At a glance
This guidance is intended for panel physicians conducting overseas health assessments for U.S.-bound refugees and is provided by CDC to support safe travel and healthy resettlement for U.S.-bound refugees. It focuses on supplemental activities unique to refugee medical exams, including vaccination guidance, presumptive treatment for intestinal helminths, pre-travel preparation for refugees with significant medical conditions, and related processes to ensure travel fitness. The data from the overseas health assessments is transmitted to CDC who then transmits the data to the U.S. states receiving the arriving refugees. Overseas documentation of health information by panel physicians ensures continuity of care for persons with medical conditions and helps facilitate their placement in the United States. In most circumstances the International Organization for Migration (IOM) organizes travel for U.S.-bound refugees on behalf of the U.S. government, including those with medical conditions. Please note that the "Pre-embarkation (Fitness-to-travel) Check" and "Guidance for Overseas Medical Examinations for Refugees with Significant Medical Conditions" sections of this guidance apply primarily to situations in which IOM, or another agency coordinating medical movement for refugees, is organizing travel for refugees.
Attention
This is a companion page to: Guidance for Overseas Medical Examinations for Refugees with Significant Medical Conditions.
Introduction
The U.S. Refugee Admissions Program (USRAP) is a program to assist refugees applying for U.S. resettlement and is managed by the Department of State in cooperation with the Department of Homeland Security and Department of Health and Human Services (HHS).
Like immigrants, U.S.-bound refugees are required to receive an overseas Health Assessment (HA) following CDC Technical Instructions for the Panel Physicians. CDC, together with the Department of State, also supports additional health interventions, such as vaccination, presumptive parasite treatment, and activities to assess and support travel fitness.
This Supplemental Guidance is intended for panel physicians conducting overseas health assessments for refugees, defined as individuals receiving refugee benefits under USRAP who may also include a small number of individuals holding V93 "follow to join" or other visa types.
Notice
This guidance describes additional interventions for U.S.-bound refugees, how to document and transmit refugee health information, and how to coordinate with agencies facilitating refugee travel (e.g., IOM). When examining U.S.-bound refugees, panel physicians should refer to this guidance and the supporting documents in the "Resources, Job Aids, and Forms" section at the bottom of this page in addition to CDC Technical Instructions for Panel Physicians.
Differences in the health assessment process for U.S.-bound refugees and immigrants
Some aspects of the health assessment process for refugees are different than the process for immigrants. While panel physicians should use the same CDC Technical Instructions for both immigrant and refugee medical examinations, the vaccination schedule for U.S.-bound refugees differs from the immigrant schedule. For refugees, panel physicians should also assess resettlement medical needs and conduct (when requested by the CDC and the agency arranging refugee travel) pre-departure evaluation and pre-embarkation checks; in contrast, these items are not part of the medical process for immigrants.
| Activity | Immigrants | Refugees and V93s |
|---|---|---|
| Overseas medical examination | Follow CDC Technical Instructions (TIs)* | Follow CDC Technical Instructions (TIs)* |
| Data entry | Use eMedical1 for data management | Use MiMOSA2,** for data management |
| Vaccination | Follow CDC Technical Instructions (TIs)* | Follow USRAP Vaccination Schedule |
1 eMedical is an online platform for managing medical examinations for visa applications
2 MiMOSA IAP (Migrant Management Operational Systems Application) is IOM's tool for managing biographical, demographic, medical, and movement information on refugees and other migrating populations
Additional health guidance and forms specific to U.S.-bound refugees
The information below does not apply to immigrants.
| Activity | Guidance and forms |
| Resettlement needs assessment | Significant Medical Condition (SMC) guidance |
| Transmit Medical forms to IOM | Department of State medical form (DS), SMC, activities of daily living (ADL) form as applicable |
| Significant medical condition (SMC) Referrals and Follow-Up | Significant Medical Condition (SMC) guidance |
Pre-departure and post-arrival health activities specific to U.S.-bound refugees
The activities below do not apply to immigrants.
| Activity | Timeline |
| Health Assessment | Within 2 - 3 months before departure |
| Pre-Departure Evaluation (PDE) | Within 1–3 weeks prior to departure |
| Pre-Embarkation Check
(PEC) |
Within 24-72 hours before departure |
| Complete pre-departure medical procedures (PDMP) form | Within 24-72 hours before departure |
| Recommend domestic medical examination, organized by receiving state | Within 90 days after arrival |
The Refugee Health Process During Resettlement
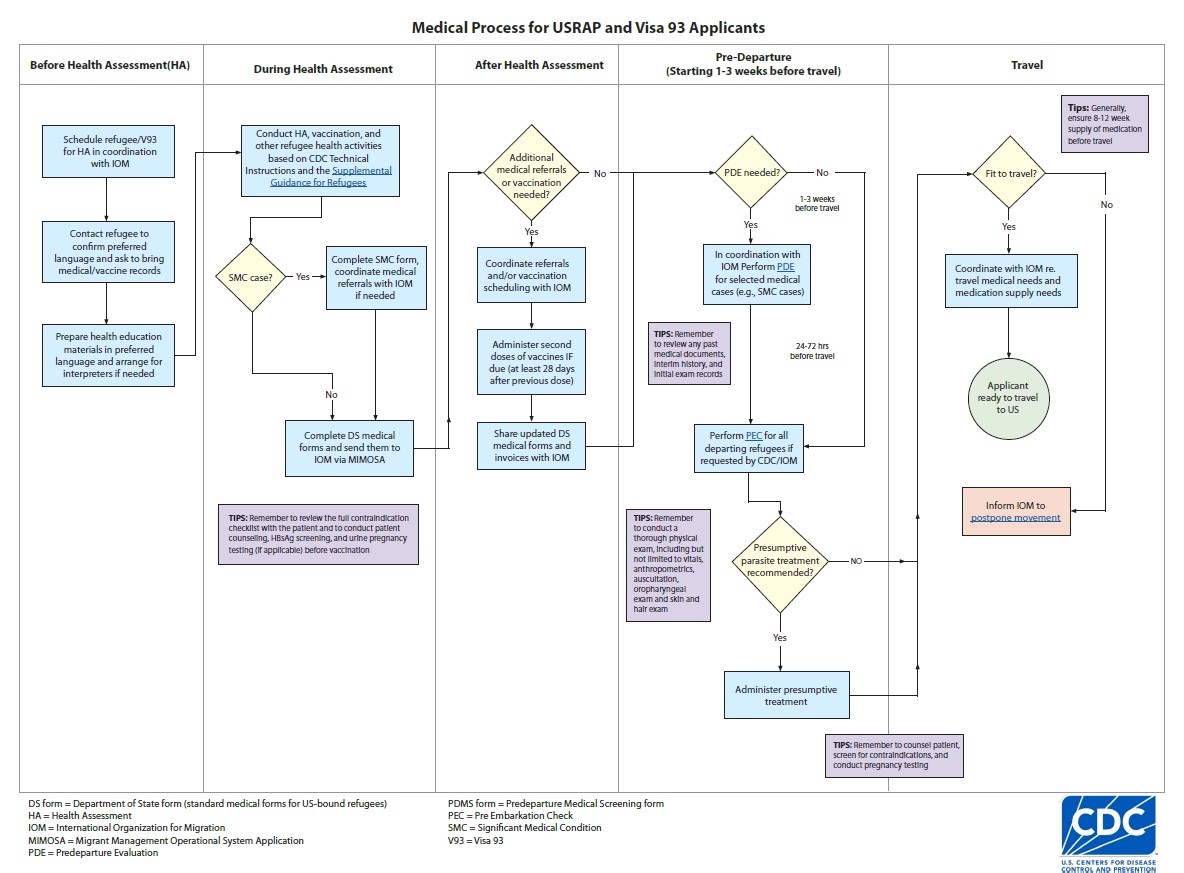
The refugee health process for U.S.-bound refugees generally lasts about 3-4 months but can be as short as one month with expedited processing. The more information the panel site provides on the Department of State (DS) and supplementary medical forms (Significant Medical Conditions Form and Activities of Daily Living Form) the better the resettlement agencies (RAs) and receiving health providers can address the unique health needs of arriving refugee families. The job aid below outlines the medical process and responsibilities of the panel site during each step of the process. The process depends on close coordination between the panel site and IOM or the partner organizing refugee travel.
Refugee Scheduling and Data Management Process
Upon receiving requests for refugee health assessment activities from refugee support centers (RSCs), IOM staff create refugee medical records in the Migrant Management Operational System Application (MiMOSA). This is a platform for capturing and managing biographical, demographic, medical, and movement information on refugees and other migrating populations.
Once the panel physician completes the entry of the MiMOSA record, they should finalize and submit it back to IOM, along with digital x-rays in DICOM format and any other scanned medical reports.
IOM medical staff review these forms for completeness before transmitting them to the RSC. Staff submit the data to the RSC information system, which the then shares the records with resettlement agencies (RAs) responsible for the refugee allocation and placement process in the United States.
At the time of refugee travel, IOM transmits updated medical records from MiMOSA to CDC's Electronic Disease Notification (EDN) system (including all medical records from Health Assessment through PEC). The medical information is then available to U.S. resettlement agencies, health departments of jurisdiction for the refugees' U.S. destinations, and healthcare providers in those jurisdictions who conduct recommended domestic medical examinations of newly arrived refugees.
The Refugee Health Assessment
The health assessment consists of counseling, informed consent, examination (following the Technical Instructions), vaccination (following the USRAP recommended immunization schedule), and vaccination follow up. In settings where the refugees and panel site staff do not share the same language, staff should complete the process with the aid of a trained medical interpreter. Panel staff should also be trained to work effectively with medical interpreters.
The panel staff member conducting counseling should use the refugee health assessment map and the IOM counseling flipchart as resources during the counseling session.
Refugee Counseling and Consent
The first part of the health assessment (HA) process is the refugee counseling session. During this session a nurse, counselor, or health educator will orient the refugee to what they can expect during the required medical examination and explain additional health interventions offered. The purpose of this session is to allay anxieties about the health assessment and obtain voluntary informed consent for all procedures.
After answering any questions the refugees may have, the counselor should ask each refugee, or the parent or caregiver of a child less than 15 years old, if they are willing to sign an informed consent form. This is an agreement between the panel site and the refugee.
Panel site staff can request an IOM consent template to create their own clinic-specific consent form. It is important to ensure that the clinic’s consent form covers all elements of the refugee health assessment process.
Refugees who sign this consent form confirm that they have understood and agree to the required medical examination process. They also agree to any recommended, voluntary health interventions (such as vaccination and presumptive parasite treatment), and to sharing medical results with other agencies involved in their resettlement. Once the refugee signs this form, staff can begin the health assessment following the CDC Technical Instructions.
Refugee Vaccination
CDC and the Bureau of Population, Refugees, and Migration (PRM) of the U.S. Department of State co-fund a vaccination program for the United States Refugee Admissions Program (USRAP) applicants to:
- Protect U.S.-bound refugees from serious vaccine-preventable diseases
- Prevent importation of vaccine preventable diseases into the U.S.
- Limit the number of vaccinations refugees will need after their arrival in the U.S.
- Facilitate earlier school enrollment for children given that in the U.S., vaccination is often required before school enrollment.
Please see the USRAP Vaccination Job Aid for an outline of the vaccination process.
Use the section on vaccines in the IOM counseling flipchart to counsel the refugee about the recommended vaccines. After counseling, panel sites should offer all USRAP applicants age-appropriate vaccines according to the USRAP Vaccination Program Schedule and in coordination with the RSC's and the IOM team in each region.
For non-IOM Panel Sites:
Please use the abbreviated USRAP Vaccination Schedule unless specifically instructed to do otherwise by CDC/IOM. Depending on current age, medical history, and documented past vaccination history, refugees are recommended to receive one dose of one or more of the following vaccines based on the USRAP vaccination schedule (except MMR, for which two appropriately-spaced doses are recommended):
- DTP (diphtheria-tetanus-pertussis) or DTaP (diphtheria-tetanus-acellular pertussis)
- Td (tetanus-diphtheria) or Tdap
- MMR (measles-mumps-rubella) (2 doses)
- IPV (inactivated polio vaccine or bOPV (bivalent oral polio vaccine)
- Hep B (hepatitis B)
- Pentavalent (DTP-HepB-Hib [haemophilus influenzae type b]) or hexavalent (DTaP-IPV-HepB-Hib) combination vaccines
Note that for logistical, availability, or cost reasons CDC may modify this list of vaccines and the number of doses. CDC or IOM will communicate this to the panels where applicable.
CDC recommends that refugees with certain medical conditions receive additional vaccines. Please refer to the USRAP vaccination schedule for medical indications for guidance.
Important Vaccination Practices
The information below describes key practices for the USRAP refugee vaccination program.
Vaccination Storage and Supplies
- Maintain the cold chain required for vaccine storage following best storage practices from the CDC Vaccine Storage and Handling Toolkit.
- Inform your IOM point of contact (with a copy to CDC at vaccinepilot@cdc.gov) of any vaccine shortages.
- Inform your IOM point of contact (with a copy to CDC at vaccinepilot@cdc.gov) of any outbreaks of communicable diseases that are affecting or could potentially affect refugees hosted in your country.
Before Vaccination
- Ask refugees to bring their (or their children's) vaccine records with them to the clinic when scheduling the exam appointment.
- Review vaccine records carefully and document valid historical doses on the DS-3025 form.
- Enter dates of historical vaccine doses sequentially under the historical vaccine dose columns.
- Counsel refugees about the vaccines being offered (counseling) and distribute vaccine information brochures to each refugee or family (for example: IOM Vaccine Information Statements (VIS))
- Test for hepatitis B surface antigen (HBsAg) using approved test kits.
- Approved test kits include BiolineTM HBsAg, DetermineTM HBsAg2, or other World Health Organization (WHO) prequalified HBsAg test kits.
- For refugees needing re-examination (e.g., returning for a second HA): If the refugee has previously started the Hep B vaccination series and HBsAg testing was already done during the first health assessment, there is no need to repeat the testing.
- Approved test kits include BiolineTM HBsAg, DetermineTM HBsAg2, or other World Health Organization (WHO) prequalified HBsAg test kits.
- Screen each refugee for contraindications to vaccination using the USRAP immunization contraindication checklist before each vaccination session (dose 1 and dose 2 if applicable).
- Perform urine pregnancy testing for all female refugees aged 15 to 50 years before administering any doses of a live injectable vaccine (e.g., MMR/measles or other live injectable vaccines). Pregnant refugees should not receive live injectable vaccines.
During Vaccination
- Vaccinate according to the USRAP Vaccination Schedule; see vaccination job aid for more information.
- Observe refugees for 15 minutes after vaccination. Ask them to stay in the waiting room or on the premises so you can monitor for uncommon adverse events such as allergic reactions.
After Vaccination
- Document dates of all administered vaccines on the DS-3025 form in the "given by panel" column.
- Update refugee vaccination card if available.
- Provide each refugee with a copy of their vaccination record from MiMOSA.
- Refer refugees to free national/government vaccination clinics, if any vaccines on the USRAP schedule are only available by that route.
- Coordinate with IOM regarding pre-vaccination pregnancy testing for female applicants aged 15 to 50 years.
- Instruct refugees to send copies of these vaccination records to the clinic so that you can update their DS-3025 forms and share the updates with IOM.
- Ask refugees to seek medical care and to inform you in the event of any adverse events after immunization (AEFI).
- Document and report AEFI using the AEFI reporting form and send them to IOM within 48 hours of notification whenever possible.
- Contact your CDC and/or IOM counterparts with any questions.
Resettlement Health Assessment
A major purpose of the overseas health assessment is to detect, diagnose, and treat inadmissible health-related conditions, including active tuberculosis, untreated syphilis or gonorrhea, Hansen's disease, physical or mental disorders associated with harmful behaviors and substance use.
In the case of U.S.-bound refugees, another important objective is to identify refugees with significant medical conditions (SMCs) and to assess and document related resettlement, travel, and follow-up health needs. Please see section on refugees with significant medical conditions for examples of SMCs.
To meet this objective, it is crucial to obtain a complete medical history (using trained medical interpreters when needed), perform a comprehensive physical examination (PE) during Health Assessment and review available medical documents.
Refer to the adult and pediatric PE checklists for guidance regarding suggested components of the physical examination.
For refugees with SMCs, refer to this page for information on referral, documentation, and follow-up.
Pre-embarkation (Fitness-to-travel) Check
Pre-embarkation checks (PEC) are recommended for all U.S.-bound refugees within 24-72 hours before their departure for the United States. In some situations, panel physicians may be asked to conduct the PEC. IOM will communicate with you directly in those circumstances. In other situations, IOM conducts the PEC.
This check helps ensure that all refugees are fit to travel, do not have acute communicable diseases of public health concern, and arrive at their destinations in stable condition.
Health information gathered during the PEC also helps the medical team confirm that appropriate arrangements have been made for any person needing travel medical assistance or urgent follow-up after arrival.
Physicians and nursing staff should perform the following tasks while conducting a PEC:
- Review the refugee medical forms, SMC forms, and other relevant medical reports, noting any changes to the refugee's medical condition since most recent medical evaluation.
- Confirm list of current medications, dosages, and available supply (aim for 8-12 weeks); update SMC forms as needed.
- Confirm availability and functional status of any needed medical equipment (e.g., mobility aids). Make sure they are working and check to see whether the equipment or device needs batteries or a charging cable.
- Measure and review vital signs
- Assess weight of all refugees.
- Measure height/length for refugees less than 18 years old and plot or calculate weight for height or body mass index Z-score (WHX or BMIZ, depending on age; or review result calculated by MiMOSA.
- Compare these measurements to those taken at the health assessment to determine whether moderate or severe acute malnutrition is present or worsening.
- Measure oxygen saturation for all children less than 5 years old, all patients with anemia, cardiac and/or pulmonary conditions, or shortness of breath on exam; and any others as dictated by clinical judgement.
- Perform a physical examination. Be sure to check the skin, hair, and oropharynx for signs of rash/exanthem, enanthem, scabies, and lice.
- For pregnant refugees, confirm that gestational age has not surpassed the maximum allowed for travel (34 weeks and 6 days for uncomplicated singleton gestation: 32 weeks and 6 days for multiparous or complicated pregnancies).
- Provide a certificate of fitness to fly during pregnancy as appropriate.
- Counsel refugees who have specific travel and post-arrival medical needs.
- Update SMC and DS forms and include any test results, treatments, and follow-up needs.
- Share this information with IOM, informing them of any changes in clinical status and any needed travel deferrals.
- Provide presumptive treatment for parasites as appropriate.
On the same day that you conduct the PEC, document PEC findings and details about any additional investigations or treatment on the IOM Pre-departure Medical Procedures form (PDMP) and share it with IOM. You will find this form in MiMOSA IAP or as a fillable PDF.
Travel Deferrals
Notify IOM immediately about any refugees who are not fit to travel and/or who have a significant medical condition (SMC) with any of the below characteristics:
- Is unstable.
- Was not previously evaluated or identified (for example, a condition that was newly detected at PEC that will require a specialist evaluation).
- Could pose a significant risk of deterioration during flight.
In these cases, the examining panel physician should make a request to defer the refugee's travel until the condition has been evaluated and stabilized and until arrangements are made for safe travel.
Below are some examples of conditions justifying temporary travel deferral (please connect with your IOM or CDC contacts if any questions):
- Communicable disease (including recent exposures, symptoms, or positive test results)
- Anemia with hemoglobin less than 7.5 g/dl
- Thrombocytopenia with platelets <30,000 cells/uL
- Sickle cell crisis - within the last 9 days
- Myocardial infarction - within last 7 days
- Cardiac failure - decompensated
- Unstable angina pectoris
- Cerebral infarction - within last 14 days
- Deep venous thrombosis (DVT) or other thromboembolic disorders - active, acute
- Respiratory disease with breathlessness at rest or markedly poor exercise tolerance
- Fractures - unstable/untreated
- Hemorrhage - recent, gastrointestinal
- Jaw fracture with fixed wiring
- Surgery within previous 10 days, depending on type
- Acute and/or suppurative otitis media that has not been adequately treated
- Sinusitis - severe
- Pneumothorax - suspected or confirmed
- Pregnancy with gestational age 34 weeks and 6 days or above (32 weeks and 6 days if multiparous or complicated pregnancy)
- Epilepsy or seizure disorder - uncontrolled
- Psychiatric disorders - unstable, including ongoing substance abuse
- Unpredictable or aggressive behavior
- Uncontrolled pain or distress
- Condition likely to cause discomfort or offense to other passengers (e.g., open, foul-smelling wound)
- Other new, unstable, and/or previously unevaluated medical condition as dictated by clinical judgment and in consultation with your IOM and/or CDC medical point of contact
Presumptive Treatment for Parasites
CDC guidance recommends presumptive parasite treatment for refugees in some regions to decrease the prevalence of intestinal parasites and malaria among U.S.-bound refugees.
During PEC, panel physicians (or nursing staff) should offer all Middle Eastern, Asian, African, Latin American, and Caribbean refugees the following, with exceptions noted in CDC's presumptive treatment guidance:
- Pregnancy test for all female refugees aged 15 to 50 years before offering presumptive treatment
- One dose of albendazole
- One dose of ivermectin (if available/licensed in your country)
Refugees who previously lived or currently live in sub-Saharan Africa should also receive praziquantel for schistosomiasis if available (even if health assessment/medical process is done outside of sub-Saharan Africa).
Refugees departing from sub-Saharan Africa (regardless of origin) should also receive artemisinin-based combination therapy for malaria.
All presumptive treatment should be provided as directly observed therapy (e.g., all doses should be observed either by panel site staff or IOM staff) and documented on the refugees' PDMP forms. Refugees should be screened for contraindications before receiving presumptive treatment.
Medical documentation for U.S-Bound Refugees
In addition to standard documentation of physical exam and testing results, be sure to document:
- Additional tests done for refugees at the time of the health assessment. This could include HBsAg, pregnancy tests, hemoglobin, oxygen saturation, etc.
- Immunizations, including both valid historical and panel-provided vaccines, and any vaccination-related remarks
- Document on the DS-3025 form
- PEC exam findings and presumptive treatment
- Document on the PDMP forms
- Significant medical conditions
- Document using the SMC and ADL forms.
Administrative Items
At the request of the PRM and CDC and, in the case of V93 applicants, in close coordination with U.S. embassies, IOM reimburses panel physicians for medical examinations, vaccination, and presumptive treatment costs upon receipt of invoices and supporting documents. Reimbursement is completed in accordance with the U.S. Embassy contact. When IOM is engaged in the medical movement of a group of refugees, detailed reimbursement information will be provided by IOM. In most circumstances, refugees should not be charged with any upfront costs or fees for the medical services. Further, any services offered which are outside the scope of this supplemental guidance must be pre-approved by the reimbursing agency/entity. Please connect with your IOM point of contact for specific arrangements.
Table 1: Abbreviation Key
U.S. Department of Homeland Security
U.S. Department of State
International Organization for Migration, the United Nations Migration Agency
IOM Migrant Management Operational System Application
Pre-embarkation Check / Fitness to Travel
Bureau of Population, Refugees and Migration, within DOS
Resettlement support centers***
U.S. Citizenship and Immigration Services, within DHS
United States Refugee Admissions Program
*Panel physicians are medical doctors appointed by the local U.S. embassy or consulate to perform immigration medical examinations for immigrants and/or refugees bound for the United States.
**Resettlement agencies are U.S. domestic agencies providing initial support to refugees upon arrival, including coordinating their health care.
***Resettlement support centers are overseas entities coordinating USRAP refugee resettlement activities
Resources, Job Aids, and Forms
Several of the USRAP resources below link to the International Organization for Migration. The audience for whom these links are intended will have access to the IOM pages. Should you have permissions but have trouble accessing any of them please contact: mhddpt@iom.int.
- The medical process of U.S.-bound refugees
- Vaccination for U.S.-bound refugees
- CDC Vaccine Storage and Handling Toolkit
- The Pre-embarkation check (PEC)
- CDC Guidelines for Overseas Presumptive Treatment of Strongyloidiasis, Schistosomiasis, and Soil- Transmitted Helminth Infections
- CDC Overseas Refugee Health Guidelines: Malaria
- IATA Medical Manual 12th Edition (2020)
- USRAP fillable SMC form
- USRAP fillable ADL form
- USRAP abbreviated vaccination schedule
- USRAP vaccination guidance for medical indications
- USRAP Hepatitis B testing protocol
- USRAP immunization contraindication checklist
- USRAP AEFI reporting form
- Vaccine Information Statements
- Refugee counseling flip chart
- Counseling brochure for pregnant refugees
- Hepatitis B counseling brochure
- USRAP refugee health counseling videos
- Significant Medical Conditions Guidance
- WHO MUAC malnutrition tables
