At a glance
There are two pathways for emergency response employees to be notified about exposure to potentially life-threatening infectious diseases: routine notification by the medical facility, and a request initiated by the employee. There is also an alternate pathway for special circumstances.

Overview
Notifications about emergency response employeeA (ERE) exposure can occur in one of two ways:
(1) The medical facility determines that the victim of an emergency has a potentially life-threatening airborne or aerosolized infectious disease about which the ERE who transported the victim to the medical facility should be notified, or
(2) The ERE who transported, treated, assisted, or attended a victim pursuant to an emergency believes that they have been exposed to any infectious disease on the NIOSH list and requests information from the medical facility.
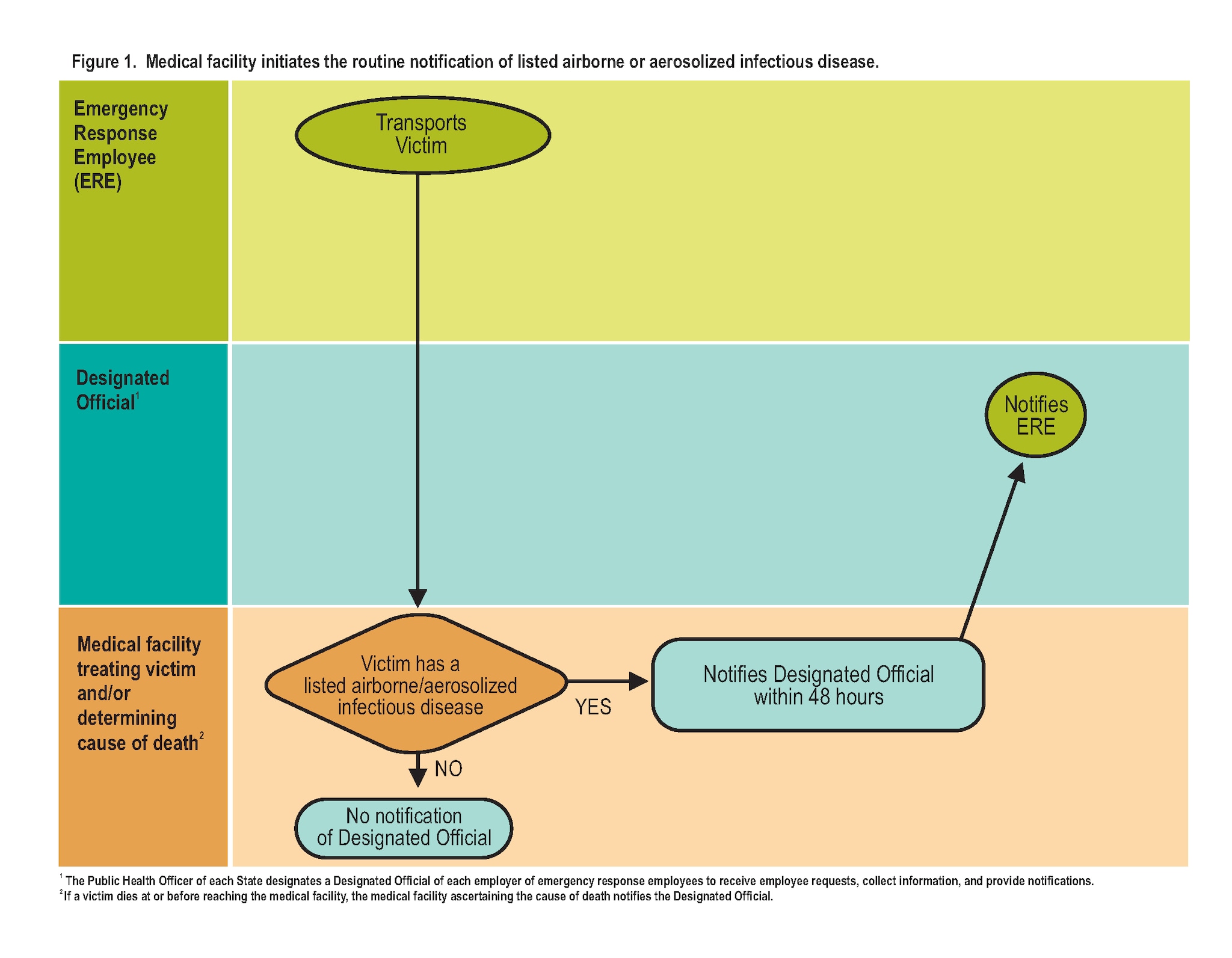
Pathway 1: Medical facility initiates routine notification
The medical facility initiates routine notification if it determines that the victim of an emergency has a potentially life-threatening airborne or aerosolized infectious disease regarding a patient that the ERE transported to the facility.
Steps:
- The medical facility notifies the designated officer of the ERE within 48 hours, providing the name of the infectious disease and the date when the emergency victim was transported by the ERE to the facility.
- The designated officerB informs the ERE immediately.
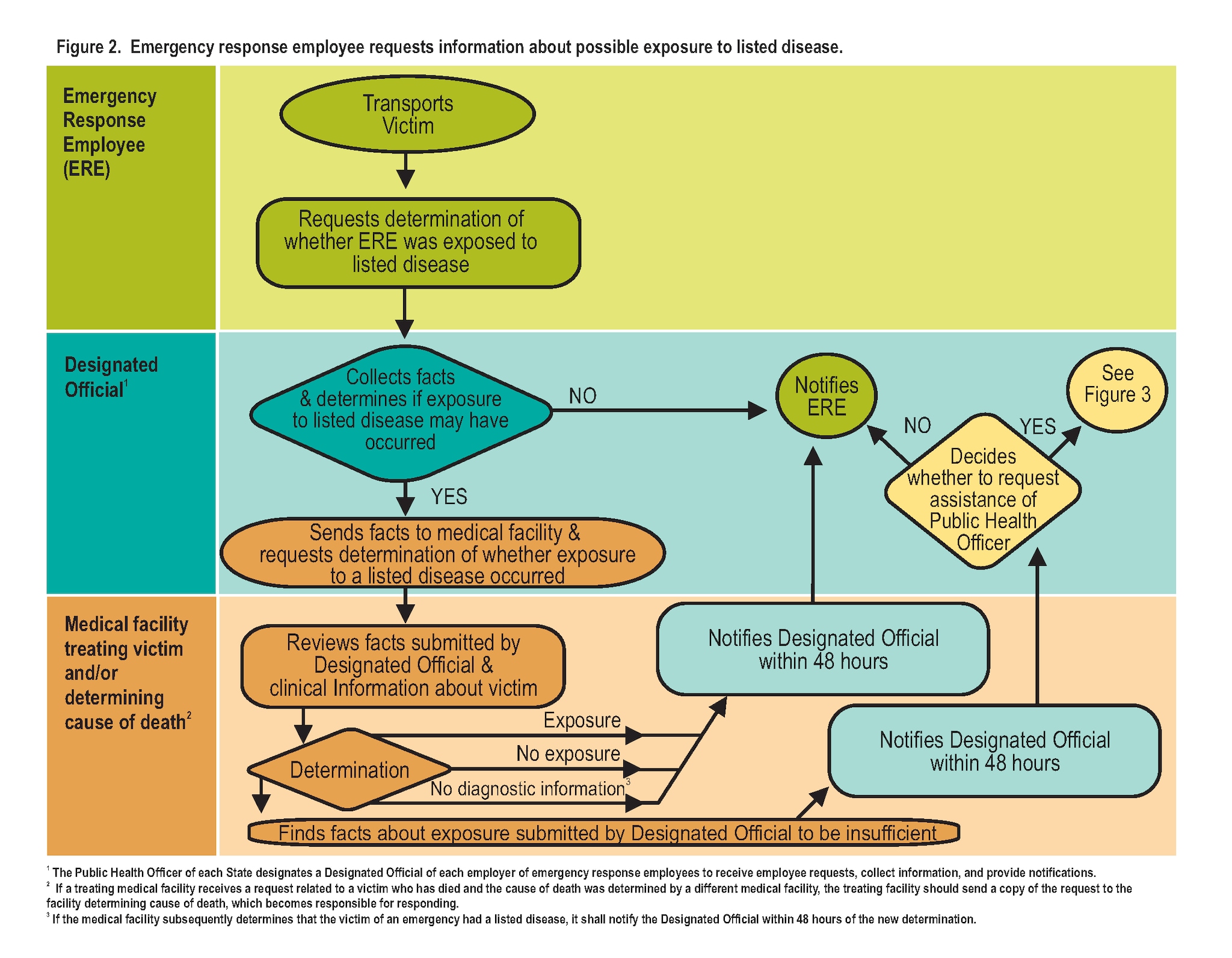
Pathway 2: ERE initiates a request
The ERE initiates a request based on a potential exposure to a listed infectious disease by a victim of an emergency during an emergency (i.e. needlestick injury, other contact with body fluidsC, or suspicion of exposure to an airborne or aerosolizedD infectious disease), only if the victim was transported to a medical facility because of the emergency, and the ERE attended, treated, assisted, or transported the victim pursuant to the emergency.
Steps:
- The ERE submits a request to a designated officer to make an initial determination.
- The request is examined by the designated officer.
- The designated officer determines whether the ERE may have been involved, if the victim involved had any listed infectious disease, in a potential exposure under the facts presented. The designated officer shall make such determination in accordance with the NIOSH guidelines.
- If so, the designated officer submits a written request to the medical facility to which the victim was transported or determined the cause of death.
- Once the medical facility receives the request, it has 48 hours to respond.
- The medical facility reviews their records to determine if the ERE was exposedE to a potentially life-threatening infectious disease.F
- In receiving a request from a designated officer, the medical facility shall
- Evaluate the facts in the request; and
- Make a determination of whether the ERE was exposed to an infectious disease included on NIOSH's List of Potentially Life-Threatening Infectious Diseases to Which Emergency Response Employees May Be Exposed based on the medical information possessed by the facility regarding the victim and in accordance with NIOSH's guidelines.
- The medical facility will make one of four determinations in response to the request:
- Notification of exposure
- Finding of no exposure
- Insufficient information submitted by designated officer — If the medical facility determines that "insufficient information" was provided by the designated officer, the designated officer can request the assistance of the public health officer for the community in which the medical facility is located, see "Special Circumstance" below.
- Possesses no information — If the medical facility finds that it possesses no information on whether the victim has an infectious disease included on NIOSH's list, the medical facility shall send written notification to the designated officer informing him of the insufficiency of such medical information.)
- The medical facility reports this information to the designated officer.
- The designated officer informs the ERE.
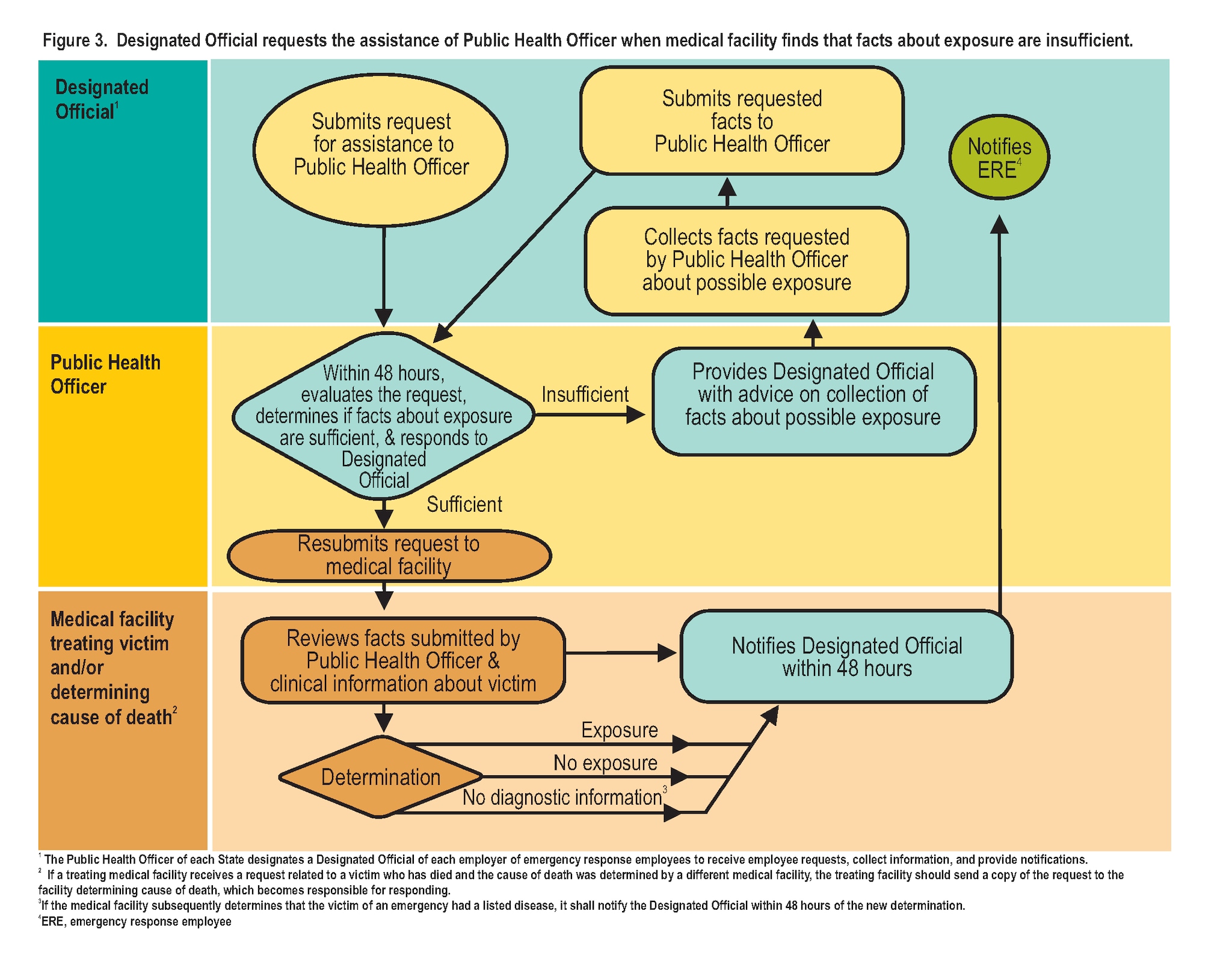
Special circumstances
If the medical facility determines that the designated officer's request has insufficient information, the designated officer may contact the public health officer for assistance.
Steps:
- The designated officer submits a request for assistance to the public health officer for the community in which the medical facility is located for an evaluation of the request and response.
- The public health officer evaluates the request and response, and determines whether the information about the exposure is sufficient.
- The public health officer responds to the designated officer within 48 hours.
- If the information is sufficient, the public health official resubmits the request to the medical facility AND the medical facility shall provide a determination of exposure to the designated officer. The medical facility reviews the request, makes a determination, and notifies the designated officer within 48 hours.
- The designated officer informs the ERE.
- If the public health officer determines the information is not sufficient, the public health official advises the designated officer to collect more information regarding the possible exposure
- The public health officer shall resubmit the request to the medical facility IF sufficient facts are obtained by the designated officer. The medical facility shall then provide a determination regarding exposure to the designated officer.
- Firefighters, law enforcement officers, paramedics, emergency medical technicians, funeral service practitioners, and other individuals (including employees of legally organized and recognized volunteer organizations, without regard to whether such employees receive nominal compensation) who, in the course of professional duties, respond to emergencies in the geographic area involved.
- The Public Health Officer of each state designates a Designated Official of each employer of emergency response employees to receive employee requests, collect information, and provide notifications.
- Person-to-person transmission of an infectious agent through direct or indirect contact with an infected person’s blood or other body fluids.
- Person-to-person transmission of an infectious agent by an aerosol of small particles able to remain airborne for long periods of time. These can transmit diseases on air currents over long distances, cause prolonged airspace contamination, and can be inhaled into the trachea and lung.
- To be in circumstances in which there is recognized risk for transmission of an infectious agent from a human source to an ERE or, in the case of a Select Agent, from a surface or environment contaminated by the agent to an ERE.
- An infectious disease to which EREs may be exposed and that has reasonable potential to cause death or fetal mortality in either healthy EREs or in EREs who are able to work but take medications or are living with conditions that might impair host defense mechanisms.
