Key points
- Meningococcal disease is serious and can be deadly in hours.
- Early diagnosis and antibiotic treatment are important.
- People spread meningococcal bacteria through close or lengthy contact with other people.
- Anyone can get meningococcal disease, but certain people are at increased risk.
- Vaccines offer the best protection against meningococcal disease.

What it is
Meningococcal disease is a name for any infection caused by bacteria called Neisseria meningitidis.
Types
The two most common types of meningococcal infections are meningitis and bloodstream infections.
With meningococcal meningitis, the bacteria infect the lining of the brain and spinal cord and cause swelling.
With a meningococcal bloodstream infection, the bacteria enter the blood and damage the walls of the blood vessels. This causes bleeding in the skin and organs.
Symptoms
Symptoms are different for meningococcal meningitis and bloodstream infections. However, both are very serious and can be deadly.
Risk factors
Many factors affect someone's risk for meningococcal disease, including age and certain medical conditions and medicines.
Causes
N. meningitidis are bacteria that can live in the back of the nose and throat. About 1 in 10 people have these bacteria in their throat and aren't sick.
Sometimes the bacteria move to other parts of the body and cause infection.
Spread to others
People spread meningococcal bacteria to others by sharing respiratory and throat secretions (saliva or spit).
Generally, it takes close or lengthy contact to spread the bacteria.
- Example of close contact: Kissing
- Example of lengthy contact: Living together
They aren't as contagious as germs that cause the common cold or the flu.
Prevention
Vaccination
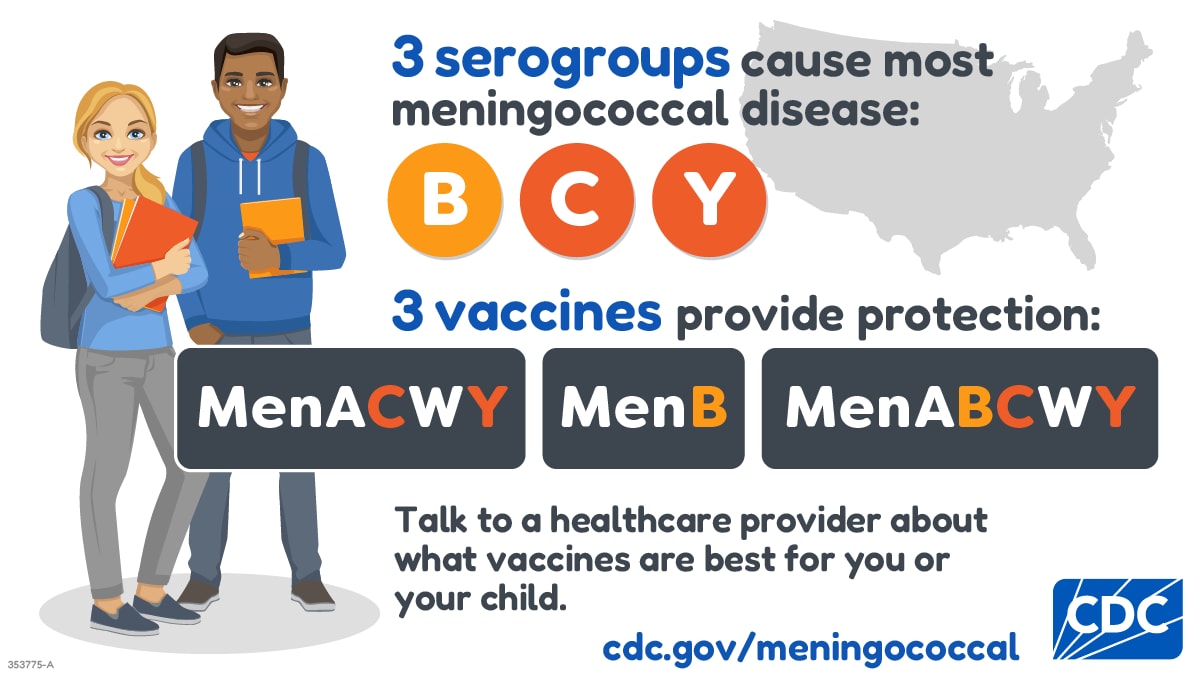
The best way to prevent meningococcal disease is to get vaccinated. CDC recommends meningococcal vaccination for
- All preteens and teens
- Children and adults at increased risk for meningococcal disease
Antibiotics
Close contacts of someone with meningococcal disease should receive antibiotics to prevent them from getting sick. A healthcare provider or health department generally decides who should get preventive antibiotics.
Re-infection
Although rare, people can get meningococcal disease more than once. People who get meningococcal disease twice should get tested to see if they have an underlying immune deficiency (weakened immune system).
Testing and diagnosis
Meningococcal disease can be difficult to diagnose because the signs and symptoms are often similar to other illnesses.
Healthcare providers who suspect meningococcal disease will collect samples of blood or cerebrospinal fluid (fluid near the spinal cord). They then send the samples to a lab for testing.
If bacteria are in the samples, laboratory workers can culture (grow) them. This helps healthcare providers know what's causing the infection and which antibiotic will work best.
Other tests can sometimes detect and identify the bacteria if the cultures don't.
Treatment and recovery
Healthcare providers treat meningococcal disease with antibiotics. A patient will get antibiotics right away if a healthcare provider thinks they have meningococcal disease. Antibiotics help reduce the risk of dying.
Depending on how serious the infection is, people with meningococcal disease may need other treatments, including:
- Breathing support
- Medications to treat low blood pressure
- Surgery to remove dead tissue
- Wound care for parts of the body with damaged skin
