (IPV) – IPV is a significant public health issue that disproportionately affects women. About 35% of female IPV survivors experience some form of physical injury. Other negative health outcomes associated with IPV include a range of conditions affecting the heart, digestion, reproduction, and nervous system. Survivors can experience mental health problems such as depression and post-traumatic stress disorder (PTSD). Women from racial and ethnic minority groups and women with disabilities are more likely to experience IPV and are at higher risk for worse consequences. Learn more about IPV amongst young people in the Teen Newsletter about teen dating violence.
CDC’s Office of Women’s Health (OWH) serves as a central point for women’s health and raises visibility of risk factors and other conditions that impact women and girls’ health. This office reports data, disseminates research, and sets goals for prevention, research, education, and policy development.
CDC’s Office of Health Equity (OHE) advances health equity and women’s health issues across the nation through CDC’s science and programs. One of OHE’s priorities is to focus on solutions for reducing health disparities, improving women’s health, and ensuring a diverse and inclusive public health workforce.
CDC’s Division of Cancer Prevention and Control (DCPC) leads CDC’s efforts in preventing and detecting cancers early and improving the overall health of cancer survivors. DCPC seeks to educate the public on prevention methods, like receiving the HPV vaccination, receiving the PAP and HPV screening tests, and practicing safe sex.
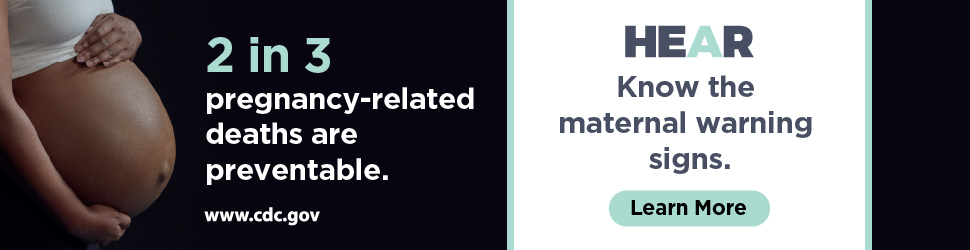
CDC’s Division of Reproductive Health (DRH) is committed to healthy pregnancies and deliveries for every woman. The Hear Her campaign supports CDC’s efforts to prevent pregnancy-related deaths by sharing potentially life-saving messages about urgent warning signs. You’ll learn more about this campaign below.
CDC’s Division of Violence Prevention (DVP) is committed to stopping violence before it begins. Teen dating violence is common. Nearly 1 in 11 women reports having experienced physical dating violence in the last year. To learn more, check out this Newsletter on Teen Dating Violence.
Overall, the CDC works collaboratively to address the various public health issues that disproportionately or uniquely affect women and girls.
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
In this month’s newsletter, we will look at the topic of maternal mortality to illustrate the four steps of the public health approach.
Each year in the U.S., about 700 people die during pregnancy or in the year after. Another 50,000 women each year experience severe pregnancy complications that can cause serious consequences for a woman’s health. Every pregnancy-related death is tragic, especially considering that 2 out of 3 are preventable. Recognizing the warning signs and providing timely treatment and quality care can prevent many pregnancy-related deaths.
- Surveillance (What is the problem?). In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
Through the , CDC conducts national pregnancy-related mortality surveillance to better understand the risk factors for and causes of pregnancy-related deaths in the U.S.
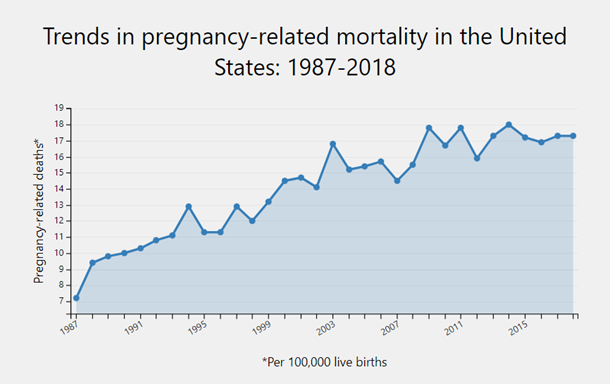
Since the PMSS was implemented, the number of reported pregnancy-related deaths in the U.S. steadily increased from 7.2 deaths per 100,000 live births in 1987 to 17.3 deaths per 100,000 live births in 2018. The graph above shows trends in pregnancy-related mortality ratios between 1987 and 2018 (the latest available year of data).
- Risk Factor Identification (What is the cause?). After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to diseases, such as something in the environment or certain behaviors that people are practicing?
Many factors influence pregnancy-related health outcomes. It is important for all women of reproductive age to adopt healthy lifestyles (e.g., maintain a healthy diet and weight, be physically active, quit all substance use, prevent injuries) and address any health problems before getting pregnant.
A healthy pregnancy begins before conception and continues with prenatal care, along with early recognition and management of complications if they arise. Health care providers can help women prepare for pregnancy and for any potential problems during pregnancy. Early initiation of prenatal care by pregnant women, and continuous monitoring of pregnancy by health providers, are key to helping to prevent and treat severe pregnancy-related complications.
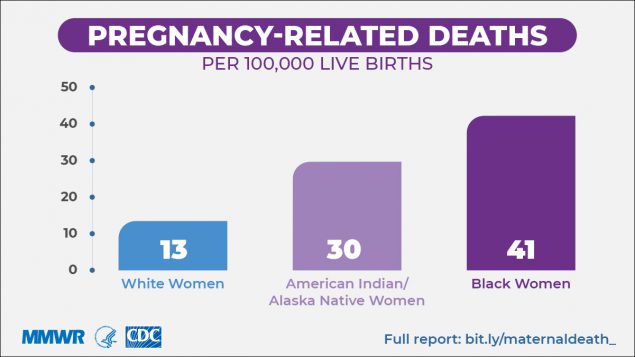
One major disparity in pregnancy-related death is race. Black women are three times more likely to die from a pregnancy-related cause than White women. Multiple factors contribute to these disparities, such as variation in quality health care, underlying chronic conditions, structural racism, and implicit bias. These factors prevent many people from racial and ethnic minority groups from having fair opportunities for economic, physical, and emotional health.
- Intervention Evaluation (What works?). Once we’ve identified the risk factors related to the problem, we ask, “What intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
Complications of pregnancy are health problems that occur during pregnancy. They can involve the mother’s health, the baby’s health, or both. Some women have health problems that arise during pregnancy, and other women have health problems before they become pregnant that could lead to complications. It is very important for women to receive health care before and during pregnancy to identify and decrease the risk of pregnancy complications.
Small advances in preventing pregnancy-related complications can improve the quality of life for thousands of pregnant women. Pregnancy symptoms and complications can range from mild and annoying discomforts to severe, sometimes life-threatening, illnesses. Some of these complications include:
- Anemia – When the number of healthy red blood cells is less than normal, anemia may occur. Women with pregnancy-related anemia may feel tired and weak. Anemia can be helped by taking iron and folic acid supplements.
- High blood pressure – Chronic poorly-controlled high blood pressure before and during pregnancy puts a pregnant woman and her baby at risk for problems. It is associated with an increased risk for maternal complications such as preeclampsia, placental abruption (when the placenta separates from the wall of the uterus), and gestational diabetes.
- Obesity – Overweight and obese women who lose weight before pregnancy are likely to have healthier pregnancies. Obesity is associated with an increased use of health care and physician services and longer hospital stays for delivery.
- Depression – Some women experience depression during or after pregnancy. Depression that persists during pregnancy can make it hard for a woman to care for herself and her unborn baby.
- Avoiding harmful infections – During pregnancy, the baby is protected from many illnesses, but some infections can still be harmful. Easy steps, such as hand washing and avoiding certain foods, can help protect from some infections.
- Implementation (How did we do it?). In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
Recognizing urgent maternal warning signs and getting an accurate and timely diagnosis can save lives during pregnancy and up to a year after delivery.
The CDC’s Hear Her campaign encourages women’s partners, friends, family, and health care providers to listen to their concerns and engage in important conversations with them. The campaign features compelling personal stories from women of diverse backgrounds who experienced severe pregnancy-related complications. The program’s audience is women who have recently given birth and health care providers who frequently interact with pregnant women.
The campaign’s objectives are to:
- Increase awareness of serious pregnancy-related complications and their warning signs.
- Empower women to speak up and raise concerns.
- Encourage women’s support systems to engage in important conversations with them.
- Provide tools for women and providers to better engage in life-saving conversations.
“Listening and taking seriously the concerns of pregnant and postpartum women is a simple, yet powerful action that can save lives,” said Wanda Barfield, M.D., M.P.H., director of CDC’s Division of Reproductive Health at the National Center for Chronic Disease Prevention and Health Promotion. “Women know their bodies and can often tell when something is not right. We hope Hear Her will help people recognize maternal warning signs and quickly get the care women need.”
Using The Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
This month’s Out of the CDC Museum Collection features women’s menstrual products that were linked to toxic-shock syndrome


The front and back of a box of Rely tampons, which were sold in the 1970s and later linked to toxic-shock syndrome.
Rely was a brand of superabsorbent tampons made by Procter & Gamble starting in 1975 that was later linked to Toxic Shock Syndrome. This predated 1976 changes the FDA and the Medical Device Amendments implemented that would re-categorize menstrual products as medical devices that would require rigorous testing and pre-approval by the FDA.
Now, before any tampons can be legally sold in the U.S., they must go through the FDA’s review to determine whether they are as safe and effective as (substantially equivalent to) legally marketed tampons.