At a glance
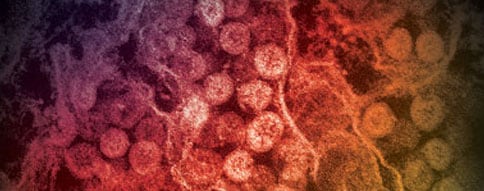
- Middle East Respiratory Syndrome (MERS) is caused by Middle East Respiratory Syndrome Coronavirus (MERS-CoV). A wide clinical spectrum of illness in patients with MERS has been reported. People with MERS-CoV infection range from being asymptomatic to having severe acute respiratory illness resulting in death, with most reported cases having more severe illness.
Clinical presentation
Middle East Respiratory Syndrome (MERS) is caused by Middle East respiratory syndrome coronavirus (MERS-CoV). A wide clinical spectrum of illness in patients with MERS has been reported. People with MERS-CoV infection range from being asymptomatic to having severe acute respiratory illness resulting in death, with most reported cases having more severe illness.
Although MERS cases have been reported among children and adults of all ages, most reported MERS cases have been in older adults. Most hospitalized MERS patients have had pre-existing medical conditions that likely increased their risk for severe illness. Among global cases reported to date, the mortality rate of MERS cases reported to the World Health Organization (WHO) is approximately 35%.
Common signs and symptoms of MERS include:
- fever
- dyspnea
- non-productive cough
- chills/rigors
- headache
- myalgia
Other signs and symptoms can include sore throat, coryza (runny nose and/or sneezing), productive cough, dizziness, nausea and vomiting, diarrhea, and abdominal pain.
Chest radiographic findings might include unilateral or bilateral patchy densities or opacities, interstitial infiltrates, consolidation, or pleural effusions.
Patients who require admission to an intensive care unit (ICU) often have a history of a febrile upper respiratory tract illness, and they might exhibit rapid progression to pneumonia (i.e., within a week of illness onset). Rapidly progressive pneumonitis, acute respiratory distress syndrome (ARDS), refractory hypoxemia, respiratory failure, and extrapulmonary complications, including acute kidney injury, hypotension, hepatitis, and septic shock, have been reported.
Contact the CDC Emergency Operations Center
Clinical course
Most patients develop symptoms approximately 5 days after an exposure to an infected person or camel, but the incubation period can range from 2-14 days.
In hospitalized MERS patients, the median time from the onset of symptoms to a person's hospitalization is approximately 4 days.
In critically ill patients, the median time from onset to ICU admission is approximately 5 days, and median time from onset to death is approximately 12 days.
Laboratory Findings
Laboratory findings at admission can vary, but can include leukopenia, lymphopenia, thrombocytopenia, and elevated lactate dehydrogenase levels. Co-infection with other respiratory viruses and with community-acquired bacteria at hospital admission have been reported. MERS-CoV can be detected with higher viral load and for a longer duration in the lower respiratory tract compared with the upper respiratory tract.
Duration of MERS-CoV shedding in the respiratory tract is typically longer in more severely ill patients than mildly ill patients. It has been reported that evidence of MERS-CoV RNA has been detected in survivors for a month or more after onset, and culturable virus has been detected up to 25 days after onset. Limited data are available on the duration of extrapulmonary MERS-CoV shedding.
Patient management
There is currently no specific treatment for MERS-CoV infection. Clinical management includes supportive management of signs, symptoms, and complications. Implementation of recommended infection prevention and control measures is very important.
