Drug Overdose Deaths in 28 States and the District of Columbia: 2020 Data from the State Unintentional Drug Overdose Reporting System
SUDORS Data Brief, Number 1, June 2022
Printable PDF Version [PDF – 891 KB]
Christine L. Mattson, PhD, Sagar Kumar, MPH, Lauren J. Tanz, ScD, Priyam Patel, MSPH, Qingwei Luo, MS, and Nicole Davis, PhD
- In 2020, 38,048 drug overdose deaths were reported from 28 states and DC for an age-adjusted rate of 30.6 per 100,000 people
- 70% of drug overdose deaths involved illicitly manufactured fentanyls (IMFs)
- The rate of drug overdose deaths was highest among American Indian/Alaska Native, non-Hispanic and Black, non-Hispanic persons
- Two-thirds of decedents had at least one potential opportunity for linkage to care or implementation of a life-saving action prior to death
Introduction
In the United States, 91,799 drug overdose deaths occurred in 2020, a 30% increase from 2019, and provisional estimates suggest continued increases in 2021.1,2 Recent increases in drug overdose deaths have been largely driven by illicitly manufactured fentanyl (IMF),3,4,5 but deaths involving stimulants, such as cocaine and methamphetamine, are also on the rise.3,4,6 This report uses data from the State Unintentional Drug Overdose Reporting System (SUDORS), which complements information available from other systems, to describe the drugs involved in and circumstances surrounding drug overdose deaths of unintentional or undetermined intent to help inform overdose prevention and response efforts.
Data Source and Methods
CDC funds 47 states and the District of Columbia to abstract information from death certificates and medical examiner and coroner reports, including toxicology results, on drug overdose deaths of unintentional or undetermined intent through SUDORS. Detailed information is abstracted and entered into a web-based system to describe decedent demographics, circumstances that preceded the fatal overdose (e.g., prior history of overdose, recent release from an institutional setting), circumstances occurring during or immediately preceding the overdose (e.g., presence of potential bystanders), as well as some limited medical history (e.g., mental health diagnoses, treatment for substance use disorder), and response to the overdose (e.g., naloxone administration). In addition, SUDORS contains information on drugs detected during post-mortem toxicology testing as well as those determined by a medical examiner or coroner to have caused death.
This report includes data from 28 states and the District of Columbia that collected information on all drug overdose deaths of unintentional and undetermined intent that occurred during January to December 2020 and had medical examiner/coroner reports for at least 75% of deaths (see map).
- Recent release from institutional setting
- Prior overdose
- Mental health diagnosis
- Current treatment for substance use disorder(s)
- Potential bystander present at fatal overdose
- Fatal drug use witnessed
Death counts and rates were presented overall and grouped by opioid and stimulant involvement into three mutually exclusive categories: 1) opioids with stimulants, 2) opioids without stimulants, and 3) stimulants without opioids. In addition, overdose deaths were grouped into the 10 most frequently occurring mutually exclusive combinations of specific opioid and stimulant types.
Rates were calculated from 2020 Census population denominators. Drug-, sex-, and race/ethnicity-specific rates are age standardized to the 2010 Census population.
Select circumstances surrounding the overdose were analyzed to characterize the overdose setting (i.e., location of the overdose, whether the person was experiencing homelessness or housing instability), response to the overdose (i.e., naloxone administration), and to identify possible intervention opportunities. A composite variable was created to identify documented evidence that a decedent had one or more potential intervention opportunities (see box).
Results
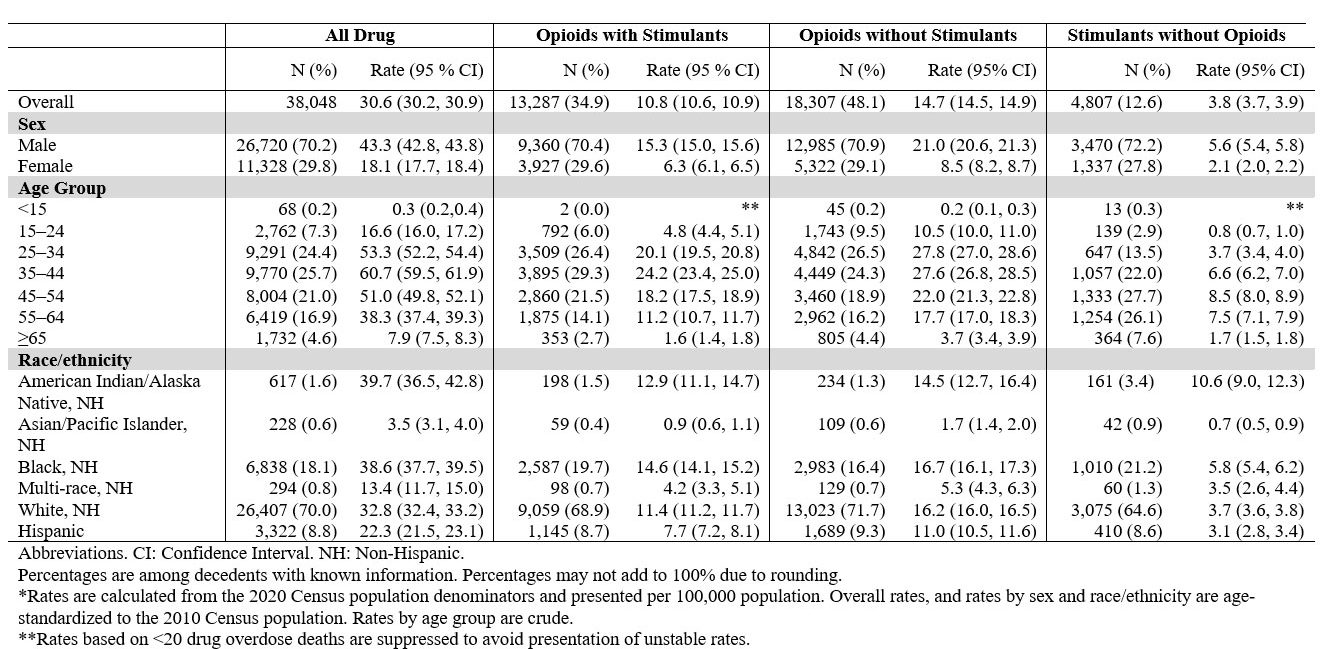
In 2020, 38,048 drug overdose deaths occurred in 28 states and DC for an age-adjusted rate of 30.6 per 100,000 population (appendix).
- 13,287 deaths involved opioids with stimulants, accounting for 34.9% of all overdose deaths, for an age-adjusted rate of 10.8 per 100,000
- 18,307 deaths involved opioids without stimulants, accounting for 48.1% of all overdose deaths, for an age-adjusted rate of 14.7 per 100,000
- 4,807 deaths involved stimulants without opioids, accounting for 12.6% of all overdose deaths, for an age-adjusted rate of 3.8 per 100,000
In 2020, drug overdose death rates varied by sex, age, and race and ethnicity.
- The age-adjusted rate of drug overdose deaths was 43.3 per 100,000 for males and 18.1 per 100,000 for females
- The rate of drug overdose deaths was highest among persons aged 35–44 years of age at 60.7 per 100,000
- The age-adjusted rate of drug overdose deaths was highest for American Indian/Alaska Native, non-Hispanic persons at 39.7 per 100,000 and for Black, non-Hispanic persons at 38.6 per 100,000
In 2020, overdose death rates involving opioids with and without stimulants and stimulants without opioids varied by age.
- For deaths that involved opioids with stimulants, the death rate was highest among persons aged 35–44 at 24.2 per 100,000
- For deaths that involved opioids without stimulants, the death rate was highest among persons aged 25–34 at 27.8 per 100,000 and among persons 35-44 at 27.6 per 100,000
- For deaths that involved stimulants without opioids, the death rate was highest among persons aged 45–54 at 8.5 per 100,000
In 2020, overdose death rates involving opioids with and without stimulants and stimulants without opioids varied by race and ethnicity.
- For deaths involving opioids with stimulants, the age-adjusted rate was highest among Black, non-Hispanic persons at 14.6 per 100,000 persons followed by American Indian/Alaska Native, non-Hispanic persons at 12.9 per 100,000
- For deaths involving opioids without stimulants, the age-adjusted rate was highest among Black, non-Hispanic persons at 16.7 per 100,000 followed by deaths among White, non-Hispanic persons at 16.2 per 100,000 persons
- For deaths involving stimulants without opioids, the age-adjusted rate was highest among American Indian/Alaska Native, non-Hispanic persons at 10.6 per 100,000 persons
In 2020, the five most frequently occurring opioid and stimulant combinationsc accounted for 59.6% of overdose deaths:
- 27.9% involved IMFs with no other opioids or stimulants
- 12.8% involved IMFs and Cocaine
- 7.2% involved IMFs and Methamphetamine
- 5.8% involved Prescription Opioids with no other opioids or stimulants
- 5.8% involved IMFs and Heroin
In 2020, 70.0% of all drug overdose deaths involved illicitly manufactured fentanyls.
In 2020, persons who died of a drug overdose had documented evidence of the following select circumstancesd:
- 62.8% of decedents overdosed at home
- 20.6% were administered naloxone during or after the fatal overdose
- 7.4% were experiencing homelessness or housing instability at the time of death
In 2020, most circumstancesd were similar across drug categories; however, some differences were noted for deaths involving stimulants without opioids
- At least one potential intervention opportunitye was documented in 60.7% of overdose deaths involving stimulants without opioids compared to 65.9% for all drug overdose deaths
- A prior overdose was documented in 4.2% of overdose deaths involving stimulants without opioids compared to 11.5% for all drug overdose deaths
- Current treatment for substance use disorder(s) was documented in 2.4% for overdose deaths involving stimulants without opioids, compared to 5.9% for all drug overdose deaths
- Highly potent IMFs were involved in 70.0% of drug overdose deaths
- 27.9% of all drug overdose deaths involved IMFs with no other opioids or stimulants
- IMFs were also frequently co-involved with other drugs
- 12.8% of all drug overdose deaths involved IMFs and Cocaine
- 7.2% of all drug overdose deaths involved IMFs and Methamphetamine
- 5.8% of all drug overdose deaths involved IMFs and Heroin
Recommended actions:
- Ensure treatment for substance use disorder(s) addresses polysubstance use
- Encourage people who use drugs not to use alone
- Encourage friends and families of people who use drugs to recognize the signs and symptoms of overdose and ensure they know how to use naloxone
- Expand naloxone distribution to people who use drugs, families, friends, and communities regardless of known opioid use because naloxone can be administered without concern for adverse reaction if opioids were not involved
- Expand fentanyl test strip distribution and training on use and correct interpretation
- The overall rate of drug overdose deaths was highest among American Indian/Alaska Native, non-Hispanic and Black, non-Hispanic persons
Recommended actions:
- Ensure substance use prevention and treatment interventions, including expanded linkage and retention in care, equitable access to treatment and behavioral interventions and harm reduction services (e.g., naloxone, comprehensive syringe services programs, and fentanyl test strips), are designed and implemented to reach American Indian/Alaska Native and Black persons
- Integrate evidence-based substance use treatment with culturally appropriate traditional practices, such as spirituality and religion, which could improve treatment uptake.
- Drug overdose deaths involving opioids with stimulants accounted for one third of all drug overdose deaths, and rates differed by race/ethnicity
- Deaths rates involving opioids with stimulants were highest among American Indian/Alaska Native, non-Hispanic, Black, non-Hispanic, and White, non-Hispanic persons
Recommended action:
- Ensure increased access to medications for opioid use disorder, harm reduction services, cognitive behavioral therapy and evidence-based treatments for stimulant use disorders (e.g., contingency management) for all persons, including addressing access barriers (e.g., housing instability, transportation access, insurance status) for American Indian/Alaska Native and Black persons
- Two-thirds of drug overdose decedents had at least one potential opportunity for linkage to care prior to death or implementation of a life-saving action prior to deathe
Recommended actions:- Initiate, link to, or continue evidence-based treatment services for substance use disorder(s), including medications for opioid use disorder, when people who use drugs interact with the health care and criminal justice systems
- Integrate treatment for substance use disorder(s) and mental health when appropriate
- Increase naloxone distribution and training for people who use drugs and their families and friends
Definitions and Technical Notes
SUDORS: CDC’s State Unintentional Drug Overdose Reporting System (SUDORS) collects information on drug overdose deaths of unintentional or undetermined intent. In 2016, SUDORS was launched as part of the Enhanced State Opioid Overdose Surveillance (ESOOS) program, which funded 12 states and in 2017, an additional 20 states and the District of Columbia (DC) were funded to abstract data on opioid-involved overdose deaths. In 2019, as part of CDC’s Overdose Data to Action (OD2A) program, SUDORS was expanded to collect data on all drug overdose deaths from 47 states and DC (collectively referred to as jurisdictions).
Bystander: a potential bystander is defined as a person aged ≥11 years who was physically nearby either during or shortly preceding a drug overdose and potentially had an opportunity to intervene or respond to the overdose. This includes any persons in the same structure (e.g., same room or same building, but different room) as the decedent during that time. For example, the family member of an opioid overdose decedent who was in another room during the fatal incident would be considered a potential bystander if that person might have had an opportunity to provide life-saving measures such as naloxone administration, if adequate resources were available and the family member was aware that an overdose event could occur. This does not include, however, persons in different self-contained parts of larger buildings (e.g., a person in a different apartment in the same apartment building would not be considered a potential bystander).
Current treatment: current treatment for substance use disorders (SUD) included medications for opioid use disorder (MOUD), living in an inpatient rehabilitation facility, or participation in mental health or SUD outpatient treatment.
Involved: drugs were classified as involved in (i.e., contributing to) overdose deaths if the medical examiner/coroner listed them as causing death on the death certificate, or in the medical examiner/coroner report, or postmortem toxicology report.
Fentanyl: fentanyl is a synthetic opioid that is 80-100 times stronger than morphine.
Fentanyl analog: a chemical compound that has similar chemical or pharmacologic properties as, but minor structural changes, to fentanyl.
Homelessness/housing instability: persons experiencing homelessness were those who resided in either places not designed for or ordinarily used as regular sleeping accommodations or in a supervised shelter or drop-in center designated to provide temporary living arrangements, congregate shelters, or temporary accommodations provided by a homeless shelter. Persons experiencing housing instability are those who are not experiencing homelessness but lack the resources or support networks to obtain or retain permanent housing and includes interrelated challenges, such as trouble paying rent, overcrowding, moving frequently, or staying with relatives.
Heroin: drugs coded as heroin were heroin and 6-acetylmorphine. In addition, morphine was coded as heroin if detected along with 6-acetylmorphine or if scene, toxicology, or witness evidence indicated presence of heroin impurities or other illicit drugs, injection, illicit drug use, or a history of heroin use.
Illicitly manufactured fentanyls (IMFs): fentanyl was classified as likely illicitly manufactured using toxicology, scene, and witness evidence. In the absence of sufficient evidence to classify fentanyl as illicit or prescription, fentanyl was classified as illicit because the vast majority of fentanyl overdose deaths involve illicit fentanyl. All fentanyl analogs except alfentanil, remifentanil, and sufentanil (which have legitimate human medical use) were included as illicitly manufactured fentanyls.
Naloxone: naloxone is a life-saving medication that can reverse an overdose from opioids, including heroin, fentanyl, and prescription opioid medications.
Opioids: for the purpose of this analysis, the opioid category includes both prescription and illicit opioids such as hydrocodone, oxycodone, oxymorphone, morphine, codeine, fentanyl, heroin, and fentanyl analogs.
Recent release from institutional setting: released within a month before death from institutional settings such as prisons/jails, residential treatment facilities, and psychiatric hospitals.
Stimulants: for the purpose of this analysis, the stimulant category includes cocaine and all its metabolites, amphetamines and cathinones, and the following central nervous system stimulants: 2-fluoromethamphetamine, 3,4-dichloromethylphenidate, 4-Fluoromethamphetamine, armodafinil, atomoxetine, beta-Phenethylamine, caffeine, CNS stimulant not otherwise specified, dexmethylphenidate, ephedrine, isopropylphenidate, lisdexamfetamine, mephentermine, methylphenidate, modafinil, propylhexedrine, pseudoephedrine, norephedrine, norpseudophedrine, ritalinic acid, stimulant amines, sympathetic amine, and sympathomimetics.
About the Authors
Christine Mattson, Sagar Kumar, Lauren Tanz, and Nicole Davis work on the Overdose Mortality Team in the Epidemiology and Surveillance Branch in the Division of Overdose Prevention (DOP) at the National Center for Injury Prevention and Control. Priyam Patel is a fellow at the Oak Ridge Institute for Science and Education assigned to DOP. Qingwei “Cherry” Luo works for Strategic Innovation Solutions, LLC (SIS) and is assigned to provide data management and statistical support to DOP.
Suggested Citation
Mattson CL, Kumar S, Tanz LJ, Patel P, Luo Q, Davis NL. Drug Overdose Deaths in 28 States and the District of Columbia: 2020 data from the State Unintentional Drug Overdose Reporting System (SUDORS). SUDORS Data Brief, No 1. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2022.
Acknowledgements
Jurisdictions participating in the State Unintentional Drug Overdose Reporting System and participating state or jurisdictional agencies, including health departments, vital registrar offices, and coroners and medical examiners offices.
Additional information on CDC’s overdose surveillance, prevention and response initiative can be found at Overdose Data to Action. For more information on SUDORS, please see State Unintentional Drug Overdose Reporting System (SUDORS) Fact Sheet (cdc.gov) For more information on drug overdose death data in the United States, please see https://www.cdc.gov/drugoverdose/deaths/index.html and https://www.cdc.gov/drugoverdose/fatal/dashboard/index.html.
- Jurisdictions that reported all overdose deaths in their jurisdiction during 2020 and had medical examiner/coroner reports for at least 75% of deaths are included in this dashboard. These jurisdictions include Alaska, Arizona, Connecticut, Delaware, District of Columbia, Georgia, Kansas, Kentucky, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Montana, Nevada, New Hampshire, New Jersey, New Mexico, North Carolina, Ohio, Oklahoma, Oregon, Rhode Island, South Dakota, Utah, Vermont, Virginia, and West Virginia.
- The following race and ethnicity groups were analyzed: American Indian/Alaska Native, non-Hispanic (AI/AN, NH), Asian/Pacific Islander, non-Hispanic (A/PI, NH), Black, non-Hispanic (Black, NH), Multi-race, non-Hispanic (Multi, NH), White, non-Hispanic (White, NH) and Hispanic.
- Opioid and stimulant drugs or drug combinations included illicitly manufactured fentanyls (including fentanyl and fentanyl analogs), heroin, prescription opioids (including alfentanil, buprenorphine, butorphanol, codeine, dextrorphan, dihydrocodeine, hydrocodone, hydromorphone, levorphanol, loperamide, meperidine, methadone, morphine (if scene or witness evidence did not indicate likely heroin use and if 6-acetylmophine was not also detected), nalbuphine, noscapine, oxycodone, oxymorphone, pentazocine, prescription fentanyl, propoxyphene, sufentanil, tapentadol, tramadol, and prescription brand names (e.g., Opana) and metabolites (e.g., nortramadol)), other opioids (including non-specific opioids or other synthetic opioids such as U-4770, isotonitazene), cocaine, methamphetamine, and other stimulants (including amphetamine, cathinones, and central nervous system stimulants). If a category does not specify whether other opioids or other stimulants are or are not involved, then the category includes deaths involving the specified drugs (e.g., heroin, methamphetamine) with and without other opioids or other stimulants.
- Circumstances represent evidence available in source documents; these are likely underestimated as death investigators might have limited information. Circumstance percentages are only calculated among decedents with an available medical examiner or coroner report, which included 97.6% of decedents in this analysis (928 or 2.4% were missing reports).
- Potential opportunities for intervention included documented evidence of at least one of the following: potential bystander presence, a mental health diagnosis, prior overdose, fatal drug use witnessed, recent release from institutional setting (< 1 month), or current treatment for substance use disorder(s). Percentages are only calculated among decedents with an available medical examiner or coroner report. Information represents evidence available in source documents; these are likely underestimated as death investigators might have limited information.
- Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States, 1999–2020. NCHS Data Brief, no 428. Hyattsville, MD: National Center for Health Statistics. 2021. DOI: https://dx.doi.org/10.15620/cdc:112340.
- Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. 2021.
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep 2021;70:202–207. DOI: http://dx.doi.org/10.15585/mmwr.mm7006a4
- O’Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital Signs: Characteristics of Drug Overdose Deaths Involving Opioids and Stimulants — 24 States and the District of Columbia, January–June 2019. MMWR Morb Mortal Wkly Rep 2020;69:1189–1197. DOI: http://dx.doi.org/10.15585/mmwr.mm6935a1
- O’Donnell J, Tanz LJ, Gladden RM, Davis NL, Bitting J. Trends in and Characteristics of Drug Overdose Deaths Involving Illicitly Manufactured Fentanyls — United States, 2019–2020. MMWR Morb Mortal Wkly Rep 2021;70:1740-1746.
- Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential — United States, 2003–2017. MMWR Morb Mortal Wkly Rep 2019;68:388–395. DOI: http://dx.doi.org/10.15585/mmwr.mm6817a3
- Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics; 2020. Available at http://wonder.cdc.gov.