At a glance
- Healthcare providers and health departments can use these flowcharts as a visual tool for following best mumps testing practices.
- Testing procedures include information on specimen type and timing of specimen collection.
Sporadic & outbreak-related mumps testing
Tool to guide testing
Health departments can also request a modifiable version of the job-aid by emailing the CDC Mumps Team. Please include "Mumps Testing Job-Aid" in the subject line. The modifiable version can be edited to include the following:
- Contact information
- Testing and shipping instructions
- Outbreak-specific guidance
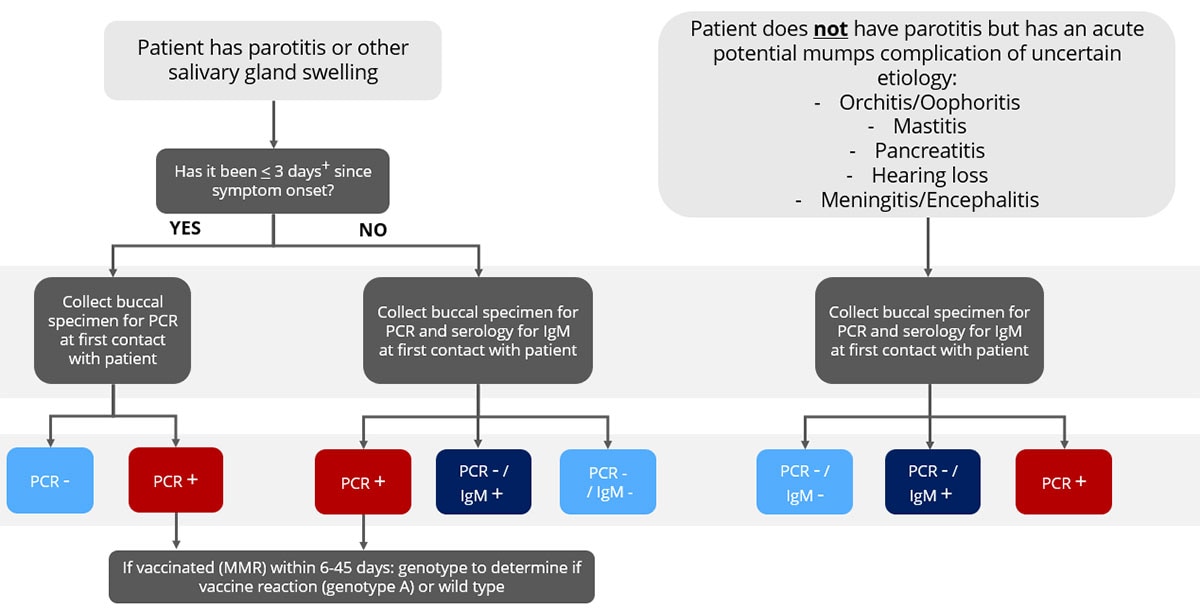
Sporadic (no epidemiologic-link, not outbreak-related) mumps testing flowchart
For persons presenting with symptoms of mumps without known epidemiologic-linkage, multiplex testing for other infectious etiologies is recommended concurrent with mumps testing to better interpret the clinical picture alongside laboratory results.
Consider testing for other infectious etiologies such as influenza, parainfluenza, EBV, & adenovirus that can cause parotitis. If mumps testing is negative and there is a more likely alternative diagnosis with a positive laboratory result, individuals can be classified as not a mumps case.
Additional considerations
- A negative laboratory result in a person with clinically compatible mumps symptoms does not rule out mumps.
- Persons tested for immunologic screening without symptoms would not be considered a case if IgM+ unless there is documentation that mumps was suspected.
For mumps PCR, specimen should be ideally collected 0–3 days after parotitis onset but can be collected up to 10 days. If >10 days since symptom onset, PCR testing no longer recommended. For mumps IgM, collecting specimens >3 days after parotitis onset improves the ability to detect IgM.
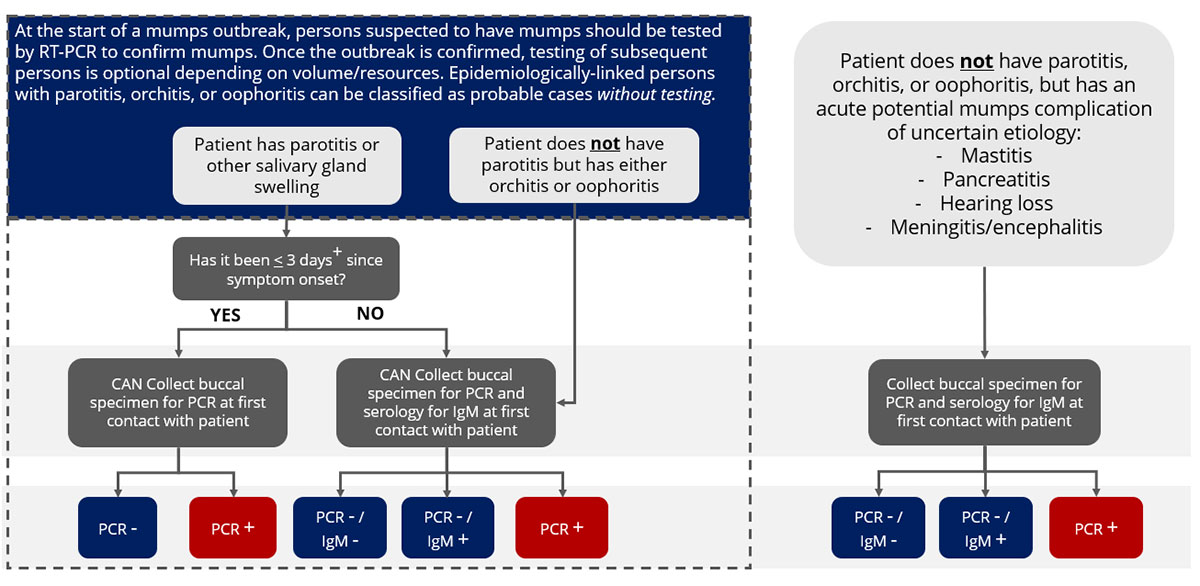
Epidemiologic-link or outbreak-related mumps testing flowchart
Persons being tested have exposure to a confirmed case or linkage to a group/community defined by public health officials during an outbreak of mumps.
Additional considerations
- A negative laboratory result in a person with clinically compatible mumps symptoms does not rule out mumps.
- Persons tested for immunologic screening without symptoms would not be considered a case if IgM+ unless there is documentation that mumps was suspected.
- In an outbreak setting, occasionally asymptomatic or persons with atypical presentation may test PCR +, culture +, or show seroconversion, and would be classified as confirmed cases.
- Parotitis after vaccination has been reported in <1% of vaccinees. If epidemiologically-linked/outbreak-associated cases recently received dose of MMR, genotyping can be done to confirm if vaccine strain
For mumps PCR, specimen should be ideally collected 0–3 days after parotitis onset but can be collected up to 10 days. If >10 days since symptom onset, PCR testing no longer recommended. For mumps IgM, collecting specimens >3 days after parotitis onset improves the ability to detect IgM.
Text version of flowcharts
Sporadic (no epidemiologic-link, not outbreak-related) mumps testing flowchart
Scenario 1
Top of chart “Patient has parotitis or other salivary gland swelling"
Then question: "Has it been ≤ 3 days+ since symptom onset?"
If "Yes", then "Collect buccal specimen for PCR at first contact with patient."
- If PCR - (Classify as suspect case)
- If PCR + (Classify as confirmed case)
- If vaccinated (MMR) within 6–45 days: genotype to determine if vaccine reaction (genotype A) or wild type.
- If vaccinated (MMR) within 6–45 days: genotype to determine if vaccine reaction (genotype A) or wild type.
If "No" Collect buccal specimen for PCR and serology for IgM at first contact with patient."
- If PCR + (Classify as confirmed case)
- If vaccinated (MMR) within 645 days: genotype to determine if vaccine reaction (genotype A) or wild type.
- If vaccinated (MMR) within 645 days: genotype to determine if vaccine reaction (genotype A) or wild type.
- If PCR - / IgM + (Classify as probable case)
- If PCR - / IgM - (Classify as suspect case)
Scenario 2
Top of chart begins "Patient does not have parotitis but has an acute potential mumps complication of uncertain etiology:"
- Orchitis/Oophoritis
- Mastitis
- Pancreatitis
- Hearing loss
- Meningitis/encephalitis
Then Collect buccal specimen for PCR and serology for IgM at first contact with patient.
- If PCR - / IgM - (Classify as suspect case)
- PCR - / IgM + (Classify as probable case)
- PCR + (Classify as confirmed case)
Epidemiologic-link or outbreak-related mumps testing flowchart
Introduction for scenarios 1 and 2 below: At the start of a mumps outbreak, persons suspected to have mumps should be tested by RT-PCR to confirm mumps. Once the outbreak is confirmed, testing of subsequent persons is optional depending on volume/resources. Epidemiologically-linked persons with parotitis, orchitis, or oophoritis can be classified as probable cases without testing.
Scenario 1
Top of chart begins "Patient has parotitis or other salivary gland swelling."
Then Q: "Has it been ≤ 3 days+ since symptom onset?"
If "Yes", then "CAN Collect buccal specimen for PCR at first contact with patient."
- If PCR - (Classify as probable case)
- If PCR + (Classify as confirmed case)
If "No," then "CAN Collect buccal specimen for PCR and serology for IgM at first contact with patient."
- If PCR - / IgM - (Classify as probable case)
- If PCR - / IgM + (Classify as probable case)
- If PCR + (Classify as confirmed case)
Scenario 2
Top of chart begins "Patient does not have parotitis but has either orchitis or oophoritis."
Then "CAN Collect buccal specimen for PCR and serology for IgM at first contact with patient."
- If PCR - / IgM - (Classify as probable case)
- If PCR - / IgM + (Classify as probable case)
- If PCR - (Classify as confirmed case)
Scenario 3
Top of chart begins: "Patient does not have parotitis, orchitis, or oophoritis, but has an acute potential mumps complication of uncertain etiology." Complication includes:
- Mastitis
- Pancreatitis
- Hearing loss
- Meningitis/encephalitis
Then "Collect buccal specimen for PCR and serology for IgM at first contact with patient"
- PCR - / IgM - (Classify as probable case)
- PCR - / IgM + (Classify as probable case)
- PCR + (Classify as confirmed case)
