Key points
- Mumps disease is caused by a paramyxovirus and can be prevented by vaccination.
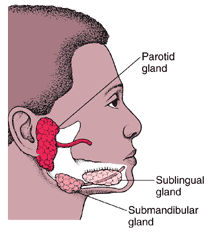
- Common clinical features include parotitis (swollen salivary glands in cheek and jaw area) and fever.
- Mumps spreads through direct contact with saliva or respiratory droplets.
- Isolate infected patients until 5 days after the onset of parotitis.

Clinical features
Mumps is a viral illness caused by a paramyxovirus, a member of the Rubulavirus family.
Mumps usually involves pain, tenderness, and swelling in one or both parotid salivary glands (cheek and jaw area). Swelling usually peaks in 1 to 3 days and then subsides during the next week. The swollen tissue pushes the angle of the ear up and out. Often, the jawbone cannot be felt because of swelling of the parotid.
Severe complications caused by the virus include cerebellar ataxia, encephalitis, viral pneumonia, and hemorrhagic conditions.
Incubation period
The average incubation period for mumps is 16 to 18 days, with a range of 12 to 25 days.
How it spreads
The mumps virus replicates in the upper respiratory tract and is transmitted person to person through direct contact with saliva or respiratory droplets of a person infected with mumps. The risk of spreading the virus increases the longer and closer the contact a person has with someone who has mumps.
The infectious period is considered from 2 days before to 5 days after parotitis onset, although virus has been isolated from saliva as early as 7 days prior to and up to 9 days after parotitis onset. Mumps virus has also been isolated up to 14 days in urine and semen.
Disease rates
Prior to vaccinae introduction:
Before the U.S. mumps vaccination program started in 1967, about 186,000 cases were reported each year, and many more unreported cases occurred. The disease caused complications, such as permanent deafness in children, and occasionally, encephalitis, which could rarely result in death.
Post-vaccine era:
Following the implementation of the routine two-dose MMR vaccination policy, there was a 99% decrease in U.S. mumps cases; with just a few hundred cases reported each year by the early 2000s.
However, starting in 2006 there has been an increase in mumps cases with several peak years. From year to year, the number of mumps cases can range from roughly a couple hundred to several thousand.
The majority of cases and outbreaks occur among people who are fully vaccinated and in close-contact or congregate settings.
Prevention
Mumps can be prevented with mumps-containing vaccine. Mumps vaccine is usually administered in the combination measles, mumps, and rubella (MMR) vaccine. The combination measles, mumps, rubella, and varicella (MMRV) vaccine can be used for children aged 12 months through 12 years.
CDC recommends children get 2 doses of MMR vaccine. Teens and adults should also be up to date on their MMR vaccination. ACIP recommends a third dose of MMR vaccine for people at increased risk of acquiring mumps in an outbreak.
Mumps transmission in healthcare settings is not common. However, transmission has occurred in past outbreaks involving hospitals and long-term care facilities housing adolescents and adults.
Diagnosis and laboratory testing
RT-PCR and viral culture are used to confirm mumps infection. Buccal swabs are most commonly used for RT-PCR testing, but urine and cerebrospinal fluid may also be used in specific situations.
IgM serology can also be used to aid in diagnosing mumps infection. A patient's vaccination status and timing of specimen collection are important for interpreting laboratory results. A negative test result does not rule out mumps infection.
Other tools
Mumps during pregnancy
Mumps that occurs in pregnant women is generally benign and not more severe than in people who are not pregnant. Like other infections, there is a theoretical risk that mumps during the early months of pregnancy may cause complications.
Most studies on the effects of gestational mumps on the fetus were conducted in the 1950s–60s when the disease was more common before mumps vaccine was available. One study from 1966 reported an association between mumps infection during the first trimester of pregnancy and an increase in the rate of spontaneous abortion or intrauterine fetal death,1 but this result has not been observed in other studies.2 One study of low birth weight in relation to mumps during pregnancy found no significant association.1
While there are case reports of congenital malformations in infants born to mothers who had mumps during pregnancy, the only prospective, controlled study found rates of malformations were similar between mothers who had mumps and those who did not have mumps during pregnancy.3
Investigation support
From year to year, the number of U.S. mumps cases can range from a couple hundred to a couple thousand. Some years have more cases than usual because of large outbreaks.
When mumps cases or an outbreak occur, state and local health departments have the lead in investigating the outbreak.
CDC helps and supports health departments in these outbreak investigation by:
- Providing technical assistance to public health officials from states with reported mumps cases.
- Gathering data reported by states on confirmed mumps cases and evaluating and monitoring these data from a national perspective.
- Testing clinical specimens from people suspected to have mumps when requested by states.
- Providing technical assistance on mumps laboratory testing.
- Testing for and tracking changes in the mumps virus strains circulating in the United States.
- Providing rapid assistance on the ground during outbreak investigations, often through a formal request by the state health department.
- Investing in state and local health departments infrastructure and laboratory capacity. This supports front-line response to suspected and confirmed mumps cases.
- Alerting clinicians, healthcare facilities, and public health officials around the country about current outbreaks.
- Providing vaccine policy recommendations, clinical guidance for healthcare providers, and outbreak guidance and materials for health departments.
- Providing information to public and healthcare providers through a variety of media, including the CDC website
Reporting mumps cases
Mumps is a nationally notifiable disease, and all cases should be reported to the state or local health department. Contact your state health department for more information on how to report mumps in your state.
- Siegel M, Fuerst HT, Peress NS. Comparative fetal mortality in maternal virus diseases. A prospective study on rubella, measles, mumps, chicken pox and hepatitis. N Engl J Med 1966;274(14):768-71.
- Wilson CB, Nizet V, Maldonado YA, Remington JS, Klein JO. Remington and Klein's infectious diseases of the fetus and newborn infant. 8th Edition, Elsevier Health Sciences, 2016.
- Siegel M. Congenital malformations following chickenpox, measles, mumps, and hepatitis. Results of a cohort study. JAMA 1973;226(13):1521-4.
