Key points
- Symptoms of invasive candidiasis are non-specific but often include fever and chills.
- Blood cultures are used to diagnose invasive candidiasis.
- Candidemia is the most common type of bloodstream infection in the U.S.
- Other forms of infection include: endocarditis, peritonitis, meningitis, osteomyelitis, arthritis, and endophthalmitis.
- Echinocandin antifungals are the most common treatment; antifungal susceptibility testing may be necessary.

Etiology
Candida albicans, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei are most common. Species distribution varies by patient population and geographic region.
Reservoir
Candida is a commensal organism of the gastrointestinal tract and skin.
Risk factors
Common risk factors for invasive candidiasis include:
- Critical illness with a prolonged intensive care unit stay.
- Presence of central venous catheters.
- Use of broad-spectrum antibiotics or total parenteral nutrition.
- Hematologic or solid organ malignancy, or neutropenia.
- Stem cell transplantation.
- Abdominal surgery (especially in the presence of an anastomotic leak).
- Pre-term infancy with a very low birth weight.
- Renal failure or hemodialysis
- Injection drug use.
How it spreads
Most infections arise from the endogenous flora of patients with risk factors following disruption of skin and mucosal barriers. Less commonly, Candida can be transmitted via healthcare workers' hands or contaminated medical devices.
The most common invasive infections spread through the bloodstream, referred to as candidemia.
Clinical features
Signs and symptoms of invasive candidiasis are often non-specific and include fever and chills that do not respond to antibacterial treatment. While Candidemia is most common, other forms include endocarditis, peritonitis, meningitis, osteomyelitis, arthritis, and endophthalmitis.
Candida auris has emerged globally since 2009, including in the United States from mid-2015, and is very concerning because it is highly antimicrobial resistant, causes invasive infections associated with high mortality, and spreads easily between patients in healthcare settings.
Prevention
In healthcare settings, these measures are important to prevent invasive candidiasis:
- Adhering to hand hygiene recommendations
- Following recommendations for placement and maintenance of central venous catheters
- Practicing antimicrobial stewardship
Some groups of patients may benefit from antifungal prophylaxis:
- Some solid organ transplant recipients
- High-risk ICU patients
- Patients with chemotherapy-induced neutropenia
- Stem cell transplant recipients with neutropenia

Diagnosis
Invasive candidiasis is primarily diagnosed with blood culture. Newer culture-independent diagnostic methods are promising but are not yet widely used. The Beta-D-glucan assay is approved as an adjunctive diagnostic tool but is not a very specific test for Candida. Determining the species of Candida causing the infection is important to guide appropriate antifungal treatment.
Treatment of candidemia and invasive candidiasis
Initial treatment
For most adult patients with candidemia, an echinocandin is recommended as initial therapy. Fluconazole is an alternative initial treatment in patients who are not critically ill when fluconazole-resistance is considered unlikely. Other treatments include voriconazole and amphotericin B formulations.
Transitional treatment
The infectious Diseases Society of America (IDSA) recommends retesting patients every day or every other day. Once blood cultures clear transition to fluconazole if susceptible to azoles.
Duration of treatment
In general, treatment should continue for two weeks after clearance of Candida and resolution of symptoms. Intravenous catheter removal is recommended for non-neutropenic patients and can be considered for neutropenic patients.
For neonatal candidiasis, the recommended primary treatment is amphotericin B deoxycholate or fluconazole. The treatment duration is two weeks after clearance of Candida from the bloodstream and symptom resolution.
Treatment for invasive candidiasis including candidemia vary by type of infection.
Surveillance and statistics
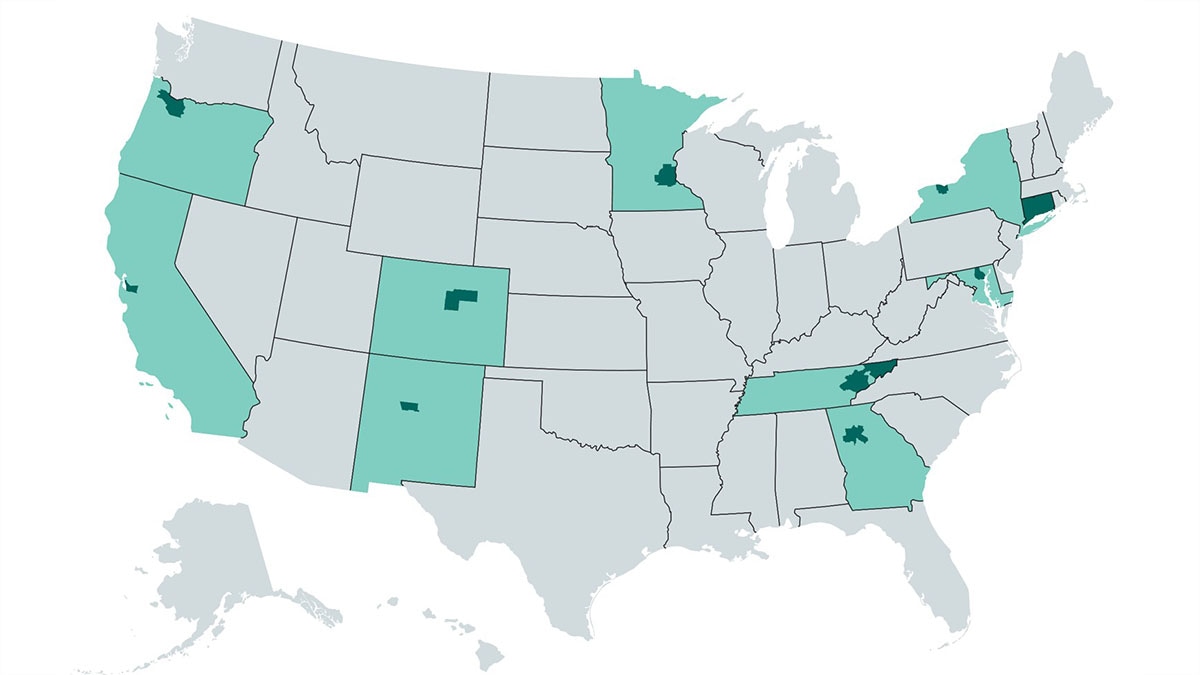
CDC performs active population-based surveillance for Candida bloodstream infections in certain areas. See surveillance and statistics.
Areas for further research
Candidemia is one of the most common bloodstream infections in the United States and invasive candidiasis is associated with an in-hospital all-cause mortality of approximately 30%. To help reduce the impact of invasive candidiasis, more research is needed to:
- Describe the national burden of candidemia
- Identify new and emerging risk factors for invasive candidiasis
- Target areas for intervention and prevention strategies
- Further develop laboratory methods to more rapidly diagnose Candida infections and detect antimicrobial resistance
- Better understand the drivers, mechanisms, and public health burden of antimicrobial-resistant Candida infections to identify the best prevention methods.
