Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017
Weekly / January 4, 2019 / 67(5152);1419–1427
On December 21, 2018, this report was posted online as an MMWR Early Release.
Lawrence Scholl, PhD1; Puja Seth, PhD1; Mbabazi Kariisa, PhD1; Nana Wilson, PhD1; Grant Baldwin, PhD1 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
The U.S. opioid overdose epidemic continues to evolve. In 2016, 66.4% of the 63,632 drug overdose deaths involved an opioid.
What is added by this report?
In 2017, among 70,237 drug overdose deaths, 47,600 (67.8%) involved opioids, with increases across age groups, racial/ethnic groups, county urbanization levels, and in multiple states. From 2013 to 2017, synthetic opioids contributed to increases in drug overdose death rates in several states. From 2016 to 2017, synthetic opioid-involved overdose death rates increased 45.2%.
What are the implications for public health practice?
Continued federal, state, and local surveillance efforts to inform evidence-based prevention, response, and treatment strategies and to strengthen public health and public safety partnerships are urgently needed.
The 63,632 drug overdose deaths in the United States in 2016 represented a 21.4% increase from 2015; two thirds of these deaths involved an opioid (1). From 2015 to 2016, drug overdose deaths increased in all drug categories examined; the largest increase occurred among deaths involving synthetic opioids other than methadone (synthetic opioids), which includes illicitly manufactured fentanyl (IMF) (1). Since 2013, driven largely by IMF, including fentanyl analogs (2–4), the current wave of the opioid overdose epidemic has been marked by increases in deaths involving synthetic opioids. IMF has contributed to increases in overdose deaths, with geographic differences reported (1). CDC examined state-level changes in death rates involving all drug overdoses in 50 states and the District of Columbia (DC) and those involving synthetic opioids in 20 states, during 2013–2017. In addition, changes in death rates from 2016 to 2017 involving all opioids and opioid subcategories,* were examined by demographics, county urbanization levels, and by 34 states and DC. Among 70,237 drug overdose deaths in 2017, 47,600 (67.8%) involved an opioid.† From 2013 to 2017, drug overdose death rates increased in 35 of 50 states and DC, and significant increases in death rates involving synthetic opioids occurred in 15 of 20 states, likely driven by IMF (2,3). From 2016 to 2017, overdose deaths involving all opioids and synthetic opioids increased, but deaths involving prescription opioids and heroin remained stable. The opioid overdose epidemic continues to worsen and evolve because of the continuing increase in deaths involving synthetic opioids. Provisional data from 2018 indicate potential improvements in some drug overdose indicators;§ however, analysis of final data from 2018 is necessary for confirmation. More timely and comprehensive surveillance data are essential to inform efforts to prevent and respond to opioid overdoses; intensified prevention and response measures are urgently needed to curb deaths involving prescription and illicit opioids, specifically IMF.
Drug overdose deaths were identified in the National Vital Statistics System multiple cause-of-death mortality files,¶ with death certificate data coded using the International Classification of Diseases, Tenth Revision (ICD-10) codes X40–44 (unintentional), X60–64 (suicide), X85 (homicide), or Y10–Y14 (undetermined intent). Among deaths with drug overdose as the underlying cause, the type of drug or drug category is indicated by the following ICD-10 multiple cause-of-death codes: opioids (T40.0, T40.1, T40.2, T40.3, T40.4, or T40.6)**; natural/semisynthetic opioids (T40.2); methadone (T40.3); heroin (T40.1); synthetic opioids other than methadone (T40.4); cocaine (T40.5); and psychostimulants with abuse potential (T43.6).†† Some deaths involved more than one type of drug, and these were included in rates for each drug category; thus, categories are not mutually exclusive.§§
Annual percent change with statistically significant trends in age-adjusted drug overdose death rates¶¶ for all 50 states and DC from 2013 to 2017 and in age-adjusted death rates involving synthetic opioids for 20 states that met drug specificity criteria*** were analyzed using Joinpoint regression.††† Age-adjusted overdose death rates were examined from 2016 to 2017 for all opioids, prescription opioids (5), heroin, and synthetic opioids. Death rates were stratified by age, sex, racial/ethnic group, urbanization level,§§§ and state. State-level analyses included DC and 34 states with adequate drug specificity data for 2016 and 2017.¶¶¶ Analyses comparing changes in death rates from 2016 to 2017 used z-tests when the number of deaths was ≥100 and nonoverlapping confidence intervals based on a gamma distribution when the number was <100.****
Drug overdoses resulted in 70,237 deaths during 2017; among these, 47,600 (67.8%) involved opioids (14.9 per 100,000 population), representing a 12.0% rate increase from 2016 (Table 1). Synthetic opioids were involved in 59.8% of all opioid-involved overdose deaths; the rate increased by 45.2% from 2016 to 2017 (Table 2). From 2013 through 2017, overdose death rates increased significantly in 35 states and DC; 15 of 20 states that met drug specificity criteria had significant increases in overdose death rates involving synthetic opioids (Figure). From 2016 to 2017, death rates involving cocaine and psychostimulants increased 34.4% (from 3.2 to 4.3 per 100,000) and 33.3% (from 2.4 to 3.2 per 100,000), respectively, likely contributing to increases in drug overdose deaths; however, rates remained stable for deaths involving prescription opioids (5.2 per 100,000) (Table 1) and heroin (4.9) (Table 2).
From 2016 to 2017, opioid-involved overdose deaths increased among males and females and among persons aged ≥25 years, non-Hispanic whites (whites), non-Hispanic blacks (blacks), and Hispanics (Table 1). The largest relative change occurred among blacks (25.2%), and the largest absolute rate increase was among males aged 25–44 years (an increase of 4.6 per 100,000). The largest relative change among age groups was for persons aged ≥65 years (17.2%). Counties in medium metro areas experienced the largest absolute rate increase (an increase of 1.9 per 100,000), and the largest relative rate increase occurred in micropolitan counties (14.9%). Death rates increased significantly in 15 states, with the largest relative changes in North Carolina (28.6%), Ohio (19.1%), and Maine (18.7%).
From 2016 to 2017, the prescription opioid-involved death rate decreased 13.2% among males aged 15–24 years but increased 10.5% among persons aged ≥65 years (Table 1). These death rates remained stable from 2016 to 2017 across all racial groups and urbanization levels and in most states, although five states (Maine, Maryland, Oklahoma, Tennessee, and Washington) experienced significant decreases, and one (Illinois) had a significant increase. The largest relative changes included a 29.7% increase in Illinois and a 39.2% decrease in Maine. The highest prescription opioid-involved death rates in 2017 were in West Virginia (17.2 per 100,000), Maryland (11.5), and Utah (10.8).
Heroin-involved overdose death rates declined among many groups in 2017 compared with those in 2016 (Table 2). The largest declines occurred among persons aged 15–24 years (15.0%), particularly males (17.5%), as well as in medium metro counties (6.1%). Rates declined 3.2% among whites. However, heroin-involved overdose death rates did increase among some groups; the largest relative rate increase occurred among persons aged ≥65 years (16.7%) and 55–64 years (11.6%) and among blacks (8.9%). Rates remained stable in most states, with significant decreases in five states (Maryland, Massachusetts, Minnesota, Missouri, and Ohio), and increases in three (California, Illinois, and Virginia). The largest relative decrease (31.9%) was in Ohio, and the largest relative increase (21.8%) was in Virginia. The highest heroin-involved overdose death rates in 2017 were in DC (18.0 per 100,000), West Virginia (14.9), and Connecticut (12.4).
Deaths involving synthetic opioids propelled increases from 2016 to 2017 across all demographic categories (Table 2). The highest death rate was in males aged 25–44 years (27.0 per 100,000), and the largest relative increases occurred among blacks (60.7%) and American Indian/Alaska Natives (58.5%). Deaths increased across all urbanization levels from 2016 to 2017. Twenty-three states and DC experienced significant increases in synthetic opioid-involved overdose death rates, including eight states west of the Mississippi River. The largest relative rate increase occurred in Arizona (122.2%), followed by North Carolina (112.9%) and Oregon (90.9%). The highest synthetic opioid-involved overdose death rates in 2017 were in West Virginia (37.4 per 100,000), Ohio (32.4), and New Hampshire (30.4).
Discussion
In the United States, drug overdoses resulted in 702,568 deaths during 1999–2017, with 399,230 (56.8%) involving opioids.†††† From 2016 to 2017, death rates from all opioids increased, with increases driven by synthetic opioids. Deaths involving IMF have been seen primarily east of the Mississippi River;§§§§ however, recent increases occurred in eight states west of the Mississippi River, including Arizona, California, Colorado, Minnesota, Missouri, Oregon, Texas, and Washington.
Drug overdose death rates from 2013 to 2017 increased in most states; the influence of synthetic opioids on these rate increases was seen in approximately one quarter of all states during this same 5-year period. Overdose deaths involving cocaine and psychostimulants also have increased in recent years (1,6). Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by co-involvement of prescription and illicit drugs (7,8).¶¶¶¶ For example, in 2016, synthetic opioids (primarily IMF) were involved in 23.7% of deaths involving prescription opioids, 37.4% involving heroin, and 40.3% involving cocaine (9). In addition, death rates are increasing across multiple demographic groups. For example, although death rates involving opioids remained highest among whites, relatively large increases across several drug categories were observed among blacks.
The findings in this report are subject to at least five limitations. First, at autopsy, substances tested for vary by time and jurisdiction, and improvements in toxicologic testing might account for some reported increases. Second, the specific types of drugs involved were not included on 15% of drug overdose death certificates in 2016 and 12% in 2017, and the percentage of death certificates with at least one drug specified ranged among states from 54.7%–99.3% in 2017, limiting rate comparisons between states. Third, because heroin and morphine are metabolized similarly (10), some heroin deaths might have been misclassified as morphine deaths, resulting in underreporting of heroin deaths. Fourth, potential race misclassification might have led to underestimates for certain categories, primarily for American Indian/Alaska Natives and Asian/Pacific Islanders.***** Finally, most state-specific analyses were restricted to DC and a subset of states with adequate drug specificity, limiting generalizability.
Through 2017, the drug overdose epidemic continues to worsen and evolve, and the involvement of many types of drugs (e.g., opioids, cocaine, and methamphetamine) underscores the urgency to obtain more timely and local data to inform public health and public safety action. Although prescription opioid- and heroin-involved death rates were stable from 2016 to 2017, they remained high. Some preliminary indicators in 2018 point to possible improvements based on provisional data;††††† however, confirmation will depend on results of pending medical investigations and analysis of final data. Overall, deaths involving synthetic opioids continue to drive increases in overdose deaths. CDC funds 32 states and DC to collect more timely and comprehensive drug overdose data, including improved toxicologic testing in opioid-involved fatal overdoses.§§§§§ CDC is funding prevention activities in 42 states and DC.¶¶¶¶¶ CDC also is leveraging emergency funding to support 49 states, DC, and four territories to broaden their surveillance and response capabilities and enable comprehensive community-level responses with implementation of novel, evidence-based interventions.****** Continued efforts to ensure safe prescribing practices by following the CDC Guideline for Prescribing Opioids for Chronic Pain†††††† are enhanced by access to nonopioid and nonpharmacologic treatments for pain. Other important activities include increasing naloxone availability, expanding access to medication-assisted treatment, enhancing public health and public safety partnerships, and maximizing the ability of health systems to link persons to treatment and harm-reduction services.
Acknowledgment
Rose Rudd, MSPH, Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC.
Corresponding authors: Lawrence Scholl, lzi8@cdc.gov, 404-498-1489; Puja Seth, pseth@cdc.gov, 404-639-6334.
1Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* Natural opioids include morphine and codeine, and semisynthetic opioids include drugs such as oxycodone, hydrocodone, hydromorphone, and oxymorphone. Methadone is a synthetic opioid. Prescription opioids include methadone, natural, and semisynthetic opioids. Synthetic opioids, other than methadone, include drugs such as tramadol and fentanyl. Heroin is an illicit opioid synthesized from morphine that can be a white or brown powder or a black, sticky substance.
† https://www.cdc.gov/nchs/products/databriefs/db329.htm.
§ https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm.
¶ https://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm.
** T40.0 (opium) and T40.6 (other and unspecified narcotics).
†† Psychostimulants with abuse potential include drugs such as methamphetamine and 3,4-methylenedioxy-methamphetamine (MDMA).
§§ For example, a death involving both a synthetic opioid other than methadone and heroin would be included in both the synthetic opioid other than methadone and heroin death rates.
¶¶ Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 U.S. Census standard population age distribution https://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf.
*** State-level analyses for synthetic opioid-involved overdose deaths, comparing death rates from 2013 to 2017, included 20 states that met the following criteria: 1) >80% of drug overdose death certificates named at least one specific drug in 2013–2017; 2) change from 2013 to 2017 in the percentage of death certificates reporting at least one specific drug was <10 percentage points; and 3) ≥20 deaths involving synthetic opioids other than methadone occurred during 2013 and 2017. States whose reporting of any specific drug or drugs involved in an overdose changed by ≥10 percentage points from 2013 to 2017 were excluded because drug-specific overdose numbers and rates might have changed substantially from 2013 to 2017 as a result of changes in reporting.
††† For all analyses, a p-value of <0.05 was considered to be statistically significant. https://surveillance.cancer.gov/joinpoint/.
§§§ Categories of 2013 NCHS Urban-Rural Classification Scheme for Counties (https://www.cdc.gov/nchs/data_access/urban_rural.htm). Large central metro: Counties in metropolitan statistical areas (MSAs) of ≥1 million population that 1) contain the entire population of largest principal city of the MSA, or 2) have their entire population contained in the largest principal city of the MSA, or 3) contain at least 250,000 inhabitants of any principal city of the MSA; Large fringe metro: Counties in MSAs of ≥1 million population that did not qualify as large central metro counties; Medium metro: Counties in MSAs of populations of 250,000–999,999; Small metro: Counties in MSAs of populations <250,000; Micropolitan (nonmetropolitan counties): counties in micropolitan statistical areas; Noncore (nonmetropolitan counties): nonmetropolitan counties that did not qualify as micropolitan.
¶¶¶ State-level analyses comparing death rates from 2016 to 2017 included 34 states and DC that met the following criteria: 1) >80% of drug overdose death certificates named at least one specific drug in 2016 and 2017; 2) change from 2016 to 2017 in the percentage of death certificates reporting at least one specific drug was <10 percentage points; and 3) ≥20 deaths occurred during 2016 and 2017 in at least two opioid subcategories examined. States whose reporting of any specific drug or drugs involved in an overdose changed by ≥10 percentage points from 2016 to 2017 were excluded because drug-specific overdose numbers and rates might have changed substantially from 2016 to 2017 as a result of changes in reporting.
**** Z-tests were used if the number of deaths was ≥100, and a p-value of <0.05 was considered to be statistically significant. Nonoverlapping confidence intervals based on the gamma method were used if the number of deaths was <100 in 2015 or 2016. Note that the method of comparing confidence intervals is a conservative method for statistical significance; caution should be observed when interpreting a nonsignificant difference when the lower and upper limits being compared overlap only slightly.
†††† https://wonder.cdc.gov.
§§§§ https://emergency.cdc.gov/han/han00413.asp.
¶¶¶¶ https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_09-508.pdf.
***** https://www.cdc.gov/nchs/data/series/sr_02/sr02_172.pdf.
††††† https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm.
§§§§§ https://www.cdc.gov/drugoverdose/foa/state-opioid-mm.html.
¶¶¶¶¶ https://www.cdc.gov/drugoverdose/states/state_prevention.html. https://www.cdc.gov/drugoverdose/foa/ddpi.html.
****** https://www.cdc.gov/cpr/readiness/funding-opioid.htm.
†††††† https://www.cdc.gov/drugoverdose/prescribing/guideline.html.
References
- Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep 2018;67:349–58. CrossRef PubMed
- Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013–2014. MMWR Morb Mortal Wkly Rep 2016;65:837–43. PubMed CrossRef
- O’Donnell JK, Gladden RM, Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region—United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66:897–903 10.15585/mmwr.mm6634a2. CrossRef PubMed
- O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 states, July–December 2016. MMWR Morb Mortal Wkly Rep 2017;66:1197–202. CrossRef PubMed
- Seth P, Rudd RA, Noonan RK, Haegerich TM. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 2018;108:500–2. CrossRef PubMed
- McCall Jones C, Baldwin GT, Compton WM. Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health 2017;107:430–2. CrossRef PubMed
- Kandel DB, Hu MC, Griesler P, Wall M. Increases from 2002 to 2015 in prescription opioid overdose deaths in combination with other substances. Drug Alcohol Depend 2017;178:501–11. CrossRef PubMed
- Mattson CL, O’Donnell J, Kariisa M, Seth P, Scholl L, Gladden RM. Opportunities to prevent overdose deaths involving prescription and illicit opioids, 11 states, July 2016–June 2017. MMWR Morb Mortal Wkly Rep 2018;67:945–51. CrossRef PubMed
- Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA 2018;319:1819–21. CrossRef PubMed
- Davis GG; National Association of Medical Examiners and American College of Medical Toxicology Expert Panel on Evaluating and Reporting Opioid Deaths. Complete republication: National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. J Med Toxicol 2014;10:100–6. CrossRef PubMed
Source: National Vital Statistics System, Mortality file.
* Deaths are classified using the International Classification of Diseases, Tenth Revision (ICD–10). Drug overdose deaths are identified using underlying cause-of-death codes X40–X44, X60–X64, X85, and Y10–Y14. Rates are age-adjusted using the direct method and the 2000 U.S. standard population, except for age-specific crude rates. All rates are per 100,000 population.
† Drug overdose deaths, as defined, that have opium (T40.0), heroin (T40.1), natural and semisynthetic opioids (T40.2), methadone (T40.3), synthetic opioids other than methadone (T40.4), or other and unspecified narcotics (T40.6) as a contributing cause.
§ Drug overdose deaths, as defined, that have natural and semisynthetic opioids (T40.2) or methadone (T40.3) as a contributing cause.
¶ Categories of deaths are not exclusive because deaths might involve more than one drug. Summing of categories will result in more than the total number of deaths in a year.
** Data for Hispanic origin should be interpreted with caution; studies comparing Hispanic origin on death certificates and on census surveys have shown inconsistent reporting on Hispanic ethnicity. Potential race misclassification might lead to underestimates for certain categories, primarily American Indian/Alaska Native non-Hispanic and Asian/Pacific Islander non-Hispanic decedents. https://www.cdc.gov/nchs/data/series/sr_02/sr02_172.pdf.
†† By 2013 urbanization classification (https://www.cdc.gov/nchs/data_access/urban_rural.htm).
§§ Analyses were limited to states meeting the following criteria. For states with very good to excellent reporting, ≥90% of drug overdose deaths mention at least one specific drug in 2016, with the change in drug overdose deaths mentioning at least one specific drug differing by <10 percentage points from 2016 to 2017. States with good reporting had 80% to <90% of drug overdose deaths mention at least one specific drug in 2016, with the change in the percentage of drug overdose deaths mentioning at least one specific drug differing by <10 percentage points from 2016 to 2017. States included also were required to have stable rate estimates, based on ≥20 deaths, in at least two drug categories (i.e., opioids, prescription opioids, synthetic opioids other than methadone, and heroin).
¶¶ Absolute rate change is the difference between 2016 and 2017 rates. Percent change is the absolute rate change divided by the 2016 rate, multiplied by 100. Nonoverlapping confidence intervals based on the gamma method were used if the number of deaths was <100 in 2016 or 2017, and z-tests were used if the number of deaths was ≥100 in both 2016 and 2017.
*** Statistically significant (P-value <0.05).
Source: National Vital Statistics System, Mortality file.
* Deaths are classified using the International Classification of Diseases, Tenth Revision (ICD–10). Drug overdose deaths are identified using underlying cause-of-death codes X40–X44, X60–X64, X85, and Y10–Y14. Rates are age-adjusted using the direct method and the 2000 U.S. standard population, except for age-specific crude rates. All rates are per 100,000 population.
† Drug overdose deaths, as defined, that have heroin (T40.1) as a contributing cause.
§ Drug overdose deaths, as defined, that have semisynthetic opioids other than methadone (T40.4) as a contributing cause.
¶ Categories of deaths are not exclusive as deaths might involve more than one drug. Summing of categories will result in more than the total number of deaths in a year.
** Data on Hispanic origin should be interpreted with caution; studies comparing Hispanic origin on death certificates and on census surveys have shown inconsistent reporting on Hispanic ethnicity. Potential race misclassification might lead to underestimates for certain categories, primarily American Indian/Alaska Native non-Hispanic and Asian/Pacific Islander non-Hispanic decedents. https://www.cdc.gov/nchs/data/series/sr_02/sr02_172.pdf.
†† By 2013 urbanization classification (https://www.cdc.gov/nchs/data_access/urban_rural.htm).
§§ Analyses were limited to states meeting the following criteria. For states with very good to excellent reporting, ≥90% of drug overdose deaths mention at least one specific drug in 2016, with the change in drug overdose deaths mentioning at least one specific drug differing by <10 percentage points from 2016 to 2017. States with good reporting had 80% to <90% of drug overdose deaths mention at least one specific drug in 2016, with the change in the percentage of drug overdose deaths mentioning at least one specific drug differing by <10 percentage points from 2016 to 2017. States included also were required to have stable rate estimates, based on ≥20 deaths, in at least two drug categories (i.e., opioids, prescription opioids, synthetic opioids other than methadone, and heroin).
¶¶ Absolute rate change is the difference between 2016 and 2017 rates. Percent change is the absolute rate change divided by the 2016 rate, multiplied by 100. Nonoverlapping confidence intervals based on the gamma method were used if the number of deaths was <100 in 2016 or 2017, and z-tests were used if the number of deaths was ≥100 in both 2016 and 2017. Note that the method of comparing confidence intervals is a conservative method for statistical significance; caution should be observed when interpreting a nonsignificant difference when the lower and upper limits being compared overlap only slightly. Confidence intervals of 2016 and 2017 rates of synthetic opioid-involved deaths in Iowa overlapped only slightly: (1.40, 2.39), (2.36, 3.59).
*** Statistically significant (P-value <0.05).
††† Cells with ≤9 deaths are not reported. Rates based on <20 deaths are not considered reliable and are not reported.
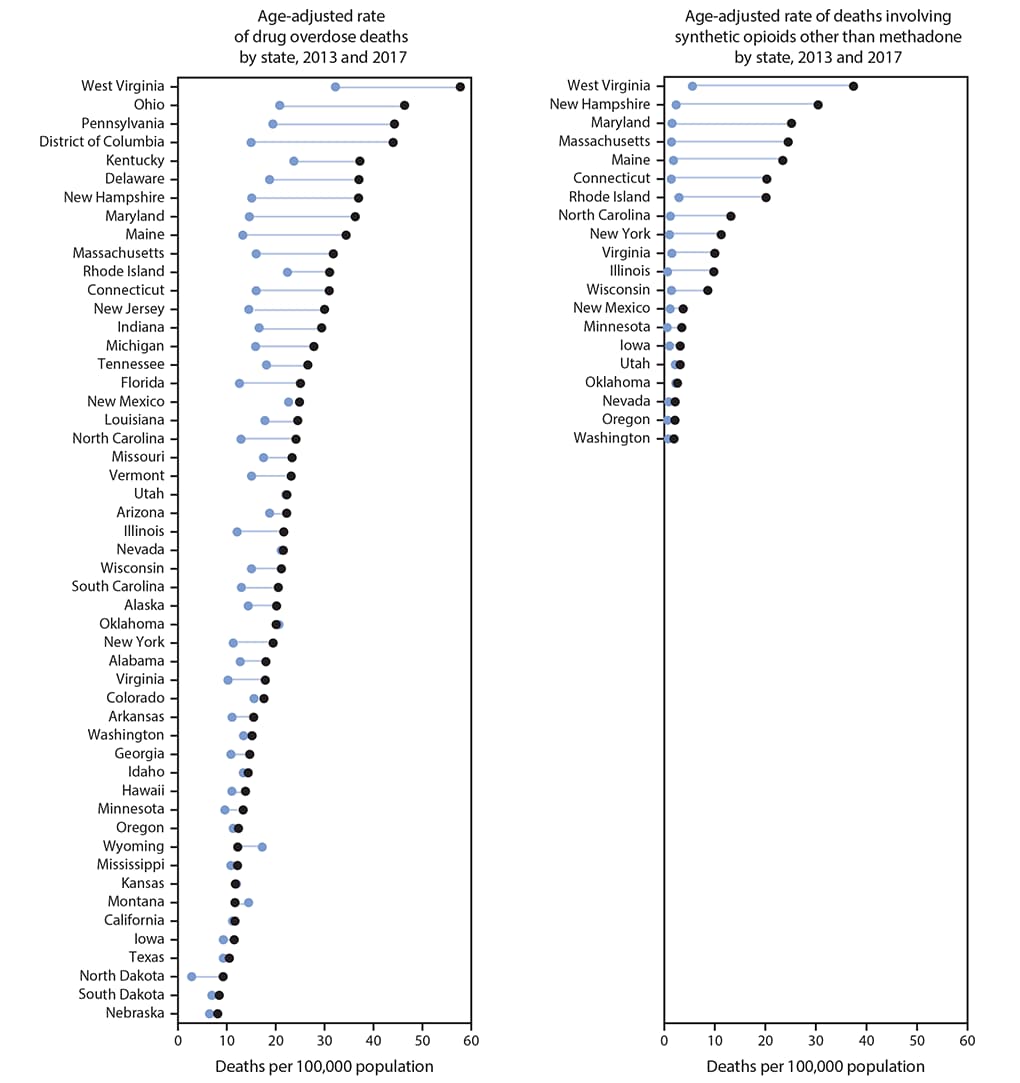
* Rates shown are the number of deaths per 100,000 population. Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 U.S. standard population age distribution.
† Deaths are classified using the International Classification of Diseases, Tenth Revision (ICD–10). Left panel includes drug overdose deaths identified using underlying cause-of-death codes X40–X44, X60–X64, X85, and Y10–Y14. Right panel includes drug overdose deaths, as defined, that have synthetic opioids other than methadone (T40.4) as a contributing cause.
§ State-level analyses of overdose rates for deaths involving synthetic opioids other than methadone included 20 states that met the following criteria: 1) >80% of drug overdose death certificates named at least one specific drug in 2013–2017; 2) change from 2013 to 2017 in the percentage of death certificates reporting at least one specific drug was <10 percentage points; and 3) ≥20 deaths involving synthetic opioids other than methadone occurred each year during 2013–2017. States whose reporting of any specific drug or drugs involved in an overdose changed by ≥10 percentage points from 2013 to 2017 were excluded because drug-specific overdose numbers and rates might have changed substantially from 2013 to 2017 as a result of changes in reporting.
¶ Left panel: Joinpoint regression examining changes in trends from 2013 to 2017 indicated that 35 states and the District of Columbia had significant increases in drug overdose death rates from 2013 to 2017 (Alabama, Alaska, Arizona, Arkansas, Connecticut, Delaware, District of Columbia, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, New Jersey, New York, North Carolina, Ohio, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Vermont, Virginia, Washington, West Virginia, and Wisconsin). All remaining states had nonsignificant trends during this period. Right panel: Joinpoint regression examining changes in trends from 2013 to 2017 indicated that 15 states had significant increases in death rates for overdoses involving synthetic opioids other than methadone from 2013 to 2017 (Connecticut, Illinois, Iowa, Maine, Maryland, Minnesota, Nevada, New York, North Carolina, Oregon, Rhode Island, Virginia, Washington, West Virginia, and Wisconsin). The five remaining states analyzed had nonsignificant trends during this period. Significant increases in trends were not detected in some states with large absolute increases in death rates from 2013 to 2017 because of limited power to detect significant effects.
Suggested citation for this article: Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2019;67:1419–1427. DOI: http://dx.doi.org/10.15585/mmwr.mm675152e1.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.