HIV Declines Among Young People and Drives Overall Decrease in New HIV Infections
CDC has paused PrEP coverage reporting to determine the best methodology for calculating PrEP coverage, and to update PrEP coverage estimates using updated methods and sources. Due to a formula error that affects a subset of race/ethnicity data, all race/ethnicity data have been removed from this page. CDC plans to resume PrEP coverage reporting in the next HIV Monitoring Report for all demographic groups, currently scheduled for publication in June 2025. Until updated PrEP coverage estimates are published, CDC advises against citing specific PrEP coverage data points, as historical estimates will be updated.
For immediate release: Tuesday, May 23, 2023
Contact: CDC Media Relations
Increased investments, innovation, and focus on equity are vitally needed to end the HIV epidemic
Estimated annual new HIV infections were 12% lower in 2021 compared to 2017—dropping from about 36,500 infections to about 32,100—according to new CDC data published today. The decline was driven by a 34% decrease in new infections among 13- to 24-year-olds, mostly among gay and bisexual males. HIV prevention efforts must go further and progress must be faster, however, for gains to reach populations equitably and for national goals to end the HIV epidemic to be reached.
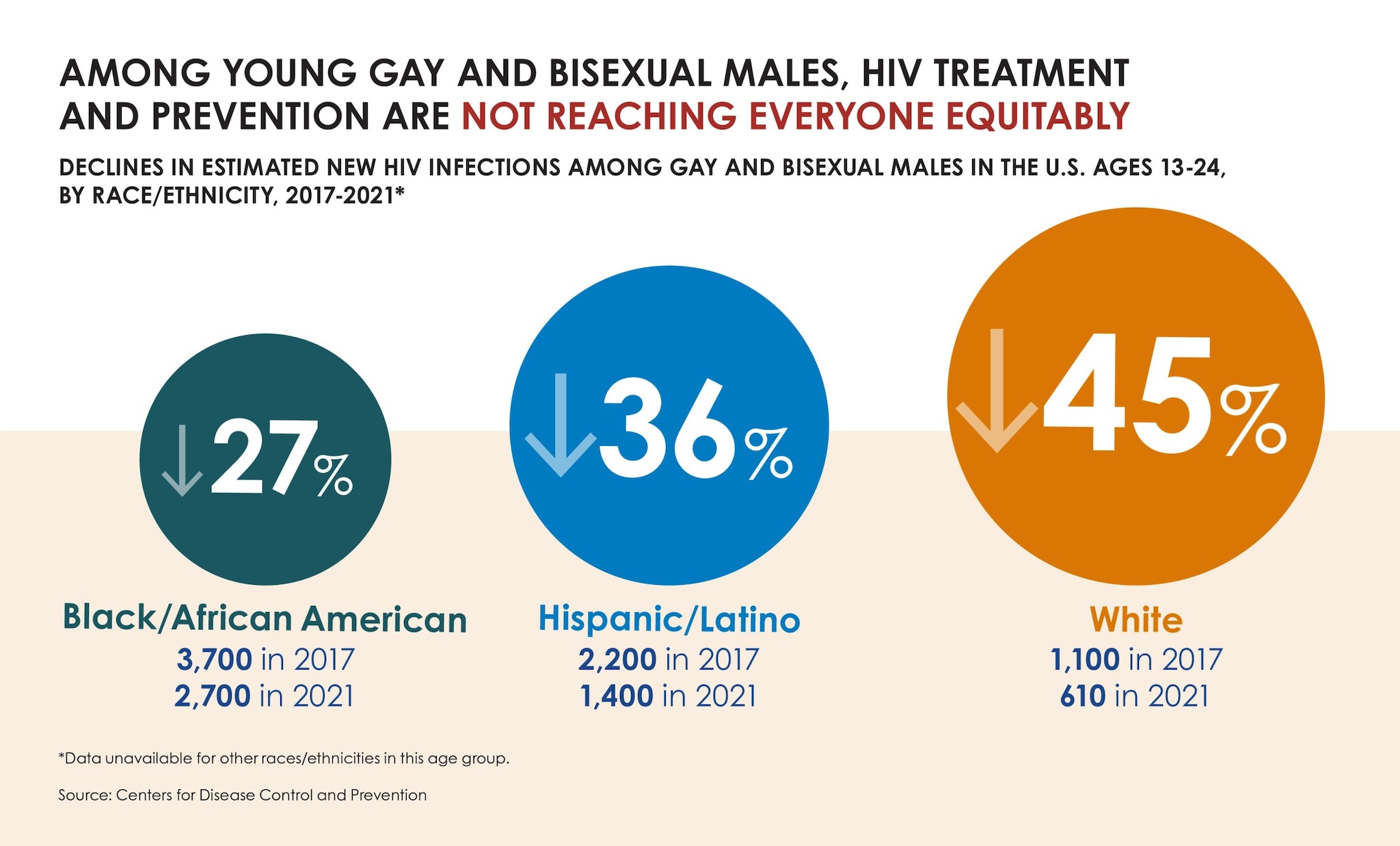
According to CDC’s latest estimates, annual HIV infections dropped from 9,300 in 2017 to 6,100 in 2021 among 13- to 24-year-olds. Declines among young gay and bisexual males (who account for roughly 80% of new infections in this age group) drove the trend, falling from an estimated 7,400 infections to about 4,900 during the timeframe.
“Our nation’s HIV prevention efforts continue to move in the right direction,” said CDC Director Rochelle P. Walensky, M.D., M.P.H. “Longstanding factors, such as systemic inequities, social and economic marginalization and residential segregation, however, stand between highly effective HIV treatment and prevention and people who could benefit from them. Efforts must be accelerated and strengthened for progress to reach all groups faster and equitably.”
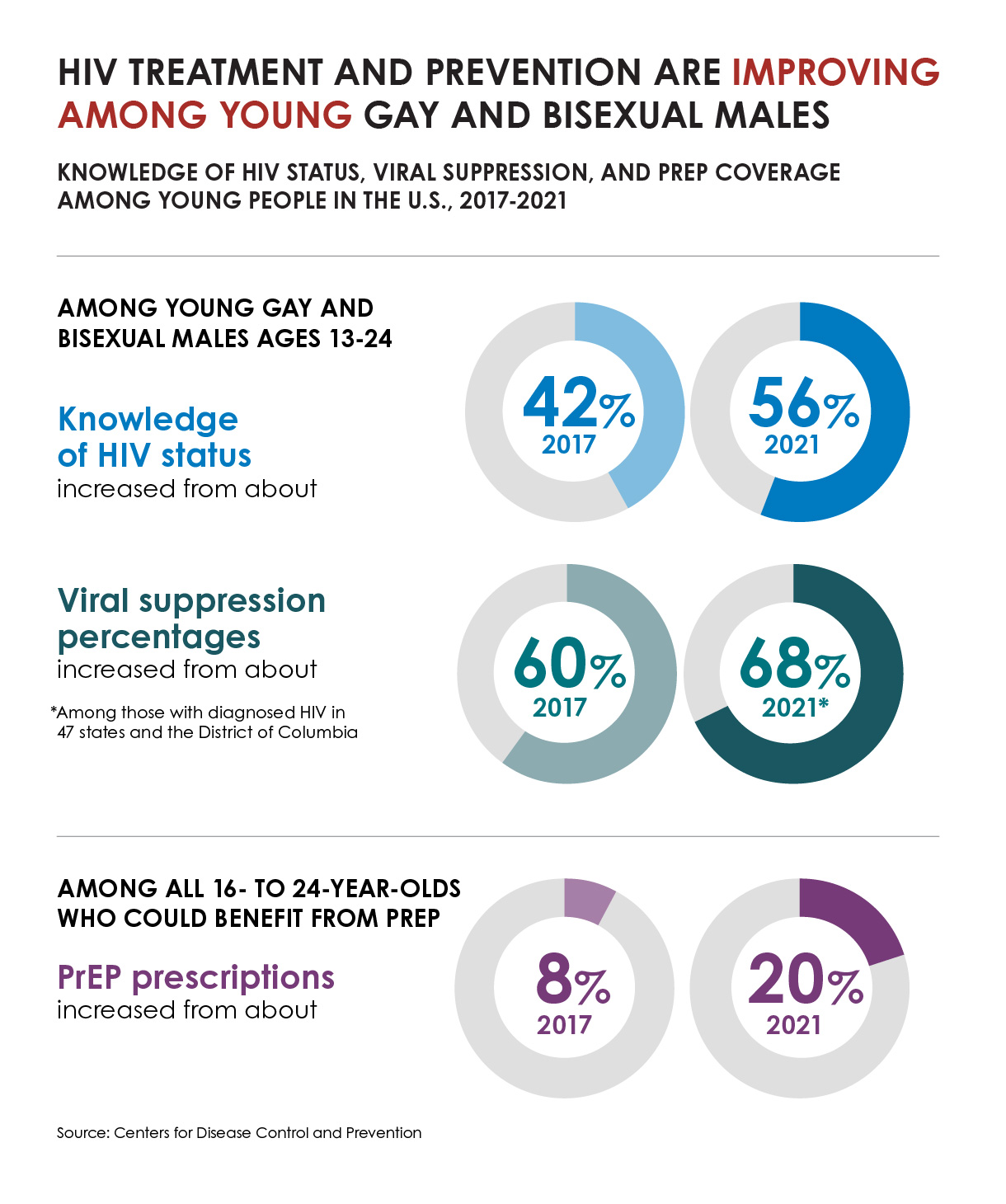
Data suggest that improved reach of HIV testing, treatment, and pre-exposure prophylaxis (PrEP) has contributed to progress in HIV prevention among young gay and bisexual males.
“In prevention, patience is not a virtue.” said Jonathan Mermin, M.D., M.P.H., Director of CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention. “Decreasing HIV incidence among youth, including young gay and bisexual males, shows us what is possible. But ending the HIV epidemic and achieving equity requires we expand this progress to all.”
HIV PrEP and treatment outcomes improve, though longstanding factors limit gains among Black people and Hispanic/Latino people.
The decline in annual HIV infections among young gay and bisexual males was not even across all racial and ethnic groups. Declines were lower among young Black/African American (subsequently, Black) and 13- to 24-year-old Hispanic/Latino gay and bisexual males than young White gay and bisexual males, suggesting that HIV prevention and treatment are not reaching everyone in this group equitably—and reflecting broader disparities that hinder HIV prevention.
Among key HIV prevention indicators, the greatest improvement was in the number of people taking PrEP to prevent HIV. In 2021, about 30% of the 1.2 million people who could benefit from PrEP were prescribed it—a notable improvement compared to about 13% prescribed PrEP in 2017. However, although most people who could benefit from PrEP are Black or Hispanic/Latino people, estimates suggest relatively few Black people or Hispanic/Latino people were prescribed PrEP in 2021.
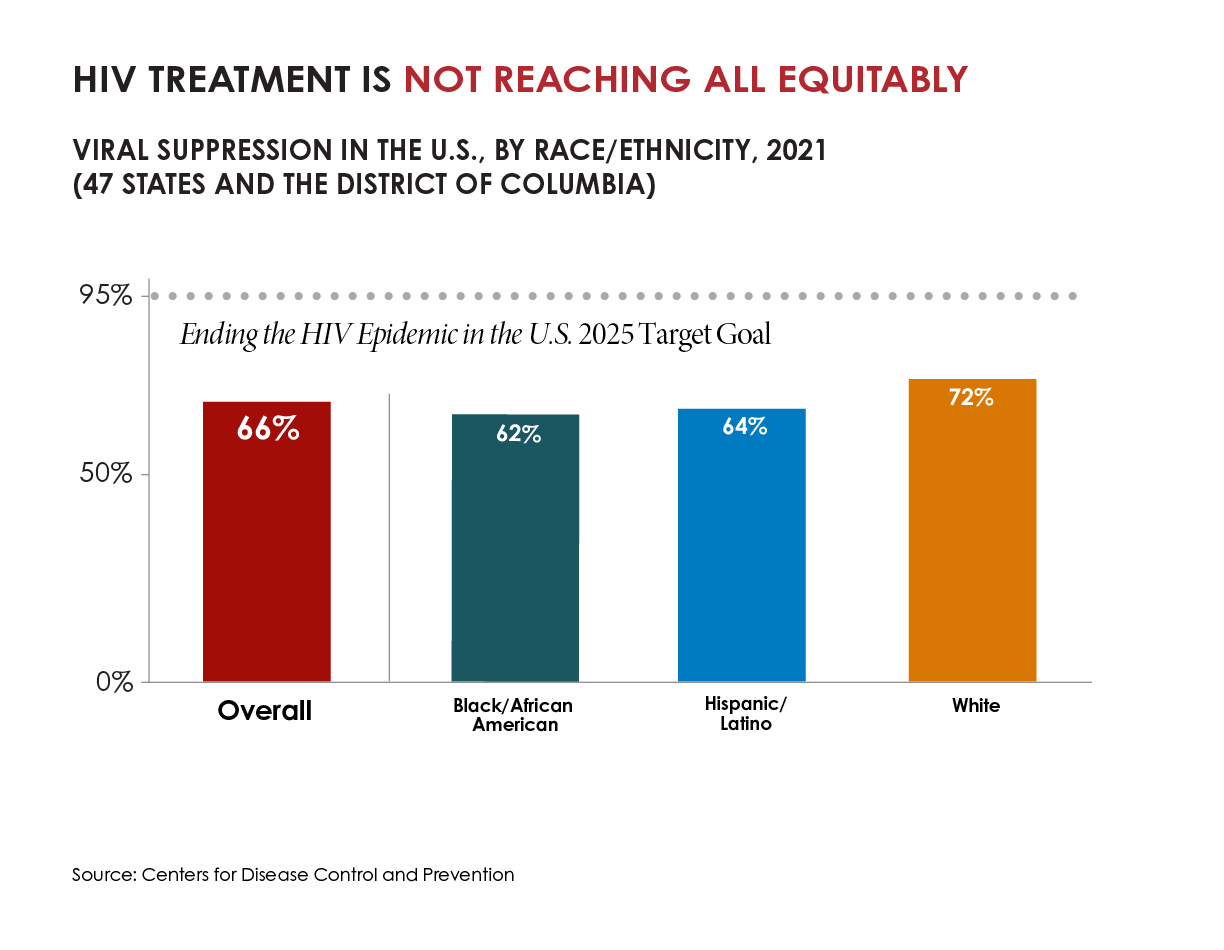
There were also small increases in other key prevention measures, but not at the pace needed to reach national goals. More people with HIV were aware of their status in 2021 than 2017, with an uptick from 86% to 87%. Though data aren’t directly comparable due to reporting differences, the portion of people with diagnosed HIV who were virally suppressed due to effective treatment was slightly higher in 2021 than in 2017, up from 63% to 66%. Viral suppression was lower among Black people and Hispanic/Latino people than White people.
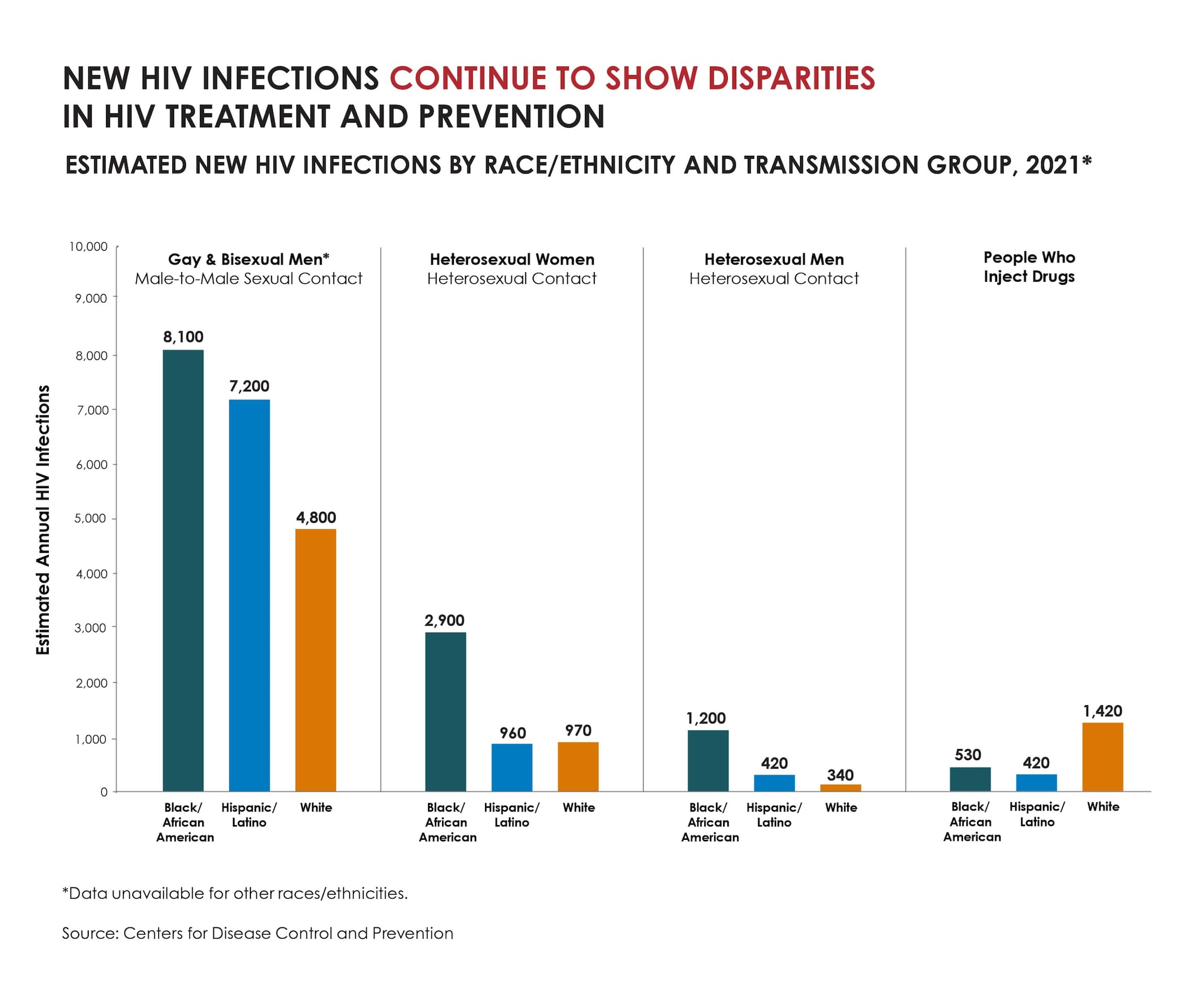
Deeply entrenched social determinants of health continue to drive these disparities and their outcomes. Most new HIV infections in 2021 were among gay and bisexual men, the majority of whom were Black or Hispanic/Latino. About one-fifth of new HIV infections in 2021 were among women, and over half of those were among Black women.
“At least three people in the U.S. get HIV every hour—at a time when we have more effective prevention and treatment options than ever before,” said Robyn Neblett Fanfair, M.D., M.P.H., Acting Director of CDC’s Division of HIV Prevention. “These tools must reach deep into communities and be delivered faster to expand progress from some groups to all groups.”
To realize this goal and end the HIV epidemic, we must:
- Increase investments in proven HIV prevention programs through the Ending the HIV Epidemic in the U.S. (EHE) initiative.
- Maximize innovations by expanding HIV self-testing and growing the number and type of settings to reach people with HIV services, like STI clinics.
- Center equity in every aspect of our work so that HIV prevention interventions better reach people who are disproportionately affected by HIV.
Tools to end the HIV epidemic in the U.S. are available now, but our nation will not succeed until they equitably reach the people who need them to stay healthy.
- As of 2021, 1.2 million people in the United States have HIV, and that 87% of them had received a diagnosis. This means that 1 of 8 people with HIV in the United States do not know they have it.
- About two-thirds of new HIV infections in 2021 were among gay and bisexual men. By age, most (9,100) of those were among 25- to 34-year-olds; followed by 13- to 24-year-olds (4,900); and 35- to 44-year-olds (4,000).
- More than half (52%) of new HIV infections in 2021 were in the U.S. South. The U.S. South was also the only region with a decline in overall estimated new infections in 2021 when compared to 2017 (down 12%).
- 16,700 in the South
- 6,600 in the West
- 4,400 in the Northeast
- 4,400 in the Midwest
- The United States made remarkable strides in eliminating perinatal HIV between 2010 and 2019.In 2021, the downward trend continued with 0.6 cases of perinatal HIV per 100,000 live births, down from the 2010 rate of 1.9 cases per 100,000 live births.
- The U.S. Department of Health and Human Services coordinates the federal Ending the HIV Epidemic in the U.S. (EHE) initiative, which aims to reduce new HIV infections by 90% from 2017 levels by 2030. Early challenges, including resource allocation and the arrival of the COVID-19 pandemic in 2020 (the first year of EHE implementation nationwide) have hindered desired pace toward U.S. goals. The FY24 President’s Budget requested $850 million in funding across CDC, HRSA, IHS, and NIH to support continued EHE scale-up and implementation. This represents a $277 million (48%) increase over the FY23 enacted funding level. The President’s Budget also proposed $237 million for a national PrEP program. These are critical resources to help propel the nation’s HIV prevention efforts forward.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
CDC works 24/7 protecting America’s health, safety, and security. Whether disease start at home or abroad, are curable or preventable, chronic or acute, or from human activity or deliberate attack, CDC responds to America’s most pressing health threats. CDC is headquartered in Atlanta and has experts located throughout the United States and the world.