Highlights
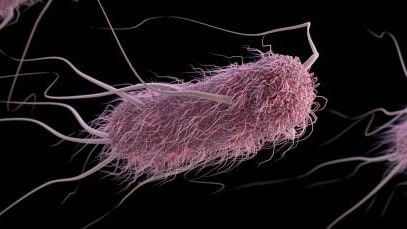
- REPEXH01 is a persistent strain of Shiga toxin-producing E. coli O157:H7 bacteria that has caused illnesses and outbreaks in the United States.
- This strain has caused many outbreaks linked to different sources, such as recreational water, ground beef, and romaine lettuce.
- Additional research could help determine where this strain is coming from and how to prevent future illnesses.
At a glance
Key findings
What is a REP strain?
Learn about REP strains if you are unfamiliar with them.
REPEXH01 is a persistent strain of Shiga toxin-producing E. coli O157:H7 bacteria that has caused illnesses and outbreaks in the United States.
Illness caused by this strain was first reported to PulseNet in 2017. Illnesses caused by this strain occur year-round but are less common in winter.
In the past, the REPEXH01 strain has spread to people through contaminated food and contaminated recreational water.
This strain is relatively diverse genetically. Bacteria in this strain are within 21 allele differences of one another by whole genome sequencing, which is more diverse than typical multistate foodborne outbreaks where bacteria generally fall within 10 allele differences of one another.
Increased diversity can occur over time as strains pass among human hosts, animal hosts, and environmental settings, each with different selective pressures.
What the data show
Illnesses and outbreaks data
Although most enteric illnesses – including those caused by REPEXH01 – are not part of an outbreak, investigation of outbreaks provides information that increases our understanding of germs, sources, settings, and factors that contribute to illness. Moreover, lab-confirmed cases comprise only a small portion of the true number of illnesses that occur because most people do not seek medical care and even fewer submit a stool specimen.
Starting in 2017, CDC and local, state, and federal health and regulatory partners have investigated several outbreaks of E. coli O157:H7 illnesses caused by the REPEXH01 strain.
Summary of selected multistate outbreaks
| Outbreak | Dates People Got Ill* |
Outbreak Source† |
Geographic Location of Outbreak Source** |
Reported Illnesses |
Number of States with Illnesses |
|---|---|---|---|---|---|
| Outbreak A | July 2017 | Recreational water (confirmed) |
California | 10 | 1 |
| Outbreak B | March 2018– August 2018 |
Romaine lettuce (confirmed) |
Arizona | 238 | 37 |
| Outbreak C | August 2018– October 2018 |
Ground beef (suspected) |
Unknown | 12 | 4 |
| Outbreak D | October 2018– December 2018 |
Leafy greens (suspected) |
Unknown | 25 | 10 |
| Outbreak E | May 2019– October 2019 |
Ground beef (suspected) |
Unknown | 44 | 12 |
| Outbreak F | December 2020– January 2021 |
Unknown | Unknown | 22 | 7 |
| Outbreak G | April 2021– June 2021 |
Unknown | Unknown | 5 | 3 |
Selected outbreak publications
- Outbreak B - Multistate outbreak of E. coli O157:H7 infections linked to romaine lettuce
- Outbreak B - Shiga toxin–producing E. coli infections associated with romaine lettuce—United States, 2018
- Outbreak F - E. coli outbreak with unknown food source
Timeline
People with E. coli O157:H7 illnesses caused by the REPEXH01 strain, by date illness began, 2017–2022
Map
E. coli O157:H7 illnesses caused by the REPEXH01 strain, by state, 2017–2022
Laboratory data
Bacteria in this strain are within 21 allele differences of one another by core genome multilocus sequence typing (cgMLST), which is more diverse than typical multistate foodborne outbreaks where bacteria generally fall within 10 allele differences of one another.
This strain includes two major genetic subclusters. Each has caused at least two outbreaks linked to different sources and geographic regions. Possible reasons for the differences among genetic subclusters are still being investigated. More research is needed to determine if any genetic subclusters are associated with specific foods, animal populations, or geographic regions.
Isolates from food, animal, and environmental samples
| Year | Number of Isolates |
Isolate Type | Geographic Location of Source |
Reason Collected |
|---|---|---|---|---|
| 2017 | 1 | Goose feces | California | Outbreak A |
| 2017 | 2 | Lake sediment | California | Outbreak A |
| 2017 | 4 | Lake water | California | Outbreak A |
| 2018 | 24 | Agricultural irrigation water |
Arizona | Outbreak B |
| 2019 | 1 | Ground beef | California | Routine Sampling |
The National Center for Biotechnology Information (NCBI) advances science and health by providing access to biomedical and genomic information. To view the full SNP cluster, click on the link below; then within NCBI's platform click the link underneath the "SNP Cluster" column.
SNP Cluster associated with isolate: PNUSAE031425
Antimicrobial-resistant isolates
The National Antimicrobial Resistance Monitoring System (NARMS) is a national public health surveillance system that tracks antimicrobial resistance for certain intestinal bacteria from ill people (CDC), retail meats (FDA), and food animals (USDA) in the United States. The NARMS program helps protect public health by providing information about emerging antimicrobial resistance, the ways in which resistance is spread, and how resistant infections differ from susceptible infections.
Bacteria from most ill people's samples showed resistance to the antimicrobials chloramphenicol, streptomycin, sulfisoxazole, tetracycline, and trimethoprim-sulfamethoxazole. These findings do not affect treatment guidance because antimicrobials are not recommended for patients with E. coli O157:H7 infection.
Percentage of E. coli O157:H7 REPEXH01 isolates from ill people that were antimicrobial resistant, by antimicrobial (n = 596), as of August 31, 2022 — NARMS
Collaborate with CDC
Interested in collaborating on a project related to this strain? Contact CDC at REPStrains@cdc.gov.
About the data
Summary of selected multistate outbreaks
Outbreak dates are based on reported or estimated illness onset dates.
Confirmed sources were implicated by epidemiologic plus traceback or laboratory data. Suspected sources were implicated by epidemiologic data only. More information available in the latest summary of possible multistate enteric disease outbreaks.
The geographic location of a confirmed outbreak source may not always be known. This can happen when a food containing multiple ingredients (e.g., bagged salad blend) is confirmed as the source, but the evidence cannot implicate a specific food, or when evidence confirms an outbreak source but traceback cannot pinpoint the exact geographic location of the source.
Timeline
N=634 for whom information was reported as of September 2, 2022. Some illness onset dates have been estimated from other reported information.
PulseNet transitioned to using whole genome sequencing (WGS) as the standard subtyping method for STEC in July 2019. Before then, not all STEC isolates reported to PulseNet had WGS data available. Isolates are identified as part of this strain based on WGS. As a result, the number of people with lab-confirmed illness caused by this strain before 2019 may be underrepresented.
Map
Outbreak dates are estimated, based on reported or estimated illness onset dates.
Antimicrobial resistant isolates
Resistance was determined based on the results of antimicrobial susceptibility testing when available (n = 73 isolates); otherwise, resistance was predicted based on whole genome sequencing (n = 523).
Ciprofloxacin data includes isolates carrying a single quinolone resistance gene (n = 2; 0.3%); a single gene may result in interpretation of “intermediate” or “susceptible” for ciprofloxacin on antimicrobial susceptibility testing.
