Key points
- Common fungal diseases are ringworm, nail infections, and vaginal yeast infections.
- Some fungi in the environment cause pneumonias.
- Hospitalized patients can get severe, often deadly, fungal diseases like Candida auris infections and candidemia.
- Fungal diseases are often misdiagnosed which can delay appropriate antifungal treatment.
- Increasing antimicrobial resistance limits treatment options.
Overview
There are nearly 1-5 million species of fungi but only a few hundred can make people sick. Fungal infections range from mild to life-threatening. People with weakened immune systems (from illness, age, or medical treatments like steroids) are at higher risk for most fungal infections.
Worldwide, more than one billion people get a fungal infection each year. Learn 5 facts about fungal diseases.
Use this PDF to learn more about fungal diseases
See more about the spread of fungal diseases and future directions.
Types
Common infections
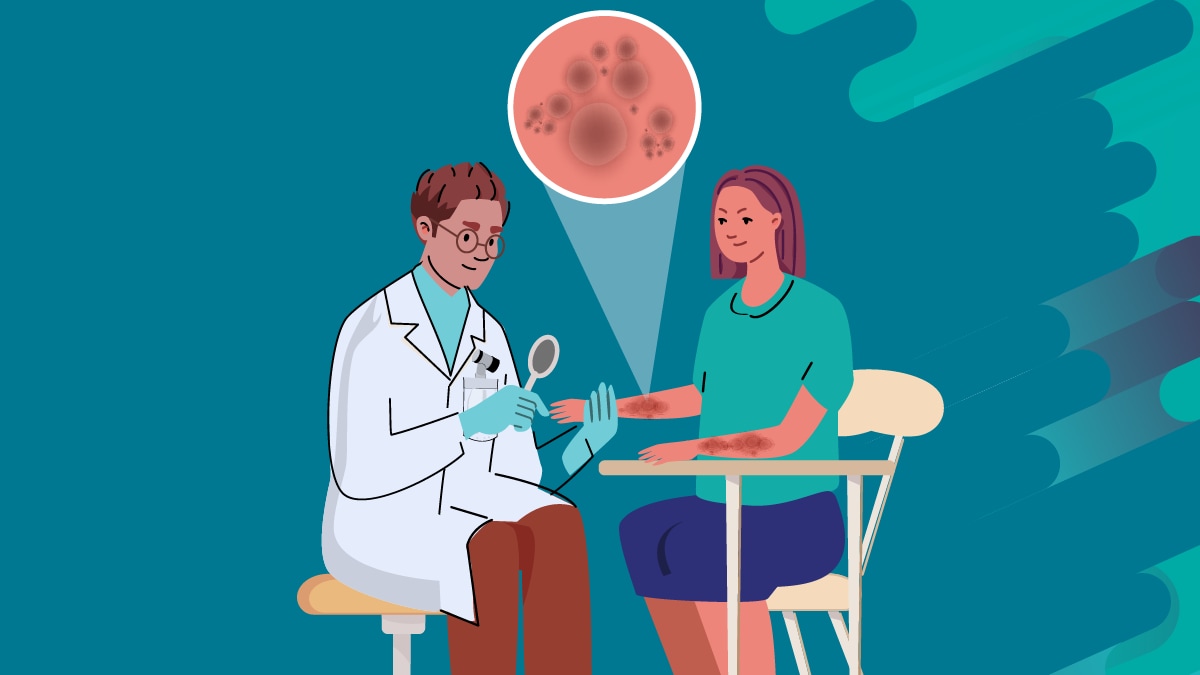
Two common fungal infections are ringworm and vaginal yeast infections.
Ringworm typically causes a ring-like rash and spreads easily between people and from pets to people. The same fungi that cause ringworm can cause jock itch, athlete's foot, and nail infections.
Most women get a vaginal yeast infection at least once in their lives. Vaginal yeast infections are caused by overgrowth of a yeast called Candida in the vagina. Everyone has Candida in and on their body; it only causes symptoms when it grows out of control.
Environmental (community-acquired) pneumonias
Other types of fungal infections spread in the environment and can cause pneumonia. Three of these infections, blastomycosis, histoplasmosis, and coccidioidomycosis (Valley fever) spread in different parts of the United States.
Infections are caused by breathing in fungal spores from soil or dust. Many people breathe in the spores without ever getting sick but some people develop severe illness.
Emerging zoonosis
Another type of fungi called Sporothrix causes sporotrichosis, which is typically a skin infection. People can get infected through scrapes from shrubs or plant matter with Sporothrix.
In Brazil and parts of Latin America Sporothrix brasiliensis, a subtype of Sporothrix, is spreading. S. brasiliensis is an emerging concern because it spreads between cats and people and can cause more severe infections. This type of sporotrichosis is not currently spreading in the United States.
Mold infections
Molds are a type of fungus that can live in indoor or outdoor environments. Two of the most common mold infections are mucormycosis and aspergillosis.
These molds are everywhere and typically do not cause illness. However, people with weakened immune systems can get infected. There are different types of mucormycosis and aspergillosis, but lung infections are the most common.
Healthcare-associated infections
Serious fungal infections can occur in healthcare settings like hospitals and long-term care facilities. Many patients already have weakened immune systems due to illness or injury, recent surgery, or medications like corticosteroids.
Patients may have invasive medical devices (like catheters and ventilators) or undergo surgeries. Both create opportunities for disease-causing fungi to get into the bloodstream, organs, or tissues.
Molds like mucormycoses and aspergillus can cause outbreaks in healthcare facilities. Healthcare-associated fungal diseases like candidemia, Candida auris infections, are among the most severe.
HIV/AIDS-associated infections
Some fungal infections are much more common among people living with HIV/AIDS (particularly those with CD4 counts below 200).
Two well-known fungal infections associated with HIV/AIDS in the United States are oral candidiasis (thrush) and Pneumocystis pneumonia. Worldwide, cryptococcal meningitis and histoplasmosis are major causes of illness in people living with HIV.

Testing
Many fungal infections can appear similar to more common diseases caused by bacteria or viruses. Misdiagnoses or delayed diagnoses and treatment are common and can cause high costs, severe illness, and death. It is important to talk to your healthcare provider if you think you or a loved one has a fungal infection.

Treatment and recovery
Fungal diseases are treated with antifungal medicines which can be oral, intravenous, or in the form of creams or ointments. There are only a few types of antifungal medicines. Antibiotics cannot treat fungal infections and can even increase the risk of fungal infections.
Antimicrobial resistance
Increasingly, fungi are becoming resistant to one or more antifungals. Antifungal resistance is when fungi develop the ability to defeat the antifungal designed to kill them. To help keep medications working, only take them exactly as prescribed by your healthcare provider.







