At a glance
CDC’s 2022 Investigations of Possible Multistate Outbreaks Caused by Salmonella, Shiga toxin-producing E. coli (STEC), Listeria monocytogenes, and Campylobacter.
Key Findings
- During 2022, CDC investigated 149 possible multistate outbreaks, of which 79 were determined to be outbreaks. Of these, outbreak investigators solved 46 outbreaks (58%). A suspected source was identified for 19 outbreaks and a confirmed source was identified for 27 outbreaks.
- The 26 solved multistate outbreaks linked to contaminated food caused 882 illnesses, 304 hospitalizations, and 16 deaths. The 20 solved multistate outbreaks linked to animal contact caused 1,400 illnesses, 299 hospitalizations, and 2 deaths.
- Leafy greens were identified as the source of the most solved foodborne outbreaks (5) during 2022. Dairy, beef, and seeded vegetables were also identified as the source of foodborne outbreaks (4 each) during 2022.
- Contact with backyard poultry was identified as the source of both the most solved animal contact outbreaks (13) and the most outbreak-associated illnesses (1,229) of any animal contact category.
Possible multistate outbreaks
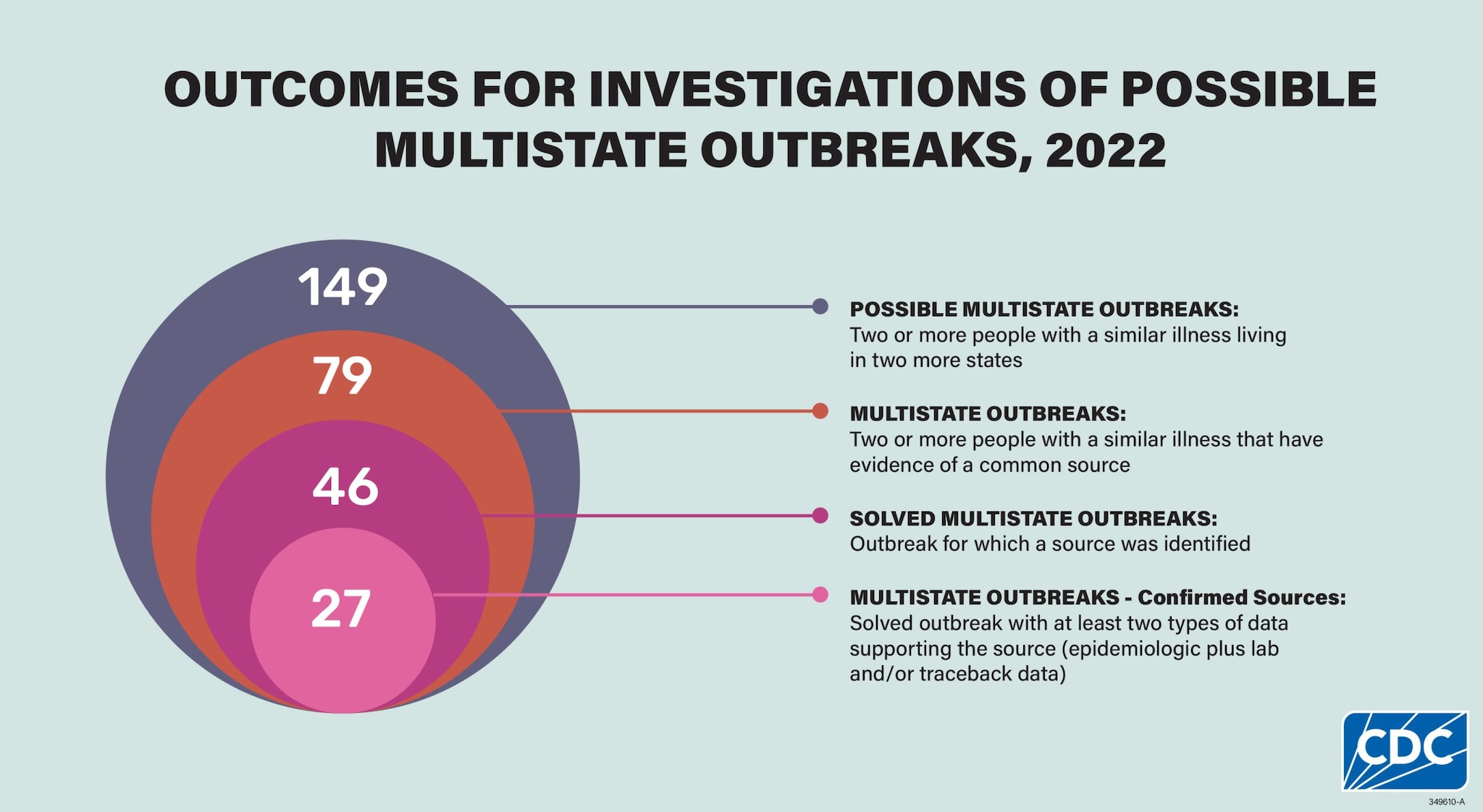
This analysis includes 149 investigations of possible multistate enteric (intestinal) outbreaks caused by Salmonella, Shiga Toxin-Producing Escherichia coli (STEC), Listeria monocytogenes, or Campylobacter during 2022. Some possible outbreaks were excluded from this report because they were determined to be single state or because they were linked to international travel. After investigation, 79 (53%) of these were determined to be multistate outbreaks, and investigators solved 46 (58%) of these outbreaks.
Multistate Outbreaks
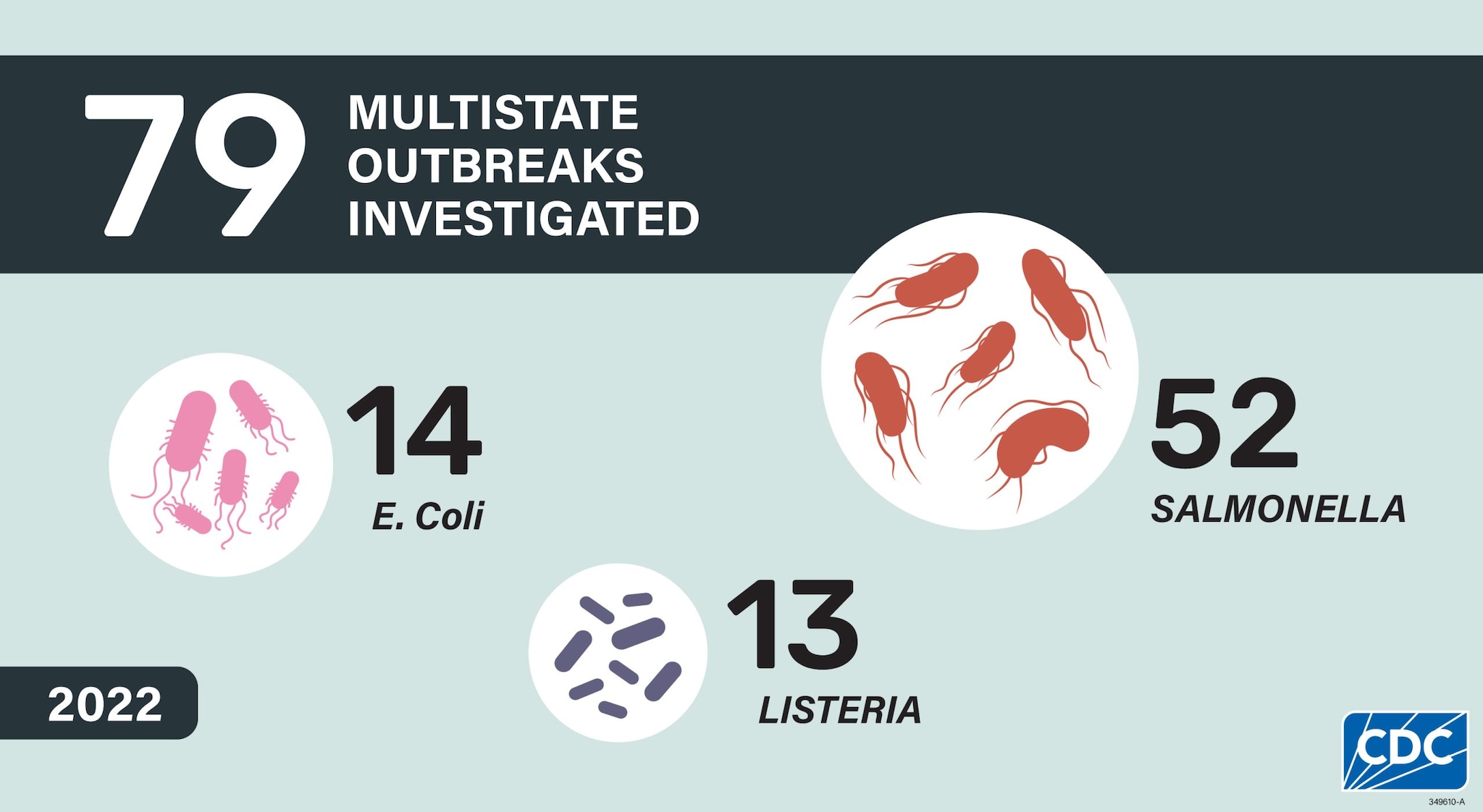
No multistate outbreaks caused by Campylobacter were identified in 2022. Consistent with what was seen in previous summaries, Salmonella caused the highest number of multistate outbreaks (52) and illnesses (2,578), comprising 66% of the multistate outbreaks and the overwhelming majority (86%) of illnesses. The number of outbreaks increased slightly from 2021. The number of multistate outbreaks in 2022 is nearly back to its highest level (2019) following several years that were significantly impacted by the COVID-19 pandemic.
Figure 1: Number of Multistate Outbreaks Investigated, by Year and Pathogen*
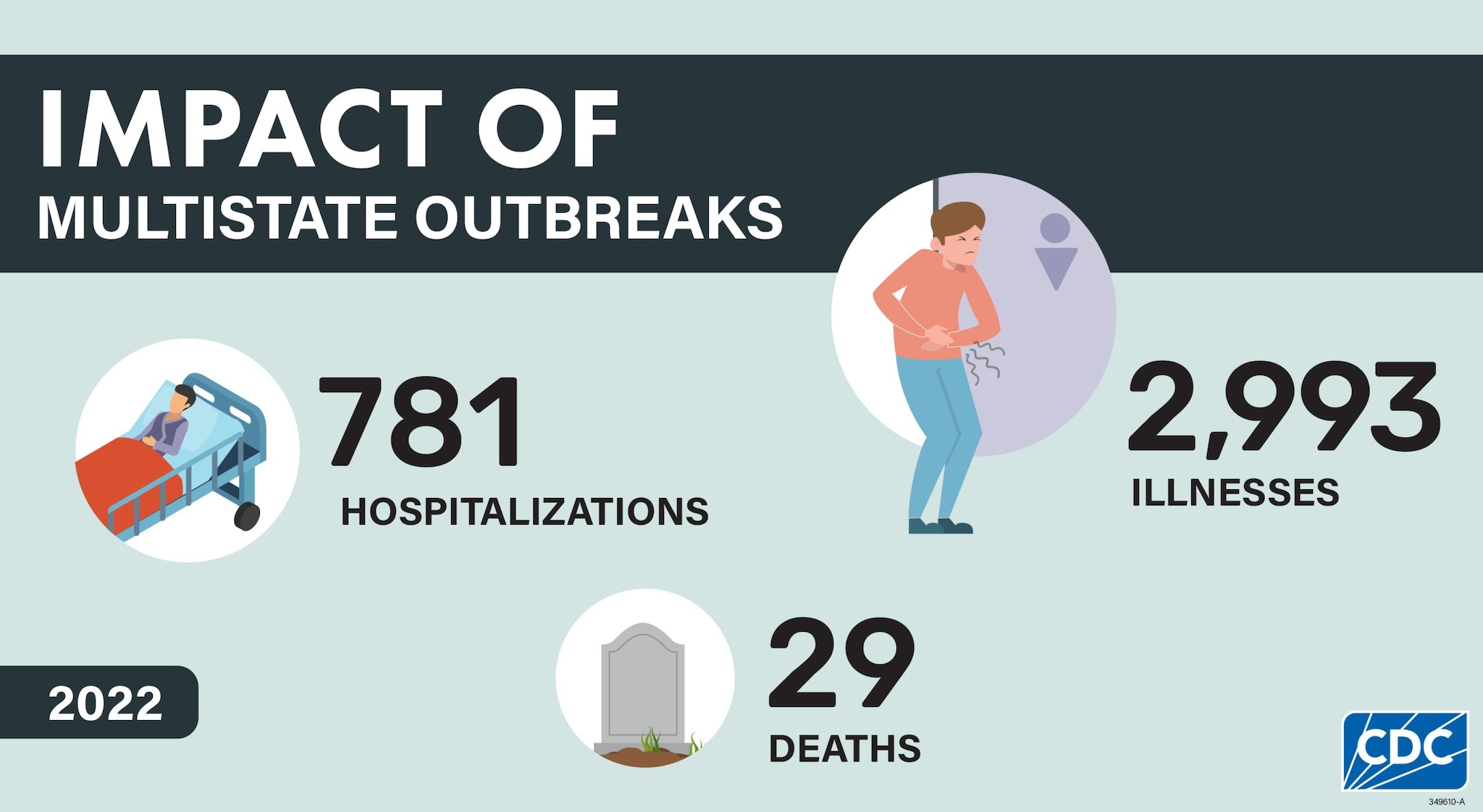
The 79 investigated multistate outbreaks resulted in 2,993 illnesses, 781 hospitalizations, and 29 deaths. These numbers substantially underrepresent the true number of illnesses caused by these outbreaks because many people do not seek medical care or do not get tested to see what could be causing their illness. Without testing, they are not identified as being part of a multistate outbreak.
Solved Multistate Outbreaks
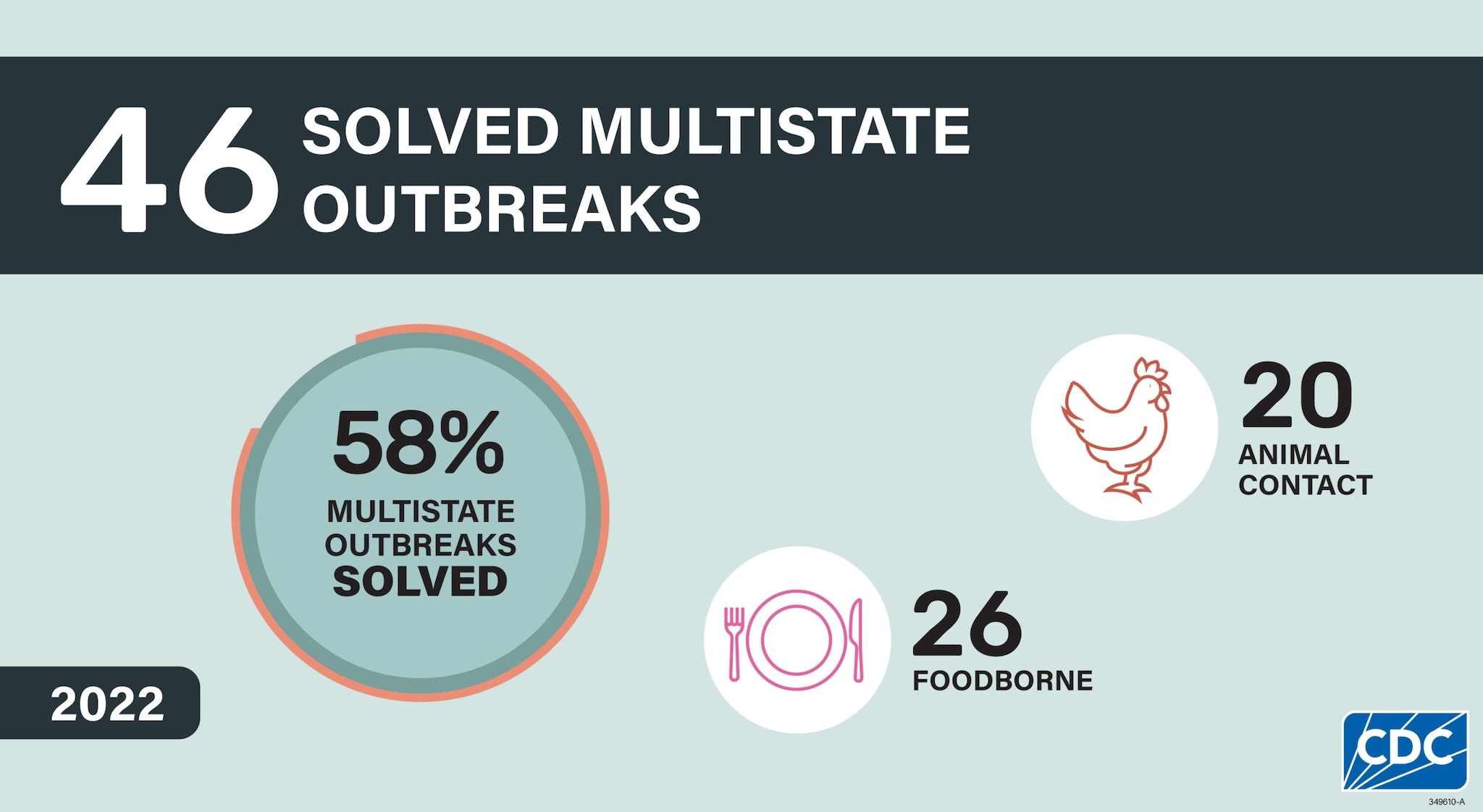
Among the 79 multistate outbreaks, 46 (58%) were solved, meaning a confirmed or suspected source of the outbreak was identified, including 27 (59%) outbreaks with confirmed sources and 19 (41%) with suspected sources. Among the 46 solved outbreaks, 26 (57%) were linked to contaminated foods, and 20 (43%) were linked to animal contact.
Figure 2: Solved Multistate Foodborne and Animal Contact Outbreaks, 2016–2022
Figure 3: Illnesses in Solved Multistate Foodborne and Animal Contact Outbreaks, 2016–2022
Solved multistate outbreaks caused at least 2,282 illnesses. Solved multistate outbreaks linked to contaminated food caused 882 illnesses, 304 hospitalizations, and 16 deaths, while multistate outbreaks linked to animal contact caused 1,400 illnesses, 299 hospitalizations, and 2 deaths.
Highlights
Salmonella and Bearded Dragons

Why were these outbreaks notable?
Bearded dragons are popular non-traditional pets given their calm temperament, size, and appearance. But, like all reptiles, bearded dragons can carry and shed Salmonella bacteria even if they look clean and healthy. During 2022, three multistate outbreaks of Salmonella illnesses in people were linked to bearded dragon contact in the United States. This is an unusually high number of multistate outbreaks. The outbreaks were caused by several rare Salmonella serotypes and they disproportionately affected children under 5 years of age. In two of these investigations, public health partners collected samples that found the Salmonella outbreak strains from a bearded dragon, its food, or its environment in a sick person’s home. These results mean that people likely got sick from touching bearded dragons or things in their habitat. Traceback information showed that there were pet stores, breeders, and suppliers distributing bearded dragons in common across the three outbreaks.
What happened as a result of these outbreaks?
CDC, state public health, and state agriculture partners worked together with key pet industry partners to learn about biosecurity practices and share prevention information. CDC Investigation Notices detailed investigation findings from each of the three outbreaks. CDC continues to work with bearded dragon breeders, suppliers, and retailers to help identify interventions to reduce Salmonella burden at each step in the distribution chain and to disseminate prevention messages to the public. These partnerships are instrumental to limit Salmonella transmission from bearded dragons and their environments to people, especially children.
Salmonella and Jerky-Style Pet Treats
Why was this outbreak notable?

In April 2022, CDC was contacted by the US Department of Agriculture Food Safety and Inspection Service (USDA-FSIS) regarding Salmonella Muenchen identified in dried beef. The dried beef was produced for human consumption at a facility that also produced jerky-style pet treats. Whole genome sequencing (WGS) showed that the Salmonella Muenchen from the dried beef was closely related genetically to Salmonella Muenchen that was making people sick. An investigation by state and federal public health partners determined that while one patient reported consuming dried beef products that might have come from the processing facility, most patients reported contact with dogs and feeding their dogs jerky-style pet treats. These findings emphasize the importance of a One Health approach to outbreak investigations because enteric pathogens can contaminate facilities that make products for both human and animal consumption.
What happened as a result of this outbreak?
Routine follow-up by USDA-FSIS at the processing facility found that the outbreak strain of Salmonella Muenchen was still present on processing equipment after the contaminated lots of dried beef had been destroyed. The outbreak strain was also later identified in turkey products for human consumption and turkey cecal contents from additional facilities, suggesting that the outbreak strain may not be limited to a single commodity or that cross-contamination within the facilities may have occurred. In addition, testing of finished chicken jerky-style pet treats by state agriculture officials identified Salmonella Infantis. Although no human illnesses were found with this strain, the firm voluntarily recalled the product. Collaboration between multiple federal and state agencies was necessary to track all potential sources of the outbreak strain and emphasizes the complexity of investigations where food products for human and animal consumption might both be sources of illness. This investigation highlights the importance of collecting information about patients’ exposures to pet foods and treats to inform laboratory testing and understand traceback in multi-vehicle outbreaks.
Listeria and Ice Cream

Why were these outbreaks notable?
In 2022, investigators linked ice cream to two multistate listeriosis outbreaks, highlighting the continued emergence of ice cream as a source for Listeria monocytogenes infections. While ice cream served to people in hospitals, long term care facilities, and nursing homes caused three previous Listeria outbreaks, both 2022 outbreaks were caused by ice cream sold to the general public. Unlike the previous outbreaks, the people sickened included pregnant women, teenagers, and otherwise healthy people. The largest outbreak was linked to ice cream primarily sold at ice cream shops in a single state, but it caused serious illness in 28 people from 11 states, including 27 hospitalizations, one death, and one pregnancy loss. Testing identified the outbreak strain of Listeria monocytogenes in the production environment and in 16 of the 17 flavors offered from the company. The second outbreak sickened three people in two states. These outbreaks demonstrate the importance of comprehensive Listeria monocytogenes control plans for producers of ice cream and other frozen, ready-to-eat foods.
What happened as a result of these outbreaks?
As a result of the larger outbreak, the state regulatory agency issued three citations to the company and FDA issued a warning letter. The company is currently not producing ice cream and eventually paid $4 million in a wrongful death lawsuit. CDC and FDA are working together to create outreach materials for smaller ice cream firms to highlight the need for Listeria control and to promote available educational materials.
Listeria and Soft Cheese
Why were these outbreaks notable?

In 2022, two listeriosis outbreaks were linked to soft cheeses made with pasteurized milk and sickened 10 people, including 2 pregnant women or their newborns. Most people were sick enough to be hospitalized for their illness. One outbreak was linked to contaminated brie and camembert cheeses, and sampling found the Listeria strain causing illness in the cheese-making facility. Investigators suspected queso fresco made with pasteurized milk as the source of the second outbreak. Unpasteurized queso fresco-type soft cheeses are a well-known source of listeriosis outbreaks. However, these outbreaks highlight that soft cheeses made with pasteurized milk can also be contaminated with Listeria during cheese-making. They also highlight the need for manufacturers of pasteurized milk cheeses to implement appropriate control measures to prevent Listeria contamination during the production process.
What happened as a result of these outbreaks?
Pregnant women and other people at higher risk for listeriosis have long been advised to avoid eating unpasteurized (raw) soft cheeses. Given the recent identification of pasteurized milk cheeses as the cause of listeriosis outbreaks, CDC is collaborating with FDA to review its current Listeria prevention guidance. In response to repeated outbreaks linked to soft fresh queso fresco-style cheeses, FDA released a strategy aimed at enhancing the safety of these foods to prevent future outbreaks
Salmonella and melons

Why was this outbreak notable?
In 2020, environmental testing done during an investigation of a multistate outbreak of Salmonella Newport infections linked to whole melons from southwest Indiana identified a strain of Salmonella Typhimurium from soil in the fields where melons were grown. As a result, CDC began actively monitoring for illnesses with this strain. In 2022, illnesses with the Typhimurium strain were rapidly detected, growing to an outbreak that sickened 87 people in 11 states. Whole cantaloupe grown in southwest Indiana were identified as the source of the outbreak. Environmental testing conducted by FDA at multiple farms identified multiple Salmonella strains in the on-farm, post-harvest, and off-farm environments, including the outbreak strain of Salmonella Typhimurium and the same Salmonella Newport strain that caused the 2020 outbreak. This outbreak highlights that Salmonella may persist in the environment where produce is grown for several years, and that persisting contamination can be a risk to produce safety.
What happened as a result of this outbreak?
As a result of this investigation, CDC designated this Salmonella Typhimurium strain as a REP strain, which will facilitate active tracking of illnesses from this strain and more rapid identification and investigation of outbreaks. FDA provided recommendations to growers of melons and similar produce to help prevent contamination. FDA and state partners are also working with the melon growers in the region to increase awareness of the risk Salmonella contamination of whole melons and develop prevention strategies.
Multistate Outbreaks Linked to Food
Figure 4: Solved Multistate Foodborne Outbreaks, by Year and Pathogen, 2016–2022
Of the 46 total solved multistate outbreaks, 26 were found to be linked to contaminated foods. Half (50%) had suspected food vehicles and half had a confirmed food vehicle.
These solved multistate foodborne outbreaks were associated with 882 illnesses, 304 hospitalizations, and 16 deaths. Ill people in these outbreaks ranged in age from less than 1 year to 94 years, with a median age of 40; 56% were female. Among all illnesses related to solved foodborne outbreaks, 4% occurred in children under 5 and 24% occurred in adults 65 years and older, age groups at higher risk for severe illness. When compared with Salmonella or STEC infections, a higher proportion of solved multistate foodborne outbreaks of Listeria infections were in adults aged 65 and over (63%). Salmonella caused the most solved multistate foodborne outbreaks (13 outbreaks, 50%), followed by Listeria (7 outbreaks, 27%), and STEC (6 outbreaks, 23%). Foodborne Salmonella outbreaks caused more illnesses (median: 44 illnesses, range: 12–103) compared to outbreaks caused by STEC (median: 11 illnesses, range: 7–109) and Listeria (median: 12 illnesses, range: 3–28).
Figure 5: Solved Multistate Foodborne Outbreaks, by Pathogen, 2022
Figure 6: Illnesses in Solved Multistate Foodborne Outbreaks, 2022
Figure 7: Hospitalizations in Solved Foodborne Outbreaks, 2022
As in previous years, illnesses associated with solved multistate foodborne Listeria outbreaks were more severe: overall, 96% of people in Listeria outbreaks were hospitalized and 18% died, compared to 30% of people hospitalized and 0.5% of people who died in multistate Salmonella outbreaks and 51% of people hospitalized and 0% died in STEC outbreaks.
Figure 8: Percentage of Ill People that were Hospitalized in Solved Foodborne Outbreaks, by Pathogen, 2022
CDC’s Outbreak Response and Prevention Branch (ORPB) assigned food categories for specific foods linked to outbreaks based on the Interagency Food Safety Analytics Collaboration (IFSAC) categorization scheme. Vegetable row crops were identified as the source of the most solved foodborne outbreaks (5) during 2022. Leafy greens were the product identified in all five outbreaks due to vegetable row crops, accounting for 160 illnesses, 93 hospitalizations, and 11 deaths. Dairy products, beef, and seeded vegetables were each identified as the source of four solved foodborne outbreaks. Two outbreaks associated with dairy products involved pasteurized soft cheeses and two involved ice cream. The four outbreaks associated with beef were due to contaminated ground beef and jerky-style pet treats that were made in a facility that also produces jerky for human consumption. The four seeded vegetable outbreaks all involved tomatoes. The two outbreaks in the “Other” category include one linked to frozen falafel and one linked to deli meats and cheeses.
Figure 9: Solved Multistate Foodborne Outbreaks by Food Category, 2022
Figure 10: Number of Illnesses Associated with Solved Multistate Foodborne Outbreaks, by Food Category, 2022
| Food Category | Pathogen(s) | Confirmed Source(s) | Suspected Source(s) |
|---|---|---|---|
| Vegetable Row Crops | STEC (3 suspected) and Listeria (1 confirmed, 1 suspected) | Prepackaged salad (1) | Leafy greens (1), Iceberg lettuce (1), Fresh spinach (1), Romaine lettuce (1) |
| Beef | STEC (1 confirmed, 1 suspected) and Salmonella (2 confirmed) | Jerky-Style Pet Treats (1), Ground Beef (2) | Beef (1) |
| Dairy | Listeria (3 confirmed, 1 suspected) | Ice cream (2), Brie and Camembert (1) | Queso Fresco (1) |
| Seeded Vegetables | Salmonella (4 suspected) | N/A | Tomatoes (4) |
| Chicken | Salmonella (1 confirmed, 1 suspected) | Chicken (1) | Chicken (1) |
| Fish | Salmonella (1 confirmed, 1 suspected) | Salmon (1) | Raw Tuna (1) |
| Other | STEC (1 confirmed) and Listeria (1 suspected) | Frozen Falafel (1) | Deli Meats and Cheeses (1) |
| Fruit | Salmonella (1 confirmed) | Melons (1) | N/A |
| Sprouts | Salmonella (1 confirmed) | Alfalfa Sprouts (1) | N/A |
| Nuts-Seeds | Salmonella (1 confirmed) | Peanut Butter (1) | N/A |
Outbreaks Linked to Animal Contact
Of the 46 solved multistate outbreaks, 20 were linked to contact with animals. These outbreaks were associated with 1,400 illnesses, 299 hospitalizations, and 2 deaths. During 2022, Salmonella caused all outbreaks linked to contact with animals. During 2022, investigators solved all 20 outbreaks linked to animal contact.
Sick people in multistate outbreaks linked to animal contact ranged in age from less than 1 to 102 years, with a median age of 34 years; 22% of illnesses occurred in children younger than 5, and 16% occurred in adults aged 65 and older. The proportion of sick people younger than 5 was higher for solved multistate animal contact outbreaks (22%) than for solved multistate foodborne outbreaks (4%). Over half (56%) of ill people were female. Among all multistate animal contact outbreaks, the median percentage of people hospitalized per outbreak was 36%, with a range of 17–50% of people hospitalized.
Figure 11: Total Number of Illnesses from Multistate Animal Contact Outbreaks linked to Backyard Poultry, 2016–2022
During 2022, there were 13 solved multistate outbreaks, 1,229 illnesses, 247 hospitalizations, and 2 deaths linked to contact with backyard poultry. Animal contact outbreaks linked to contact with backyard poultry outnumbered those linked to all other animal sources combined. Backyard poultry, such as chickens, ducks, geese, and turkeys can carry Salmonella even if they appear clean and show no signs of illness.
Figure 12: Number of Outbreaks Associated with Solved Multistate Animal Contact Outbreaks, by Animal Contact Category, 2022
Figure 13: Number of Illnesses Associated with Solved Multistate Animal Contact Outbreaks, by Animal Contact Category, 2022
Scaled reptiles caused the second highest number of multistate outbreaks linked to animal contact. The four multistate outbreaks linked to scaled reptiles caused 102 illnesses, 33 hospitalizations, and 0 deaths during 2022. Children under the age of 5 years accounted for 27% of the illnesses associated with these four scaled reptile outbreaks. Three of the four outbreaks associated with scaled reptiles were linked specifically to bearded dragons. The fourth was linked to lizards in general, with geckos and bearded dragons being suspect vehicles. Lizards such as bearded dragons can carry Salmonella even if they look healthy and clean and can shed Salmonella intermittently.
| Animal Category | Pathogen(s) | Confirmed Source(s) | Suspected Source(s) |
|---|---|---|---|
| Backyard Poultry | Salmonella (8 confirmed, 5 suspected) | Backyard Poultry (8) | Backyard Poultry (5) |
| Scaled Reptiles | Salmonella (3 confirmed, 1 suspected) | Bearded Dragons (3) | Lizards (1) |
| Turtles | Salmonella (3 confirmed) | Small Turtles (3) | N/A |
What's being done
When investigators find the food or animal source of a multistate outbreak, agencies can take actions, such as issuing outbreak notices or requesting that companies recall contaminated products. Warning the public quickly about contaminated foods or animal contact outbreaks can prevent illnesses and save lives. Not every outbreak with a confirmed source results in product actions or outbreak notices. Outbreaks may end by the time the source is confirmed, or investigators may determine that the contaminated food is no longer available for sale.
In 2022, CDC issued outbreak notices for 14 investigations. The 14 investigations included 10 linked to contaminated foods (9 with a confirmed source, 1 with an unknown food source,) and 4 linked to animal contact. Among the 9 investigations with a confirmed food source, 6 resulted in food recalls. In total, the outbreak notices received more than 2.6 million page views, including a large Salmonella outbreak linked to peanut butter which received nearly 1 million views.
CDC uses social media to disseminate and make outbreak advice accessible to the public. In 2022, outbreak posts on CDC’s Instagram, X (previously Twitter), and Facebook received more than 40 million impressions in total. A Facebook post about a Salmonella outbreak linked to peanut butter was CDC’s top post for 2022 with more than 23.5 million views.
In 2022, CDC started creating short videos on social media to expand reach and foster engagement among younger people. Six videos were created and disseminated. The 6 videos for 4 outbreaks received nearly 2.2 million views on Instagram. One video became CDC’s most-viewed social media video at the time, which was for a Listeria outbreak linked to brie cheese with 747,080 views.
For more information on how CDC decides to communicate during foodborne outbreaks, please see the Issuing Foodborne Outbreak Notices web page.
Methods
The data sources and methods used for the analyses in this report have been previously described in detail in the previous “Summary of Possible Multistate Enteric (Intestinal) Disease Outbreaks from 2017–2020” and in the MMWR report of 2016 data. Briefly, CDC maintains an internal tracking database in the System for Enteric Disease Response, Investigation, and Coordination (SEDRIC) of investigations coordinated by CDC of possible multistate outbreaks caused by Salmonella, Shiga Toxin–Producing Escherichia coli (referred to as STEC for simplicity throughout this report), Listeria monocytogenes (referred to as Listeria throughout this report), and Campylobacter. Investigation of possible multistate outbreaks of Campylobacter began in 2022, although no outbreaks of Campylobacter were identified in this report year. These analyses were based on data available in SEDRIC on August 3, 2023, and may differ from previously published reports. An investigation of a possible multistate outbreak was included in this report if it began on or after January 1, 2022, and ended on or before March 31, 2023; or if it began before 2022 but ended during April 1, 2022–March 31, 2023. For outbreaks linked to specific foods, outbreak vehicles were provisionally assigned food categories based on the fourth-level Interagency Food Safety Analytics Collaboration (IFSAC) categorization scheme. Outbreak illnesses represent a small proportion of all foodborne illness. People who are sick with a foodborne illness may not seek medical care or be tested for foodborne pathogens.
The number of multistate outbreaks reported here will differ from the number of outbreaks reported in CDC’s Foodborne Disease Outbreak Surveillance System (FDOSS), which includes both single state and multistate outbreaks and a larger group of pathogens. In addition, the investigation year in this report, which is based on when CDC investigated the possible outbreak, may differ from the outbreak year in FDOSS, which is based on when outbreak-associated illnesses occurred. ORPB provisionally assigned IFSAC food categories to outbreaks in this report. Final IFSAC food category assignments for both single state and multistate outbreaks are made during the annual FDOSS outbreak closeout process.
Acknowledgements
This work would not be possible without the collaboration and critical work of many partners, including local, state, tribal, and territorial health and agriculture departments; the PulseNet database team, CDC; the Outbreak Response and Prevention Branch (ORPB), CDC; Food and Drug Administration Coordinated Outbreak Response and Evaluation Network, Washington, DC; and the U.S. Department of Agriculture Food Safety and Inspection Service Office of Public Health Science, Applied Epidemiology Staff, Washington, DC. We would like to also acknowledge Lexi Palacios, Grace Vahey, Karen Neil, Michael Ablan, Kathy Benedict, Zhen Liu, Lauren Gollarza, Sean Stapleton, Kate Varela, and Sarah Collier (ORPB) for their efforts during the writing of this report.
