Where Resistance Spreads: Healthcare Facilities

People receiving medical care in healthcare facilities like hospitals or nursing homes can get serious infections called healthcare-associated infections (HAIs). People can get HAIs during or after procedures like surgery, or from devices like catheters or ventilators. Sometimes these infections can be caused by antimicrobial-resistant germs. People can also enter healthcare facilities with infections from the community or from another healthcare facility when transferred and these germs could spread without appropriate infection control measures.
Some of the deadliest resistant germs spread within and across healthcare facilities. In fact, seven urgent or serious antimicrobial-resistant threats identified in CDC’s 2019 AR Threats Report can cause HAIs. The estimated national cost to treat infections caused by these six multidrug-resistant germs can be substantial—more than $4.6 billion annually.
Yet many HAIs are preventable. From 2012 to 2017, the number of antimicrobial-resistant infections seen in hospitals dropped 27% and the number of deaths from antimicrobial-resistant infections fell nearly 30%. Although progress has been made, more work is needed. Three critical efforts to prevent an HAI and slow the spread of resistance include:
- Prevent infections related to surgery or placement of a catheter
- Prevent the spread of germs through infection prevention and control
- Improve use of antibiotics and antifungals (these drugs save lives but their use can contribute to the development of resistant germs)
Learn more about HAIs and what you can do to be a safe patient.
Download a printable fact sheet highlighting information on this webpage: Everything is Connected: Healthcare Facilities [PDF – 1 page].
How Germs Can Spread in Healthcare Facilities
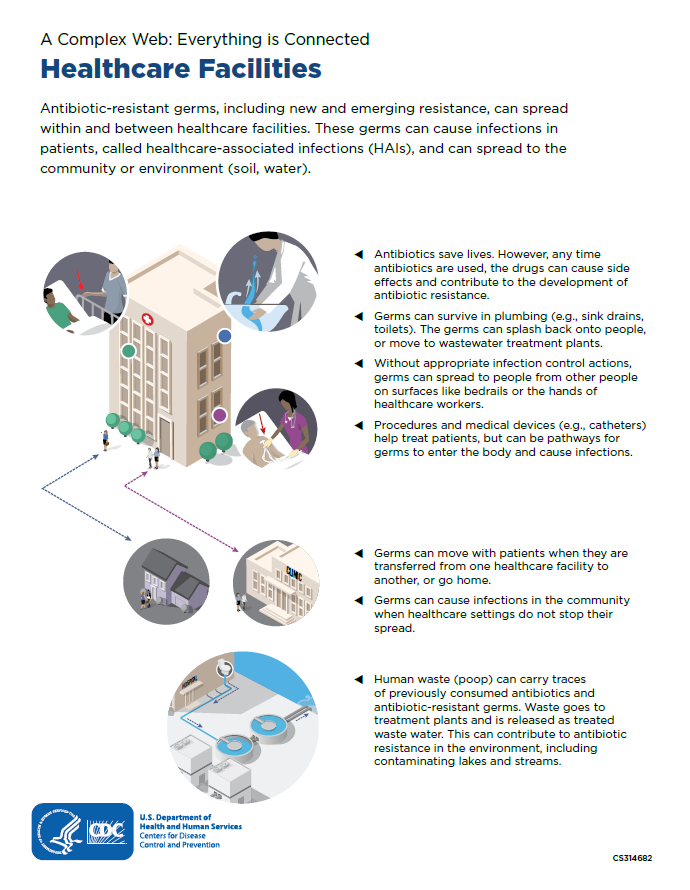
Healthcare staff use infection control practices like hand hygiene or wearing protective equipment to prevent spreading germs. Without appropriate infection control actions, germs can:
- Enter the body and cause infections through procedures and medical devices (e.g., catheters)
- Spread to people on surfaces like bedrails or the hands of healthcare workers
- Move with patients when they are transferred from one healthcare facility to another, or into the community when patients go home
- When not stopped, these resistant healthcare-associated germs can spill over into communities, becoming much harder to control
Germs can also spread in other ways. Fecal waste (poop) can carry traces of previously consumed antibiotics, antifungals, and antimicrobial-resistant germs. The combination of these drugs and resistant germs in hospital wastewater allows these resistant germs to survive in plumbing systems (e.g., toilets).
Additionally, when waste goes to treatment plants, there is the possibility of sewage leaks and overflow along the way, and sometimes drug residues and resistant germs are released as part of the treated wastewater. This can contribute to antimicrobial resistance in the environment, including contaminating lakes and streams. CDC and partners are doing more research to better understand the spread of resistance through water.
COVID-19 Impacts Antimicrobial Resistance
Much of the U.S. progress in combating antimicrobial resistance was lost in 2020, in large part, due to the effects of the COVID-19 pandemic. The pandemic pushed healthcare facilities, health departments, and communities near their breaking points.
Find out more about the impact of COVID-19 on antimicrobial resistance in the U.S.
About Antibiotic/Antifungal Use in Healthcare
Antibiotics and antifungals are valuable tools. Patients should always be promptly treated when the drugs are needed for infections and to prevent sepsis. Effective antibiotics and antifungals are also needed for people who are at high risk for developing infections, such as patients who have surgery and are at risk for surgical site infections.
However, any antibiotic and antifungals use—for people, animals, or plants—can cause side effects and contribute to antimicrobial resistance. One life-threatening side effect of taking antibiotics is severe diarrhea and colitis (inflammation of the colon) caused by Clostridioides difficile (also called C. diff). In 2017, CDC estimated 223,900 cases of C. diff infections requiring hospitalizations or in already hospitalized patients. At least 12,800 people died. C. diff can spread rapidly within healthcare facilities.
Improving antibiotic and antifungal prescribing and use is critical to treat infections effectively, protect patients from harms, and combat antimicrobial resistance. Learn more about antibiotic stewardship in healthcare facilities.