Key points
- Viruses that cause VHFs can be transmitted in postmortem care settings through unsafe handling of remains.
- Safely handle human remains by properly using personal protective equipment (PPE) and specific body bags, and by following decontamination measures at every step of the process.
- Only trained personnel wearing recommended PPE should touch or move any human remains from a person who has died from VHFs.
Summary of recommendations
This guidance refers only to the following viral hemorrhagic fevers: Ebola, Marburg, Lassa, Crimean Congo Hemorrhagic Fever (CCHF) and the South American Hemorrhagic Fevers (i.e., those caused by Junin, Machupo, Chapare, Guanarito and Sabia viruses). Refer to the pathogen-specific pages for further information about the individual pathogens (e.g., signs and symptoms, incubation periods, routes of transmission, diagnosis, treatments).
When handling the body of a person who has died from VHFs:
- Do not wash or clean the body.
- Do not embalm the body.
- Do not perform an autopsy unless it is absolutely necessary. If an autopsy is necessary, consult the state health department and CDC regarding necessary precautions.
- Do not remove any inserted medical equipment from the body such as intravenous (IV) lines, endotracheal or other tubing, or implanted electronic medical devices.
- Cremate the body. If cremation cannot be done because of safety concerns, the body should be buried in a standard metal casket or other comparable burial method.
If a hospital has a patient with VHF, contaminated and clean zones should already be established. Therefore, hospitals with a VHF-related death should be familiar with the following terminology.
Contaminated area: Areas that may contain VHF viruses, including the patient treatment room. Only workers wearing PPE that conforms to CDC guidance are allowed to be in a contaminated area.
Decontamination area: Area directly accessible to the contaminated area. Workers will perform final decontamination in the decontamination area before passing the human remains to the clean area.
Clean area: Noncontaminated area used for planning and staging. Only workers who have not entered the contaminated area or who have properly doffed their PPE after being in the contaminated area are permitted in the clean area. Workers put on clean PPE in the clean area under the direction of a trained observer.
Cremation: The act of reducing human remains to ash by intense heat.
Leakproof bag: Body bag that is puncture-resistant and sealed in a manner to contain all contents and prevent leakage of fluids during handling, transport, or shipping.
Recommendation details
The following equipment should be used in the contaminated area:
- Hospital gurney containing three pre-opened cremation-compatible body bags with the following specifications
- First bag (top layer on gurney): vinyl or other chlorine-free material, minimum of 6 mil thickness (152 micrometers). To prevent any leakage of fluids, all seams should be factory heat-sealed or welded, not sewn, and the zipper should be on top.
- Second bag (middle layer on gurney): chlorine-free material impervious to fluids that can be heat-sealed around the body to form a leakproof body bag. This bag should be specifically designed for the containment and transport of infectious human remains. The material should be precut to provide sufficient material to envelop the body and the first bag.
- Third bag (bottom layer on gurney): laminated vinyl or other chlorine-free material, minimum of 18 mil thickness (457 micrometers) with handles that are not sewn on, such as riveted handles reinforced with handle straps that run under the pouch. To prevent any leakage of fluids, all seams should be factory heat-sealed or welded, not sewn, and the zipper should be on top.
- First bag (top layer on gurney): vinyl or other chlorine-free material, minimum of 6 mil thickness (152 micrometers). To prevent any leakage of fluids, all seams should be factory heat-sealed or welded, not sewn, and the zipper should be on top.
- Thermal sealer for sealing the second bag
- PPE recommended for personnel entering the room of a patient with VHFs as described in CDC's PPE guidance
- Safety-tipped trauma shears for cutting excess material from heat-sealed bag
- Device capable of taking and securely transferring photographs electronically via Wi-Fi, e-mail, or text message (such as a digital camera or mobile phone)
- Environmental Protection Agency (EPA)-registered hospital disinfectant and wipes from List L or List Q
- Alcohol-based hand rub (ABHR)
- Red biohazard bag for medical waste
- Zip tie for locking the third bag shut at the zipper
The following equipment should be used in the clean area:
- Hospital gurney or mortuary stretcher
- Adhesive-backed pouch that is applied to the decontaminated body bag
- Single-use (disposable) gloves with extended cuffs and a long-sleeved disposable gown
- Biohazard spill kit, which should include:
- Recommended PPE
- Absorbent materials such as paper towels
- Kitty litter or a solidifier
- An EPA-registered hospital disinfectant from List L or List Q
- Biohazard waste bags
- Recommended PPE
- Infectious substance labels to be applied to the decontaminated body bag. These include the following:
- Black and white "infectious substance" label
- United Nations (UN) 2814 label
- "Do not open" label
- Name and phone number of the hospital administrator
- Black and white "infectious substance" label
Important considerations
- Ensure that workers handling the body and the trained observer wear recommended PPE and follow all procedures in CDC's PPE guidance.
- Follow the cleaning and disinfecting recommendations found in CDC's environmental infection control guidance. According to this guidance, PPE surfaces, equipment, and patient care area surfaces that become visibly soiled should be decontaminated immediately. Use an EPA-Registered hospital disinfectant from List L or List Q, with a label claim for use against a nonenveloped virus.
- Place all waste produced during postmortem preparation and decontamination into red biohazard bags in the contaminated area, following the CDC guidelines for handling VHF-associated waste.
The number of workers needed for this process will be determined by the size and weight of the body being prepared and the ability of the workers to lift the body and assist with managing the body bag. For the death of an average size adult, for example, this process should be performed by a minimum of three healthcare workers or other workers properly trained in handling infectious bodies: two to lift the body and one to hold the body bag open.
CDC recommends posting an enlarged copy of job aid that includes the following step-by-step guidelines in the contaminated area. The workers should read the guidelines aloud as they perform each step of the procedure.
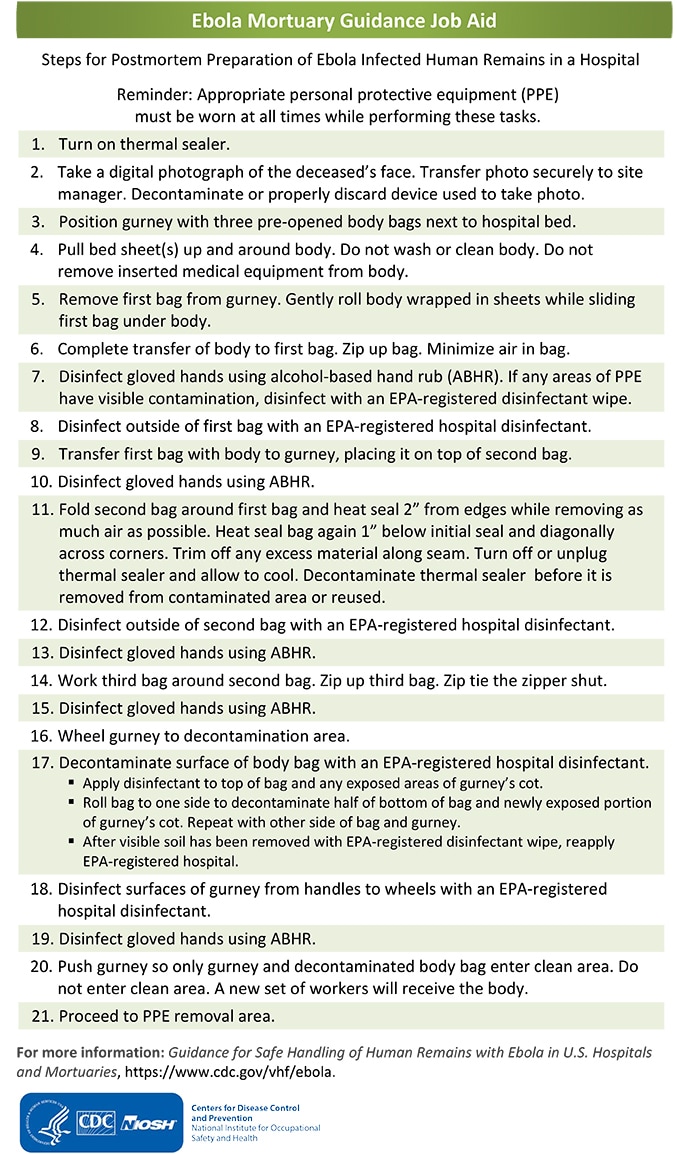
- Turn on the thermal sealer to allow it to warm up during the initial preparation of the body. This sealer will be used to seal the second body bag.
- Use the camera or other device to take a photograph of the decedent's face for identification purposes. The photograph should be securely transferred electronically to the pre-identified site manager. The device must be decontaminated before being removed from the contaminated area or reused. If not decontaminated, the device should be discarded along with other medical waste.
- Position the gurney with the three pre-opened body bags next to the hospital bed with the body.
- Pull the bed sheet(s) that are under the body up and around the front of the body. Do not wash or clean the body. Do not remove any inserted medical equipment such as IV lines or endotracheal or other tubing from the body.
- Remove the first bag from the gurney. Gently roll the body wrapped in sheets while sliding the first bag under the body.
- Complete the transfer of the body wrapped in sheets to the first bag and zip up the bag. Minimize the amount of air trapped in the bag while zipping.
- Disinfect gloved hands using ABHR. If any areas of the PPE have visible contamination, disinfect with an EPA-registered disinfectant wipe.
- Disinfect the outside of the first bag with an EPA-registered hospital disinfectant applied according to the manufacturer's recommendations.
- Transfer the first bag with the body in it to the gurney, placing it on top of the second bag.
- Disinfect gloved hands using ABHR.
- Fold the second bag material around the first bag and heat-seal 2 inches from the edges while removing as much air from the second bag as possible. Heat-seal the bag a second time 1 inch below the initial seal and then heat-seal diagonally across the corners. Trim off any excess material along the seam. Turn off or unplug the thermal sealer to allow it to cool. The thermal sealer must be decontaminated before being removed from the contaminated area or reused.
- Disinfect the outside of the second bag with an EPA-registered hospital disinfectant applied according to the manufacturer's recommendations.
- Disinfect gloved hands using ABHR.
- Work the third bag around the second bag and then zip it closed. If possible, zip tie the zipper shut.
- Disinfect gloved hands using ABHR.
- Wheel the gurney to the decontamination area.
- Decontaminate the surface of the body bag with an EPA-registered hospital disinfectant applied according to the manufacturer's recommendations. Begin by applying the hospital disinfectant to the top of the bag and any exposed areas of the gurney's cot. Roll the bag to one side to decontaminate half of the bottom of the bag and the newly exposed portion of the gurney's cot. Repeat with the other side of the bag and gurney. When performing decontamination, remove any visible soil on surfaces of the bag or gurney with the EPA-registered disinfectant wipe. After the visible soil has been removed, reapply the hospital disinfectant, and allow sufficient contact time as specified by the manufacturer of the disinfectant.
- Disinfect the surfaces of the gurney from the handles to the wheels with an EPA-registered hospital disinfectant applied according to the manufacturer's recommendations.
- Disinfect gloved hands using ABHR.
- Push the gurney gently so that only the gurney and the decontaminated body bag enter the clean area. The workers in the contaminated area should not enter the clean area. Another set of workers should receive the body in the clean area and transport the body for disposition (see Transportation of Human Remains below).
- Proceed to the PPE removal area and follow the procedures in CDC's PPE guidance. The trained observer should provide instructions on the decontamination and removal of PPE.
At this point, the body bag has been decontaminated, and the potential for further contamination has been eliminated as long as the body is handled carefully. Workers who handle the body bag from this point until the body is cremated or placed into a metal casket should wear single-use (disposable) gloves with extended cuffs and a long-sleeved disposable gown; additional PPE is optional. If there is no evidence that the body bag has been compromised by a tear or puncture or liquid coming from the bag, surfaces that contact the body bag should not be considered contaminated, and gloves and disposable gowns used for transport can be disposed of as regular trash.
Important considerations
- Ensure that anyone handling the body bag wears single-use (disposable) gloves with extended cuffs and a long-sleeved disposable gown.
- Minimize transportation of human remains that contain VHF viruses to the extent possible.
- Coordinate all transportation, including local transport for mortuary care or burial, with relevant local and state authorities in advance.
- Coordinate interstate transport with CDC by calling the Emergency Operations Center at (770) 488-7100.
- Avoid transporting noncremated remains via aircraft.
- Human remains transported for interment, cremation, or medical research at a college, hospital, or laboratory are excepted from the U.S. Department of Transportation's Hazardous Materials Regulations (49 C.F.R., Parts 171-180). See 173.134(b) (14).
Transportation of human remains from the clean area in a hospital to the place of final disposition should be performed by a minimum of two healthcare or mortuary workers. A new set of workers in the clean area receive the decontaminated body bag.
- Place patient identification and any other documents that need to accompany the body, including a printout of the photograph taken before the body was bagged, in an adhesive-backed pouch that is attached to the body bag. This will serve the function of toe tags.
- This should be done after the bagged body enters the clean area but before the bagged body is transported to the morgue or out of the hospital.
- This should be done after the bagged body enters the clean area but before the bagged body is transported to the morgue or out of the hospital.
- Notify the mortuary if the body has any implanted electronic medical devices.
- Affix the infectious substance labels to the body bag before it is moved to the hearse or other vehicle used to transport the body.
- Transport the body from the hospital to a pre-identified hearse or other vehicle.
- A plan should be in place to transport the body safely from the hospital to the hearse or other vehicle used to transport the body. For example, the plan should include a pre-identified route through the hospital that is secure and has minimal patient and personnel traffic. The route should take the body directly to the vehicle being used to transport the body.
- A plan should be in place to transport the body safely from the hospital to the hearse or other vehicle used to transport the body. For example, the plan should include a pre-identified route through the hospital that is secure and has minimal patient and personnel traffic. The route should take the body directly to the vehicle being used to transport the body.
- Transport the body to a pre-identified place of final disposition using a pre-identified route.
- A hospital or public health official should be designated in advance to accompany the body from the hospital to the place of final disposition to ensure the safety of all those involved in the process.
- Protocols should be in place so the designated official accompanying the body knows what to do if the body bag is compromised during transport and how to safely decontaminate it. For example, this official should have a biohazard spill kit with all of the equipment needed for any situation in which the body bag is compromised.
- A hospital or public health official should be designated in advance to accompany the body from the hospital to the place of final disposition to ensure the safety of all those involved in the process.
This guidance is primarily intended to protect workers involved with the disposition of human remains either by cremation (recommended) or burial.
- Ensure that anyone handling the body bag wears single-use (disposable) gloves with extended cuffs and a long-sleeved disposable gown.
- Do not open the body bags.
- Do not embalm the body.
- Do not remove any implanted medical devices.
- Cremate the remains. An oversized cremation container may be needed to contain the bagged body for cremation. Cremated remains are no longer infectious and can be handled and provided to the family using normal procedures.
- Consult your authorized state regulator and EPA regulations governing required cremation temperatures. Cremation and cremation temperatures may be subject to state, local, and EPA regulations.
- Bury the remains only in instances where cremation cannot be safely performed. For example, some crematoriums may have concerns about cremating bodies containing implanted electronic medical devices. Some of these medical devices can explode, potentially damaging the cremation chamber. Most other medical devices can be cremated safely. Where damage to the chamber is a concern, the body should be buried in a standard metal casket or other comparable burial method in accordance with state and local burial requirements. The casket containing the bagged remains can be handled without PPE.
Background
Despite low risk of VHFs in the United States, CDC provides technical guidance to ensure US healthcare facilities are prepared for a possible case. Guidance for specific occupational groups is also available from the Occupational Safety and Health Administration (OSHA) website.
Viruses that cause VHFs can be found in the bodies of patients who die of VHFs. Viruses can be transmitted in postmortem care settings by laceration and puncture with contaminated instruments used during postmortem care, through direct handling of human remains without recommended PPE, and through splashes of blood or other body fluids such as urine, saliva, feces, or vomit to unprotected mucosa such as eyes, nose, or mouth during postmortem care.
In addition to federal laws and guidelines, mortuary facilities and workers may also be subject to a variety of state, tribal, territorial, and local regulations. Consult officials or licensed attorneys in your jurisdiction for additional guidance on laws that affect mortuary practices. CDC recommends close collaboration with public health officials in the state or local jurisdiction, as well as with the licensed funeral director who has agreed to accept the bagged remains, to safely implement each step of the process.
Resources
- PPE: Confirmed Patients and Clinically Unstable Patients Suspected to have VHF
- Handling VHF-Associated Waste | Viral Hemorrhagic Fevers (VHFs) | CDC
- Infection Prevention and Control Recommendations for Patients in U.S. Hospitals who are Suspected or Confirmed to have Selected Viral Hemorrhagic Fevers (VHF) | Viral Hemorrhagic Fevers (VHFs) | CDC
- Interim Guidance for Environmental Infection Control in Hospitals | Viral Hemorrhagic Fevers (VHFs) | CDC
- Medical examiners, coroners, and biologic terrorism: a guidebook for surveillance and case management
PPE, decontamination, and infection control
- PPE selection matrix for occupational exposure to Ebola virus
- Cleaning and decontamination of Ebola on surfaces: Guidance for workers and employers in non-Healthcare/non-laboratory settings
- Safe handling, treatment, transport and disposal of Ebola-contaminated waste
- Body sealer basics
- EPA disinfectants for use against the Ebola virus from List L or List Q
Transportation of remains
- Guidance for importation of human remains into the U.S. for interment or subsequent cremation
- Guidance for handling category A solid waste
Mortuary, burial, and cremation
- Hospital, medical, and infectious waste incinerators fact sheets
- Managing infection risks when handling the deceased
- Pacemaker explosions in crematoria: problems and possible solutions
- Guidelines for protecting mortuary affairs personnel from potentially infectious materials
- Recommended procedures for handling dead human bodies by an authorized cremation authority
