At a glance
Overview
CDC expects the upcoming fall and winter respiratory disease season will likely have a similar or lower number of combined peak hospitalizations due to COVID-19, influenza, and RSV compared to last season.
This outlook is intended to provide decision-makers with information to assist in public health preparedness for respiratory virus illnesses during the 2024-2025 fall and winter respiratory season, such as when hospitals might experience the most demand.
Our assessments are based on expert opinion, historical data, and scenario modeling conducted by the Center for Forecasting and Outbreak Analytics for COVID-19, influenza, and RSV. As with all long-range scenarios, there is inherent uncertainty, which we describe below.
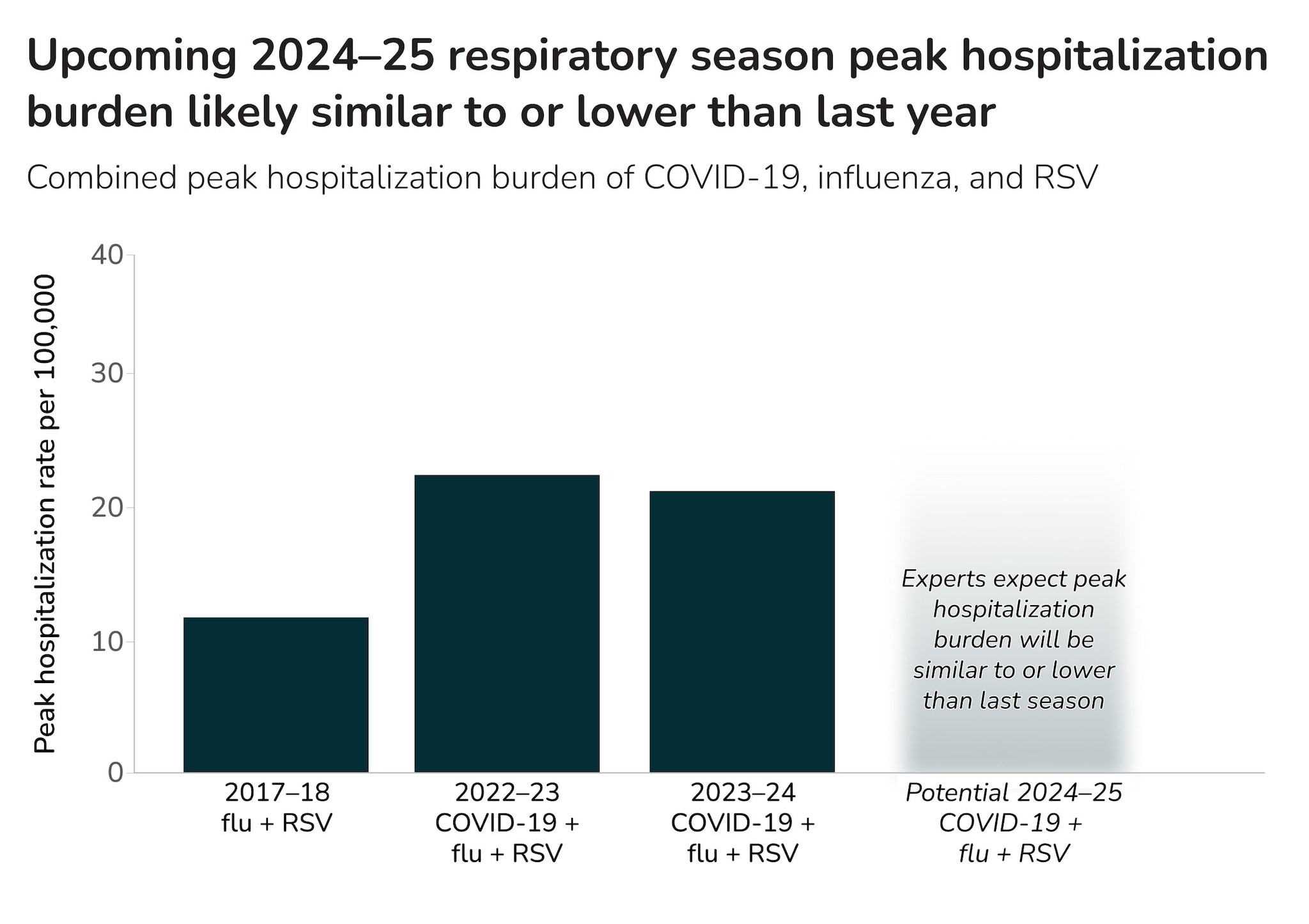
For this seasonal outlook, CDC defined three potential scenarios for the combined peak hospitalization burden of COVID-19, influenza, and RSV for the 2024-2025 respiratory season (Table 1). We then consulted a range of CDC and external experts on COVID-19, influenza, RSV, and disease forecasting to assess the likelihood of each scenario and provide associated confidence levels. The experts estimated there's a roughly 80% chance that peak combined hospitalization burden will be similar to or lower than last season, with low confidence (Figure 1, Table 1).
Table 1. Scenarios for combined peak hospitalization burden for COVID-19, influenza, and RSV
Scenario relative to 2023-2024
Definition
Percentage chance estimated by experts
Similar peak
The combined peak hospitalization burden for the 2024-2025 season will be similar (within +/- 20%) to the combined peak burden for the 2023-2024 respiratory season.
54%
Lower peak
The combined peak hospitalization burden for the 2024-2025 season will be substantially lower (at least 20%) than that of the 2023-2024 respiratory season.
28%
Higher peak
The combined peak hospitalization burden for the 2024-2025 season will be substantially higher (at least 20%) than that of the 2023-2024 respiratory season.
18%
Factors that could lead to higher peak hospitalization rate
While we expect this season's peak hospitalization rate will be similar to or lower than last year, there is still a risk of a higher peak rate, underscoring the need to consider this possibility in planning and preparedness activities. The following factors could drive higher peak rate:
- Emergence of a new COVID-19 variant with an increased ability to evade the body's prior immunity, or a new COVID-19 variant associated with higher clinical severity.
- Predominance of an influenza subtype with more severe outcomes.
- Lower vaccine uptake or effectiveness, including:
- If there is lower than projected uptake of the COVID-19 vaccine, influenza seasonal vaccine, or RSV vaccines and immunizations.
- If the updated 2024-2025 COVID-19 vaccine effectiveness against hospitalization is lower than that of the 2023-2024 vaccine.
- If influenza seasonal vaccine effectiveness against hospitalization is lower than projected.
- If there is lower than projected uptake of the COVID-19 vaccine, influenza seasonal vaccine, or RSV vaccines and immunizations.
COVID-19 outlook
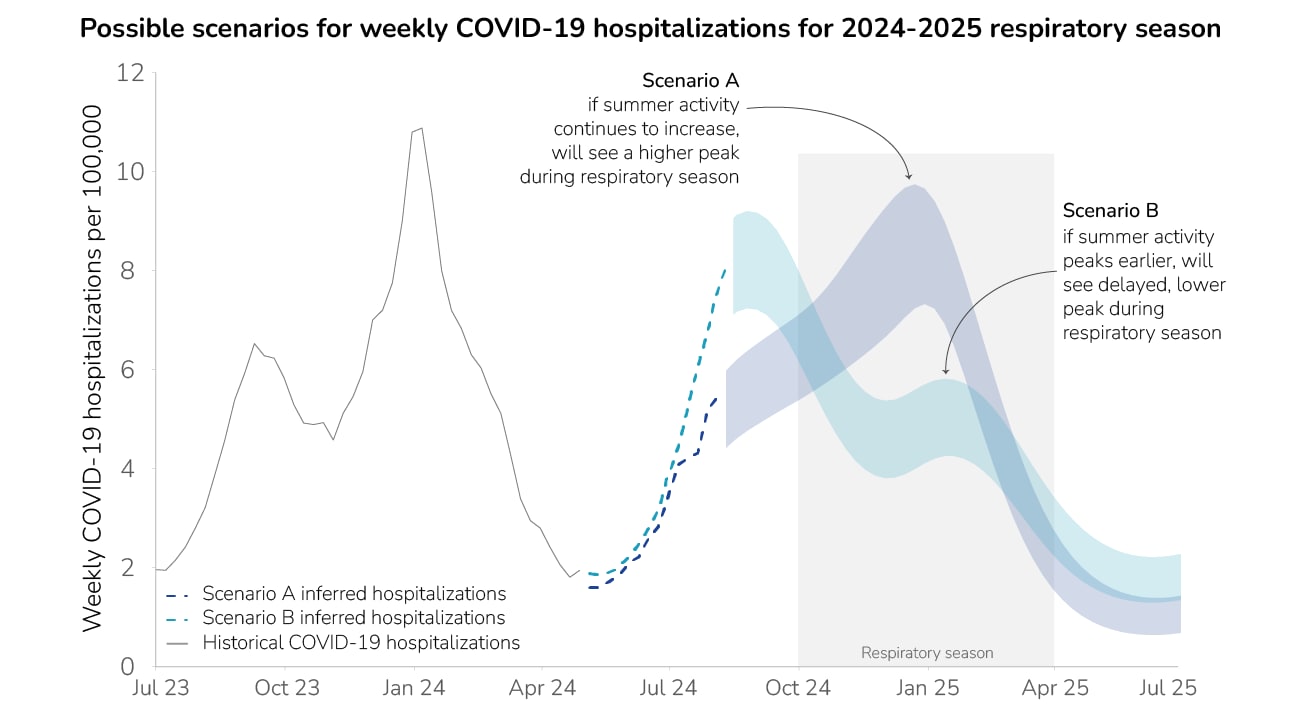
CDC projects that the peak weekly hospitalization rate due to COVID-19 will be similar to or lower than that of the 2023-2024 seasonA with moderate confidence. COVID-19 activity this fall and winter will depend on the progression of the ongoing summer COVID-19 wave. Therefore, we developed two different COVID-19 hospitalization burden scenarios for the 2024-2025 respiratory season to demonstrate the range of possibilities for how this season could unfold (Figure 2).
Our two scenarios are based on inferred COVID-19 weekly hospitalizations for the summer using two different surveillance systems: hospitalization data for a relatively small subset of hospitals (Scenario A) or emergency department visit data (Scenario B)B.
If COVID-19 activity continues to increase and does not peak before the start of the fall and winter respiratory virus season (October to April), modeling indicates that the wave may peak early during the respiratory season—with a peak weekly COVID-19 hospitalization rate between 7.2 and 9.7 hospitalizations per 100,000 occurring in late December (Scenario A, Figure 2). However, if the current COVID-19 summer wave peaks before the respiratory season begins, modeling suggests a second, smaller wave could occur during the respiratory season, with a peak weekly COVID-19 hospitalization rate between 4.2 and 5.8 hospitalizations per 100,000 occurring in mid-January (Scenario B, Figure 2). The peak COVID-19 hospitalization rate for both scenarios is lower than that of last season. A lower peak hospitalization burden due to COVID-19 could lead to a lower overall combined peak hospitalization burden during the 2024-2025 respiratory season.
We assumed that variants will emerge with similar properties to those that drove last winter's peak, and that the 2024-2025 vaccine will have similar uptake and performance as last year's vaccine. The potential impact of vaccination could change based on the timing and size of the winter peak. While our model can also be used to evaluate the impact of interventions such as vaccinations, given the uncertainty in the impact of the current summer wave, we chose instead to focus on these two different COVID-19 hospitalization burden scenarios for the 2024-2025 season.
Influenza outlook
CDC projects the peak hospitalization rate due to influenza will be similar to or lower than that of the 2023-2024 season rate of 8.9 weekly laboratory-confirmed hospitalizations per 100,000, with moderate confidence. However, past seasons have varied widely in the number of illnesses, hospitalizations, and deaths, depending on the subtypes circulating, population immunity to different subtypes, and vaccine effectiveness against circulating subtypes.
Vaccination will play a key role in preventing hospital admissions due to influenza during the respiratory season. Experts estimate, with moderate confidence, that effectiveness of the seasonal influenza vaccine against hospitalization will likely be between 33% and 50%—within the range of vaccine effectiveness observed in recent seasons. Experts estimate the vaccine will likely be between 42% and 55% for adults 18 and older, which we have designated as low and high vaccine uptake, respectively. Assuming a vaccine effectiveness of 41%C modeling estimates that 21% of hospitalizations would be prevented with high vaccine uptake compared to a scenario without any vaccine uptake, while 16% would be prevented with low vaccine uptake.
RSV outlook
CDC projects that the peak weekly hospitalization rate across all age groups due to RSV will be similar to or lower than that of the 2023-2024 season level of 4.2 weekly laboratory-confirmed hospitalizations per 100,000, with moderate confidence. We expect the RSV season to fall within normal seasonal patterns.
Early uptake of new RSV vaccines and immunizations will play a key role in preventing hospital admissions due to RSV during the respiratory season. Experts estimate, with moderate confidence, that for older adults, effectiveness of RSV vaccination against hospitalization will likely be between 73% and 88%, and that uptake of the vaccines will likely be up to 35%. Assuming a vaccine effectiveness of 80% for adults 65 and overD, modeling indicates 25% of hospitalizations of older adults would be prevented with high vaccine uptake, compared to a scenario without any vaccine uptake, while 19% would be prevented with low vaccine uptakeE.
To consider the role of immunization in preventing hospitalizations of infants less than one year old, experts estimated, with moderate confidence, effectiveness and uptake of RSV immunization (nirsevimab) and maternal RSV vaccinationF. Assuming an RSV immunization effectiveness of 90% and a maternal RSV vaccination effectiveness of 64%D, modeling indicates 76% of hospitalizations of infants would be prevented with high uptake, compared to a scenario without any uptake, while 43% would be prevented with low uptake.
Our Behind the Model article features more detail on our modeling methods.
Key Uncertainties & Methods
This outlook is a high-level assessment intended to provide scenarios for how the 2024-2025 respiratory season could unfold; it is not a precise forecast. We have noted several areas of uncertainty for specific diseases in sections above, including related to vaccination and circulating viral variants and subtypes. Additional uncertainties include the following:
- It is difficult to predict the size and timing of peak activity for each disease, as well as how the timing might overlap. Experts agree that some level of overlap in peak hospitalization burden may occur. These factors will affect the level of demand on the healthcare system. We note that while peak hospitalization rate is a key factor, cumulative burden can also impact hospital demand throughout the season.
- The virus that causes COVID-19 is constantly changing, and a new variant could emerge that is less effectively mitigated by immunity from past infections or from existing vaccines and treatments. COVID-19 occurs at meaningful levels throughout the year with periodic epidemics, which can vary in timing and magnitude.
- Avian influenza A (H5N1) is widespread in wild birds globally and is causing outbreaks in poultry and U.S. dairy cows, with several recent human cases in U.S. dairy and poultry workers. The current risk to the general public posed by the avian influenza A (H5N1) virus presently spreading in cows, poultry, and other mammals remains low.
- Particularly for RSV, estimates are less precise for the burden of illnesses and hospitalizations in past seasons which limits our ability to anticipate trends for this respiratory season. Immunization uptake is also less certain because RSV immunization for older adults, for pregnant people, and for infants and young children were recommended last year for the first time.
This outlook is based on expert opinion, historical data, and scenario modeling for COVID-19, influenza, and RSV. We have low to moderate combined confidence in our assessment.
This respiratory outlook incorporates expert opinion from 19 subject-matter experts specializing in COVID-19, influenza, and RSV epidemiology, infectious disease modeling, disease surveillance, and risk assessment methods. In partnership with Metaculus, CDC designed a questionnaire and process for soliciting views from experts on the upcoming fall and winter respiratory season. Experts each answered a series of questions on the expected hospitalization burden posed by each disease, as well as on key drivers for a season with a higher peak hospitalization rate. After experts submitted initial responses to the questionnaire, CDC and Metaculus convened a workshop to discuss results and any key areas of disagreement. Experts were then allowed to update their responses, if desired. The final results were used to inform this Respiratory Disease Season Outlook and as inputs into scenario modeling.
Our Behind the Model article features more detail on our modeling methods.
- Weekly hospitalization rate of 7.8 hospitalizations per 100,000 reported by COVID-NET and 10.8 hospitalizations per 100,000 reported by NHSN (Figure 2)
- NHSN data reporting requirements changed on April 27, 2024, necessitating that we infer hospitalization rates through other, indirect data sources: NSSP nationwide emergency department visits and COVID-19 hospitalization surveillance network data (COVID-NET) from a subset of hospitals nationwide.
- Experts were asked to estimate a 50% confidence interval for influenza vaccine effectiveness against hospitalization during the 2024-2025 respiratory season. The aggregate vaccine effectiveness estimates were calculated as the medians of the lower and upper bounds provided by experts. We used the midpoint (41%) of the median lower bound and median upper bound as an input for our scenario modeling.
- Experts were asked to estimate a 50% confidence interval for RSV vaccine effectiveness against hospitalization during the 2024-2025 respiratory season. The aggregate vaccine effectiveness estimates were calculated as the medians of the lower and upper bounds provided by experts. We used the midpoint of the median lower bound and median upper bound as an input for our scenario modeling.
- We used a vaccine uptake value of 24% for the low uptake scenario, to align with RSV vaccination uptake for older adults during the 2023-2024 respiratory season (24%).
- Experts estimate, with moderate confidence, that for infants, effectiveness of RSV immunization (nirsevimab) against hospitalization will likely be between 85% and 95%, and that uptake of immunization will likely be between 38% and 63%. In addition, experts estimate that effectiveness of maternal RSV vaccination against hospitalization for infants within 3 months of birth will likely be between 55% and 74% and that uptake of vaccination for eligible pregnant persons will be between 15% and 30%.
- Figure 1: Data are from RESP-NET.
