At a glance
- CDC jointly leads the federal public health interoperability work along with the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health Information Technology (ASTP).
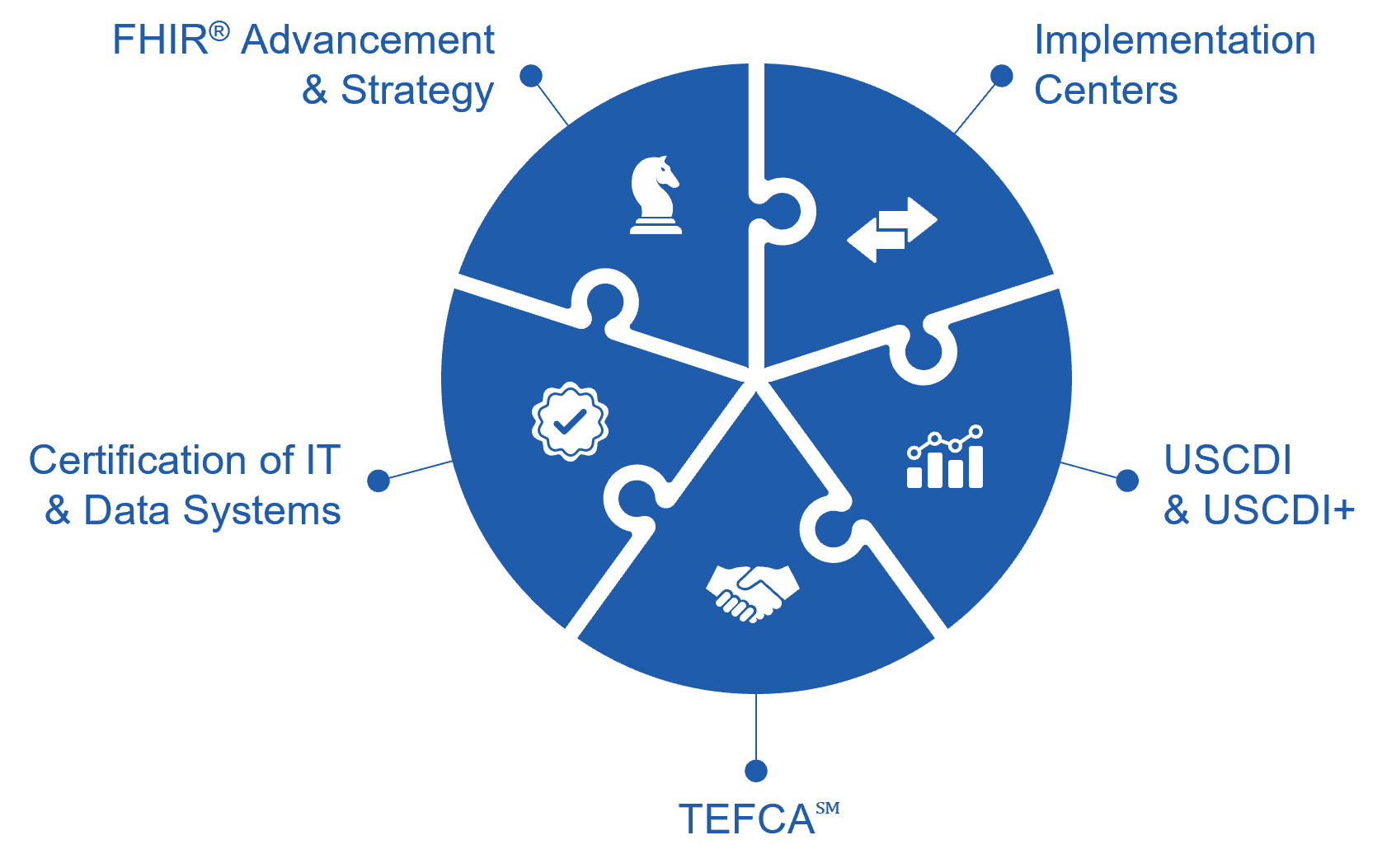
- These efforts fit together to create a multi-pronged approach designed to address the need for essential data to flow seamlessly across the public health ecosystem.
- Learn more about these efforts and why they're an important step toward public health interoperability.
Overview
CDC and the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health Information Technology (ASTP) jointly lead the federal efforts to address public health interoperability work that involves a multipronged approach.
Trusted Exchange Framework and Common AgreementSM (TEFCASM)
What is it? A common set of principles, terms, and conditions to support nationwide exchange of electronic health information for better patient, population, and public health. These principles are standardization; openness and transparency; cooperation and non-discrimination; privacy, security, and safety; access; equity; and public health.
Why Does it matter: TEFCA establishes a universal governance, policy, and technical floor for nationwide interoperability; simplifies connectivity for organizations to securely exchange information to improve patient care, enhance the welfare of populations, and generate health care value; and enables individuals to gather their healthcare information. TEFCA is designed to enable public health agencies, healthcare providers, individuals, and many more interested parties have secure, timely access to health information when and where it is needed. TEFCA will support public health agencies' efforts to transform data into action, enabling them to meet the four core public health missions, which include:
- Detect and Monitor. Simplifying information exchange will decrease the need for one-off connections to public health reporting systems. This will facilitate multiple use cases, such as electronic case reporting, immunization reporting, syndromic surveillance, or lab and registry reporting. Streamlining the pathways to public health will increase the number of entities using electronic means, rather than paper, fax or phone.
- Investigate and Respond. TEFCA exchange will allow public health agencies to send messages to providers and conduct queries to support their public health functions, including identifying incidents and informing care providers of public health concerns. In addition, those seeking certain information from public health (e.g., treatment information from public health entities acting as a provider), may be able to query for the information they need. By leveraging TEFCA exchange, public health can become more closely connected with health care providers, resulting in benefits for both.
- Inform and Disseminate. By offering more efficient data collection, TEFCA exchange will enable advanced analytics and other the creation of applications (e.g., state-level dashboards) that support public access to, and engagement with, data for individual, family, and community decision-making.
- Be Response-Ready. TEFCA exchange create an infrastructure that more readily supports exchange of real-time information needed for public health threats, allowing for ready adaptation and response to data collection needs in the event of both novel and more routine threats to public health.
Learn more:
- Learn more about how TEFCA benefits public health
- See the notice of publication for TEFCA
- Read the Trusted Exchange Framework: Principles for Trusted Exchange
- Read the Common Agreement for Nationwide Health Information Interoperability
- Learn more about TEFCA from the ONC HealthITbuzz blog: 3...2...1...TEFCA is Go for Launch
Implementation Centers
What is it? CDC awarded three national partners (ASTHO, NNPHI and PHAB)* a total of $255 million to accelerate, stand-up, and expand the capacity of four Implementation Centers (ICs). These ICs will provide technical assistance to state, tribal, local and territorial (STLT) health departments to improve public health data exchange across public health jurisdictions, healthcare, and other data providers (e.g., laboratories). Promoting the use of flexible, advanced data-sharing methods will lead to reduced burden on healthcare systems, providers, and public health entities and will increase timeliness and completeness of data, in addition to improvement in public health threat detection, response and prevention.
*National partners include The Association of State and Territorial Health Officials, National Network of Public Health Institutes, and Public Health Accreditation Board.
Why does it matter: The Implementation Centers (ICs) play an essential role in supporting our nation's health departments to obtain the necessary tools and support to modernize to the extent that the rest of the healthcare ecosystem has accomplished in the past decade. This substantial investment will support data modernization by
- Streamlining how public health agencies operate by using modern technologies;
- Reducing the burden of data exchange between public health agencies, healthcare, and the communities in which they serve; and
- Leveraging an existing multi-billion dollar investment in electronic health records to support better, more timely data for public health action.
These Implementation Centers will provide direct technical support to health departments for participation in data modernization and interoperability initiatives in public health priority areas such as electronic case reporting, participation in the Trusted Exchange Framework and Common Agreement (TEFCA), and other advancements in data access and exchange between health care and public health.
Learn more:
Public Health Information Technology Certification
What is Public Health Information Technology Certification? The ONC Health IT Certification Program is a voluntary program that helps ensure that current and future technologies are developed with interoperability in mind. Launched in 2010, the Certification Program supports the Promoting Interoperability Programs (previously Medicare and Medicaid EHR Incentive Programs) administered by the Centers for Medicare & Medicaid Services (CMS). CDC is collaborating with ONC on ways that health IT and data modernization can result in better public health data to inform population health, emergency response, and public health surveillance. The Health IT Advisory Committee, in both 2021 and 2022, explored public health data modernization and made recommendations to ONC to enhance public health data exchange interoperability. In addition, the CDC Advisory Committee to the Director recommended that CDC and ONC work with state, territory, local, and tribal partners to develop and implement a coordinated, phased approach to certification for public health use cases. ONC plans to address new ways to advance health IT for public health through proposed certification requirements in the Health Data, Technology, and Interoperability: Patient Engagement, Information Sharing, and Public Health Interoperability (HTI-2) Proposed Rule.
Why it matters: Certification ensures IT and data systems used by public health include established standards, implementation specifications, and certification requirements adopted by the Secretary at the Department of Health and Human Services (HHS). Establishing standards helps advance broader strategies for public health data interoperability by reducing the burden associated with public health data exchange for both healthcare and public health providers. Additionally, upstream public health IT standardization permits downstream surveillance data use to identify health inequities and use by public health programs to protect lives and improve health.
Learn more:
- Health Data, Technology, and Interoperability: Patient Engagement, Information Sharing, and Public Health Interoperability (HTI-2) Proposed Rule
- CDC Advisory Committee to the Director (ACD) Data and Surveillance Workgroup Report November 2022
- Looking Forward: HTI-2 & ONC's Commitment to Furthering the Vision of Better Health Enabled by Data - Health IT Buzz Health IT Buzz
- About The ONC Health IT Certification Program | HealthIT.gov
USCDI and USCDI+ for Public Health
What is USCDI? The United States Core Data for Interoperability is an ONC-led initiative to provide a common core of standardized data to support the exchange of clinical and administrative data for treatment, payment, healthcare operations, requests from patients, post-market surveillance, research, public health, and other authorized uses.
What is USCDI+? USCDI+ extends the USCDI standard for specific public health use cases. It aligns with certified health IT requirements and involves a discovery process, use case identification, and data evaluation. The new USCDI+ platform enhances user experience by facilitating dataset comparison, analysis, and harmonization.
Why it matters: Inclusion in USCDI and USDCI+ makes mission-critical data more consistent, compatible, and usable for interoperable public health and healthcare purposes.
Learn more:
- Learn more about USCDI and USCDI+
- Read the blog: Thinking Outside the Box: The USCDI+ Initiative
FHIR® Advancement and Strategy
What is FHIR? HL7® FHIR® is an interoperability standard, alternative to HL7® version 2 and HL7® CDA, designed to allow data, including clinical and administrative data, to quickly and efficiently move between healthcare and public health agencies.
Why it matters: HL7® FHIR® is the standard adopted by the Office of the National Coordinator for Health IT (on behalf of HHS) for application programming interfaces (APIs) to advance interoperability "without special effort" on the part of the user. FHIR® resources are designed to be easily understood and readily exchanged, taking advantage of standard internet protocols to allow for more efficient data exchange between systems and devices. FHIR® promotes effective communication and ensures data are exchanged appropriately between healthcare and public health partners in the right format, through the right channel at the right time. FHIR® also potentially simplifies implementation, reduces maintenance needs, and decreases costs for public health.
Learn more:
- Learn about Helios
- Learn about Public Health FHIR® Playbook. This Public Health FHIR® Playbook has been designed by the Public Health FHIR® Implementation Collaborative (PHFIC) to help state, tribal, local, and territorial (STLT) public health agencies successfully implement FHIR®, a standard for electronic health data exchange.
Disclaimer: HL7®, and FHIR® are the registered trademarks of Health Level Seven International and their use of these trademarks does not constitute an endorsement by HL7.
