Key points
- FoodCORE improves enteric disease investigation and response in state and local health departments
- FoodCORE centers collaborate across laboratory, epidemiology, and environmental health
- Performance metrics demonstrate the impact of FoodCORE resources
- Experiences of FoodCORE centers are shared through success stories and model practices
What is FoodCORE
FoodCORE stands for Foodborne Diseases Centers for Outbreak Response Enhancement. It is a CDC program to enhance the ability of state and local health departments to respond to enteric disease outbreaks.
FoodCORE centers work together to develop improve methods to detect, investigate, respond to, and control multistate outbreaks of foodborne diseases. Efforts are primarily focused on outbreaks caused by bacteria, including Salmonella, Shiga toxin-producing E. coli, and Listeria. The ability to detect and investigate viral and parasitic foodborne disease outbreaks will also be strengthened.
Why it's important
Each year in the United States foodborne diseases cause: 1
- 1 in 6 Americans (or about 48 million people) to become ill1
- 128,000 hospitalizations1
- 3,000 deaths1
Fast and effective outbreak investigations are needed to identify and remove contaminated food from the market to prevent additional illnesses. Identifying contaminated foods and learning how the contamination happened also help public health officials prevent similar outbreaks in the future. However, most health departments lack the resources to conduct comprehensive enteric disease surveillance and rapid, coordinated outbreak detection and response.
Did you know?
Program priorities
FoodCORE aims to improve enteric disease surveillance and outbreak response by providing targeted funding to strengthen capacity and collaboration. Program priorities include:
- Funding laboratory, epidemiology, and environmental health staff
- Developing collaborative surveillance and response programs
- Conducting fast, coordinated, and standardized investigations
- Developing and implementing performance metrics
- Identifying and documenting replicable model practices.
FoodCORE centers work to increase collaboration across laboratory, epidemiology, and environmental health within their health department. Staff from each area play a critical role in ongoing enteric surveillance and outbreak response. This includes:
- Learning a sick person's food, water, and environmenal exposures
- Determining what bacteria, virus, or parasite made them sick
- Assessing the environment where contamination may have occurred
With increased coordination between these three areas, the centers are able to:
- Detect more outbreaks
- Conduct thorough investigations
- Control outbreaks faster
- Protect other people from getting sick
Outcomes
Performance metrics were developed and tested by FoodCORE centers to measure the burden, timeliness, and completeness of foodborne disease activities. Metrics span from outbreak surveillance and detection through investigation, response, control, and prevention measures.
FoodCORE centers report data for Salmonella, Shiga toxin-producing Escherichia coli (STEC), and Listeria (SSL); and norovirus, other enteric disease pathogens, and outbreaks of unknown etiology (NOU).
Metrics data are shared online to show the impact of the changes that FoodCORE centers have implemented in their health departments.
What's ahead
FoodCORE centers are at the forefront of enteric disease surveillance and outbreak response. They will continue to innovate and share their experiences with others. Their successes and lessons learned will be shared online and at conferences and meetings.
Documenting success
FoodCORE centers are test kitchens for new ideas to investigate and respond to outbreaks of enteric illness. When they find something that works, a success story or model practice is written and published to the FoodCORE website. Other health departments can learn and implement these successful practices in their jurisdictions.
Success Stories
Success stories highlight outbreak investigations or projects that were particularly successful in a FoodCORE center. Topics of success stories include:
- Contributions to solving large or multi-state outbreaks
- Adaptation to changing laboratory methods
- Collaboration within a FoodCORE center and across centers
- Novel strategies to detect more cases or interview more thoroughly
Model Practices
Model practices describe what's been successful in FoodCORE centers. When a practice works across centers with varying sizes, structure, and burden, it's likely to work in other jurisdictions too. These practices are documented so that others can learn from FoodCORE centers and replicate what's worked. Topics of published model practices include laboratory timeliness and completeness, initial case-patient interviewing, student interview teams, and team communication and collaboration. Model practices are periodically revised to ensure they remain accurate as methods and technologies evolve and advance.
How it's funded
FoodCORE centers were selected through a competitive application process via CDC’s Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement.
Funding recipients
Started in 2009, the program has grown to include 10 state and local health departments. The centers cover 18% of the U.S. population, or 58 million people. The current FoodCORE centers are:
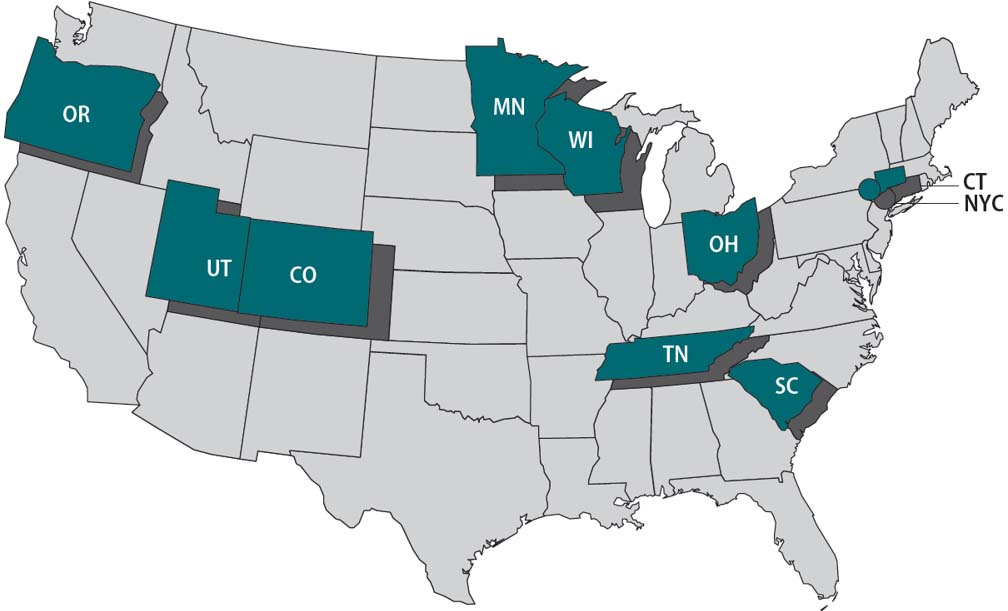
- Colorado
- Connecticut
- Minnesota
- New York City
- Ohio
- Oregon
- South Carolina
- Tennessee
- Utah
- Wisconsin
FoodCORE centers collaborate with other federal food safety programs. All ten FoodCORE centers participate in PulseNet, five are FoodNet sites, and three are Food Safety CoEs. Cross-program collaborations enhance and complement FoodCORE's internal capacity building.
- Scallan, E., Griffin, P. M., Angulo, F. J., Tauxe, R., & Hoekstra, R. M. (2011). Foodborne Illness Acquired in the United States—Unspecified Agents. Emerging Infectious Diseases, 17(1), 16-22. https://doi.org/10.3201/eid1701.p21101.
