At a glance
- Monkeypox is caused by a virus from the same family as the one that causes smallpox.
- People with monkeypox often get a rash along with other symptoms.
- Monkeypox is spread through close contact with infected people or animals.
- There is no specific treatment for monkeypox, but most people will recover with pain management and supportive care.
Overview
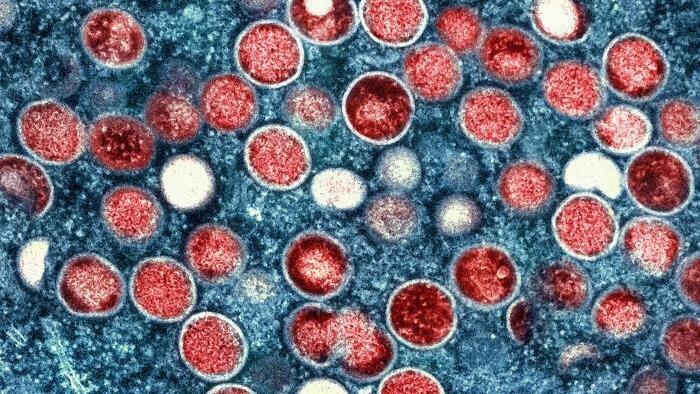
Monkeypox is caused by infection with a virus known as monkeypox virus. This virus is part of the same family as the one that causes smallpox. People with monkeypox often get a rash along with other symptoms. The rash will go through several stages, including scabs, before healing. Monkeypox is not related to chickenpox.
Monkeypox is a zoonotic disease, meaning it can be spread between animals and people. It is endemic, or found regularly, in parts of Central and West Africa. The virus that causes monkeypox has been found in small rodents, monkeys, and other mammals that live in these areas.
Discovery and history
The monkeypox virus was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. Despite being named "monkeypox" originally, the source of the disease remains unknown. Scientists suspect African rodents and non-human primates (like monkeys) might harbor the virus and infect people.
The first human case of monkeypox was recorded in 1970, in what is now the Democratic Republic of the Congo. In 2022, monkeypox spread around the world. Before that, cases of monkeypox in other places were rare and usually linked to travel or to animals being imported from regions where monkeypox is endemic.
Types
There are two types of monkeypox, clade I and clade II:
- Clade I is responsible for the current outbreak in Central and Eastern Africa. Historically, clade I monkeypox caused more severe disease and more deaths. During recent clade Ib outbreaks in Africa, fewer than 0.5% of patients died from the disease. Cases of clade Ib have been found around the world, including in the United States.
- Clade II is the type that caused the global outbreak that began in 2022. Fewer than 0.1% of people infected with clade II die from the disease.

Monkeypox clade similarities and differences
We know that both clades and all subclades of monkeypox can be spread, treated, and prevented the same way, but the risk factors and areas where monkeypox is spreading can be very different.
| Clade la | Clade lb | Clade Ila | Clade llb | |
|---|---|---|---|---|
| Geography | Endemic to Central Africa, including Republic of the Congo, Gabon, Democratic Republic of the Congo (DRC), Central African Republic, and southeastern Cameroon | Newly identified in the DRC with spread to nearby countries; travel-associated cases around the world | Endemic to West Africa, including northwestern Cameroon, Nigeria, Ghana, Cote d'Ivoire, Liberia, and Sierra Leone. | Endemic to West Africa (identified originally in Nigeria); spread to more than 100 non-endemic countries as part of the ongoing global outbreak that began in 2022 |
| Current Situation | Outbreak in Central Africa from 2023 to present | Outbreak in Central and Eastern Africa. There have been travel-associated cases in other parts of Africa, Asia, Europe, and North America, including the United States | Insufficient data | Caused the ongoing global monkeypox outbreak that began in 2022; still circulating globally at low levels, including in the United States |
| Population Primarily Affected in Outbreaks since 2022 | Both adults and children | Adults (often sex workers and their contacts); subsequent spread through day-to-day household contact | Both adults and children | Adults, particularly men who have sex with men in global outbreak |
| What's Known about How it's Spread | Primarily by contact with infected live or dead wild animals. Transmission can also occur via mother to fetus or close skin-to-skin contact, including intimate (e.g., massage, kissing) and sexual contact. | Primarily via close skin-to-skin contact, including intimate (e.g., massage, kissing) and sexual contact. Transmission can also occur via mother to fetus, or within households. | Primarily by contact with infected live or dead wild animals. Transmission can also occur via mother to fetus or close skin-to-skin contact, including intimate (e.g., massage, kissing) and sexual contact. | Primarily via close skin-to-skin contact, including intimate (e.g., massage, kissing) and sexual contact. Transmission can also occur via mother to fetus, or within households. Transmission to healthcare workers from sharps injuries and fomite transmission are rare but have been documented. |
| Mortality Rate | From more recent outbreaks, the mortality rate is ≤ 2.5%. Most deaths occur in people with immunocompromising conditions including children with malnutrition and other health conditions. | Mortality rate is less than 0.5% in Central and Eastern Africa. Most deaths occur in people with immunocompromising conditions. No mortality has been seen with travel associated cases outside Africa, but data are limited. | Mortality rate is around 1% but has limited data. Available data suggest lower CFR than clade I monkeypox | Mortality rate is less than 0.1%. Most deaths occur in people with immunocompromising conditions. |
| Vaccine | 2 doses of JYNNEOS vaccine; 1 dose of ACAM2000 for specific populations | |||
| Other Prevention Considerations | Avoid direct or skin-to-skin contact with people who have a rash that looks like monkeypox, including during sex or intimate contact; avoid objects or materials a person with monkeypox has used; avoid wild animals and animal products (lotions, bushmeat, etc.) in areas where monkeypox occurs regularly; wash hands regularly | |||
| Treatment | Healthcare professionals should assess pain in all patients with monkeypox and recognize that substantial pain may exist from mucosal lesions not evident on physical exam. Additional treatments may be needed for people at higher risk of severe disease. | |||
| Other Therapeutic Considerations | Most people recover with supportive care (nutritious food, fluids, antibiotics for secondary skin infections) and pain control (over-the-counter medications like acetaminophen and ibuprofen, topical steroids and anesthetics like lidocaine for local pain relief; prescription pain medications for short-term management of severe pain). | |||
Signs and symptoms
People with monkeypox often get a rash that may be located on hands, feet, chest, face, or mouth or near the genitals, including penis, testicles, labia, vagina, and anus. The incubation period is 3-17 days. During this time, a person does not have symptoms and may feel fine.
Risk of severe disease
Although most cases of monkeypox are not life-threatening, some people may be more likely to get severely ill, including people who:
- Have severely weakened immune systems
- Are children younger than 1
- Have a history of eczema
- Are pregnant
How it spreads
Both types of monkeypox can spread through:
- Direct contact with infected animals
- Close contact (including intimate contact) with a person with monkeypox
- Direct contact with contaminated materials
Prevention
There are several ways you can protect yourself and others from monkeypox, including:
- Getting vaccinated. Check with your healthcare provider to find out if the monkeypox vaccine is recommended for you.
- Avoiding close, skin-to-skin contact with people who have a rash that looks like monkeypox.
- Avoiding contact with materials that a person with monkeypox has used, including sharing eating utensils and cups, and handling their bedding or clothing.
- Isolating at home if you do get monkeypox
- Covering lesions and wearing a mask if you must be around others
- Avoiding contact with live or dead wild animals if you are in an area of Western or Central Africa where monkeypox occurs regularly
Testing and diagnosis
Monkeypox testing is only recommended if you have a rash that looks with monkeypox and you have other risk factors. People who think they have monkeypox should visit a healthcare provider to ask about testing.
Treatment and recovery
There is no treatment specifically for monkeypox. The type of treatment for a person with monkeypox will depend on how sick someone gets or whether they’re more likely to get severely ill. Most people with monkeypox recover fully within two to four weeks with pain management and supportive care.
