Key points
- Crimean-Congo hemorrhagic fever (CCHF) is a rare, serious viral disease spread to humans by tick bites or infected animal blood.
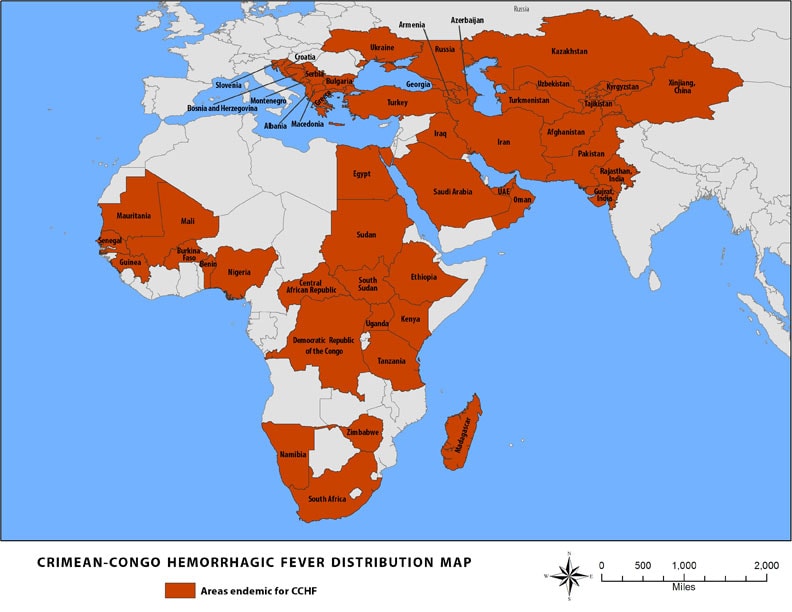
- CCHF is the most widespread viral hemorrhagic fever, found in Eastern and Southern Europe, the Mediterranean, northwestern China, central Asia, Africa, the Middle East, and the Indian subcontinent.
- Healthcare workers and people in close contact with livestock are at higher risk for CCHF.

Overview
CCHF is caused by the Crimean-Congo hemorrhagic fever virus, which is spread by ticks. The CCHF virus can cause sudden illness. CCHF can spread between humans through contact with infectious blood or body fluids. It can result in severe bleeding and death. There's no cure for CCHF.
Signs and symptoms
CCHF symptoms usually appear suddenly and may include:
- High fever
- Severe headache
- Back and joint pain
- Stomach pain and vomiting
- Red eyes and flushed face
- Red spots on the roof of the mouth
- Jaundice
- Changes in mood and sensory perception
- Agitation
- Drowsiness
- Bleeding
People with CCHF are usually sick for about two weeks. Around the fourth day of illness, large areas of severe bruising, severe nosebleeds, and uncontrolled bleeding at injection sites can develop.
Up to 50% of people hospitalized with CCHF will die.
Risk factors
The following groups of people are at a higher risk of CHHF:
- People in close contact with livestock in areas where CCHF is found
- Healthcare workers caring for someone with CCHF without proper PPE
How it spreads
CCHF virus spreads through:
- Tick bites from infected hard ticks (Ixodid)
- Contact with blood or body fluids of infected animals or humans
- Improperly sterilized medical equipment
Healthcare acquired infections are common.
Prevention
To prevent CCHF:
- Use DEET-containing insect repellent to prevent tick bites.
- Wear gloves, long sleeves, and pants when handling animals where CCHF is found.
- Avoid contact with body fluids of potentially infected animals or people.
If CCHF is suspected and the patient is clinically stable: Healthcare providers should use PPE for clinically stable suspect VHF patients.
If CCHF is suspected and the patient is clinically unstable (for example, hemodynamic instability, vomiting) OR CCHF is confirmed regardless of clinical stability: Healthcare providers should use PPE for clinically unstable VHF patients.
Testing and diagnosis
Healthcare providers diagnose CCHF with the following tests:
- Real-time polymerase chain reaction (RT-PCR)
- Detection of antibodies in the blood
CCHF is a notifiable condition. Healthcare providers should notify their health department if they suspect a patient has CCHF.
Treatment and recovery
There is no specific treatment or cure for CCHF.
- Supportive care includes fluid balance, giving oxygen, managing blood pressure, and treating other infections.
- An antiviral called Ribavirin has shown some benefits in treating CCHF patients.
- Recovery is slow, and the long-term effects are not well-studied.
- More research is needed to determine the efficacy of ribavirin and other antiviral drugs in treating CCHF.
- Khan A, et al. Viral Hemorrhagic Fevers. Seminars in Pediatric Infectious Diseases. Philadelphia: WB Saunders Co., 1997;8 (suppl 1):64-73.
- Peters CJ. Viral Hemorrhagic Fevers. Viral Pathogenesis. New York: Lippincott-Raven Publishers, 1997:779-794.
- Khan AS, et al. Viral Hemorrhagic Fevers and Hantavirus Pulmonary Syndrome. In HF Conn, RH Clohecy, RB Conn, eds. Current Diagnosis 9. Philadelphia: WB Saunders Co., 1997:193-194.
