At a glance

Why get vaccinated?
Recombinant zoster (shingles) vaccine can prevent shingles.
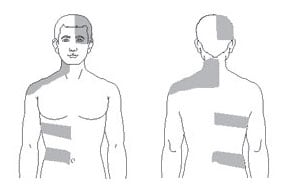
Shingles (also called herpes zoster, or just zoster) is a painful skin rash, usually with blisters. In addition to the rash, shingles can cause fever, headache, chills, or upset stomach. Rarely, shingles can lead to complications such as pneumonia, hearing problems, blindness, brain inflammation (encephalitis), or death.
The risk of shingles increases with age. The most common complication of shingles is long-term nerve pain called postherpetic neuralgia (PHN). PHN occurs in the areas where the shingles rash was and can last for months or years after the rash goes away. The pain from PHN can be severe and debilitating.
The risk of PHN increases with age. An older adult with shingles is more likely to develop PHN and have longer lasting and more severe pain than a younger person.
People with weakened immune systems also have a higher risk of getting shingles and complications from the disease.
Shingles is caused by varicella-zoster virus, the same virus that causes chickenpox. After you have chickenpox, the virus stays in your body and can cause shingles later in life. Shingles cannot be passed from one person to another, but the virus that causes shingles can spread and cause chickenpox in someone who has never had chickenpox or has never received chickenpox vaccine.
Recombinant shingles vaccine
Recombinant shingles vaccine provides strong protection against shingles. By preventing shingles, recombinant shingles vaccine also protects against PHN and other complications.
Recombinant shingles vaccine is recommended for:
- Adults 50 years and older
- Adults 19 years and older who have a weakened immune system because of disease or treatments
Shingles vaccine is given as a two-dose series. For most people, the second dose should be given 2 to 6 months after the first dose. Some people who have or will have a weakened immune system can get the second dose 1 to 2 months after the first dose. Ask your health care provider for guidance.
People who have had shingles in the past and people who have received varicella (chickenpox) vaccine are recommended to get recombinant shingles vaccine. The vaccine is also recommended for people who have already gotten another type of shingles vaccine, the live shingles vaccine. There is no live virus in recombinant shingles vaccine.
Shingles vaccine may be given at the same time as other vaccines.
Talk with your health care provider
Tell your vaccination provider if the person getting the vaccine:
- Has had an allergic reaction after a previous dose of recombinant shingles vaccine, or has any severe, life-threatening allergies
- Is currently experiencing an episode of shingles
- Is pregnant
In some cases, your health care provider may decide to postpone shingles vaccination until a future visit.
People with minor illnesses, such as a cold, may be vaccinated. People who are moderately or severely ill should usually wait until they recover before getting recombinant shingles vaccine.
Your health care provider can give you more information.
Risks of a vaccine reaction
- A sore arm with mild or moderate pain is very common after recombinant shingles vaccine. Redness and swelling can also happen at the site of the injection.
- Tiredness, muscle pain, headache, shivering, fever, stomach pain, and nausea are common after recombinant shingles vaccine.
These side effects may temporarily prevent a vaccinated person from doing regular activities. Symptoms usually go away on their own in 2 to 3 days. You should still get the second dose of recombinant shingles vaccine even if you had one of these reactions after the first dose.
Guillain-Barré syndrome (GBS), a serious nervous system disorder, has been reported very rarely after recombinant zoster vaccine.
People sometimes faint after medical procedures, including vaccination. Tell your provider if you feel dizzy or have vision changes or ringing in the ears.
As with any medicine, there is a very remote chance of a vaccine causing a severe allergic reaction, other serious injury, or death.
What if there is a serious problem?
An allergic reaction could occur after the vaccinated person leaves the clinic. If you see signs of a severe allergic reaction (hives, swelling of the face and throat, difficulty breathing, a fast heartbeat, dizziness, or weakness), call 9-1-1 and get the person to the nearest hospital.
For other signs that concern you, call your health care provider.
Adverse reactions should be reported to the Vaccine Adverse Event Reporting System (VAERS). Your health care provider will usually file this report, or you can do it yourself. Visit the VAERS website or call 1-800-822-7967. VAERS is only for reporting reactions, and VAERS staff members do not give medical advice.
How can I learn more?
- Ask your health care provider.
- Call your local or state health department.
- Visit the website of the Food and Drug Administration (FDA) for vaccine package inserts and additional information.
- Contact the Centers for Disease Control and Prevention (CDC):
- Call 1-800-232-4636 (1-800-CDC-INFO) or
- Visit CDC's vaccines website.
- Call 1-800-232-4636 (1-800-CDC-INFO) or

