At a glance
- Antibiotic stewardship is the effort to improve antibiotic use so that antibiotics are prescribed and used when they provide a clear benefit.
- This report provides an overview of CDC's antibiotic stewardship activities and emphasizes the importance of fostering collaboration to improve patient safety across the spectrum of health care.
Introduction
Improving antibiotic use is a core strategy to optimize patient safety and combat antimicrobial resistance. CDC tracks antibiotic use and stewardship implementation data to evaluate progress and improve health care quality by identifying opportunities for improving prescribing.
CDC's Office of Antibiotic Stewardship works with partners including healthcare organizations, academic researchers, professional societies, and public health and federal partners to improve antibiotic use and support stewardship implementation.
Data for action
CDC monitors antibiotic use and antibiotic stewardship implementation in different healthcare settings using a variety of data sources. These data are important to characterize prescribing trends and inform antibiotic stewardship interventions.
Spotlight
View antibiotic use and stewardship data on Antimicrobial Resistance & Patient Safety Portal (cdc.gov)
National outpatient antibiotic prescriptions dispensed in U.S. retail pharmacies are reported yearly from the IQVIA® Xponent database by state, age, sex and antibiotic class.
The total antibiotic use rate in 2023 was 756 prescriptions per 1,000 population.
Prescribing during 2022 achieves WHO AWaRe classification goals
The World Health Organization (WHO) Expert Committee on Selection and Use of Essential Medicines classifies antimicrobials into three groups (Access, Watch, and Reserve), which consider the impact of antibiotics on the development of antimicrobial resistance and emphasizes the importance of their appropriate use. The WHO 13th Program of Work established a goal that at least 60% of all antibiotics used are in the Access category.
- In 2022, outpatient antibiotic prescribing in the United States exceeded this target by 10.5% (70.5%).
- Also in 2022, 29.5% of antibiotic prescriptions were from the Watch category, and 0.08% were from the Reserve category.
Agents commonly prescribed from the Watch category (e.g., azithromycin, cefdinir, and ciprofloxacin) remain important targets for ongoing antibiotic stewardship efforts.
Prescriptions among Medicare Part D Beneficiaries during 2017-2022
Outpatient antibiotic prescribing utilizes publicly available data by the Centers for Medicare & Medicaid Services (CMS). The population eligible for Medicare Part D enrollment includes adults ages ≥65 years and adults ages <65 years with qualifying disabilities (13-16%). Antibiotic prescribing by state, geographic region and prescriber specialty are included and will be updated yearly.
Antibiotic use
The Antimicrobial Use (AU) Option of the National Healthcare Safety Network (NHSN) is a resource to monitor and benchmark antibiotic use in U.S. acute care hospitals. The Standardized Antimicrobial Administration Ratio (SAAR) is a risk-adjusted summary measure available to hospitals participating in the NHSN AU Option and posted yearly by state, population and agent category.
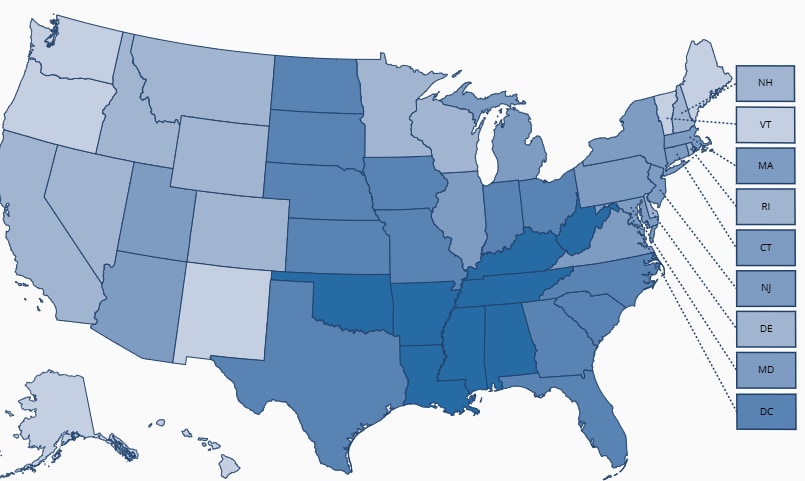
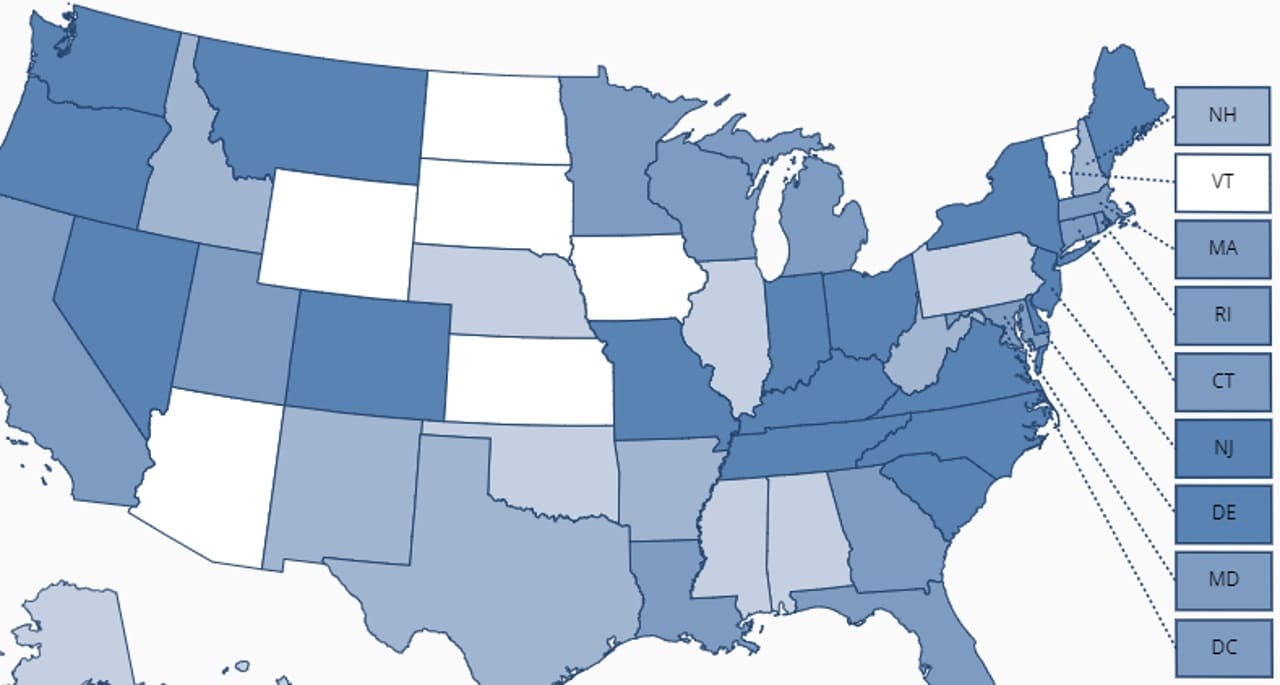
In 2023, 3,153 acute care hospitals across the United States have submitted at least one month of data to the NHSN AU Option. In the coming years, more hospitals will be reporting to the NSHN AU Option through CMS's Promoting Interoperability Program.
CDC authors outlined how expanded reporting and access to antibiotic use data can identify where prescribing can be improved and provide benchmarks for antibiotic stewardship programs. Enabling regional and national comparisons of antibiotic use, while taking into account antimicrobial resistance and healthcare-associated infection data, will help inform, implement and assess stewardship interventions.1
Hospital Antibiotic Stewardship Core Elements and Priorities
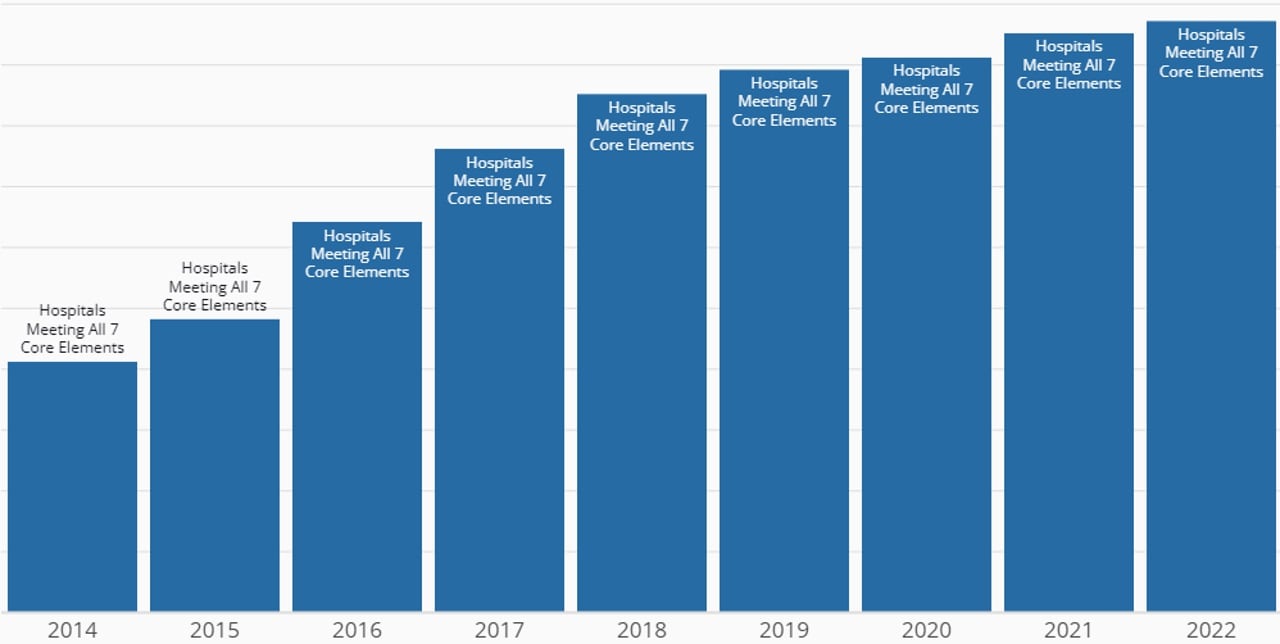
CDC's Core Elements of Hospital Antibiotic Stewardship provides a framework for the implementation of antibiotic stewardship programs (ASPs). The implementation of antibiotic stewardship programs in acute care hospitals is assessed through the NHSN Patient Safety Component Annual Hospital Survey. Staff in hospitals complete annual survey questions that assess the uptake of CDC's Core Elements. CDC reports the percentage of hospitals meeting the Core Elements by year and state.
- The percentage of hospitals meeting all 7 Core Elements increased from 41% in 2014 to 96% in 2023.
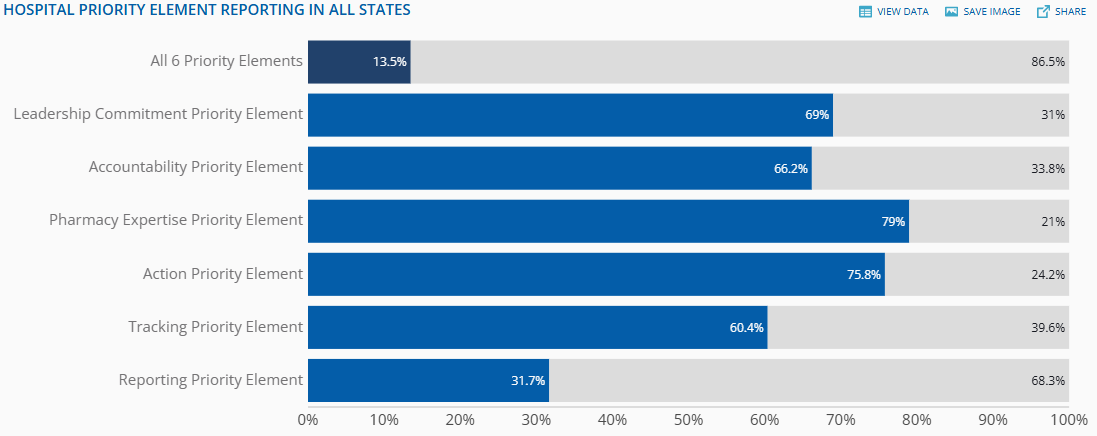
With robust national uptake of the Core Elements, CDC released Priorities for Hospital Core Element Implementation (Priorities) in Fall 2022 to enhance the quality and impact of hospital ASPs.
Priorities are a subset of effective antibiotic stewardship implementation approaches identified in six of the seven Hospital Core Elements. The Priorities are supported by evidence and/or recommended by antibiotic stewardship experts.
- In 2023, the percentage of hospitals meeting all six Priorities was 13% and hospitals meeting five of the six Priorities was 29%.
The NHSN Patient Safety Component Annual Hospital Survey questions from 2014 to 2021 were analyzed to evaluate specific antibiotic stewardship practices.
- Recommended practices which increased during this time period included listing antibiotic stewardship in program leaders' job descriptions, programs co-led by a physician and pharmacist, and audit and feedback interventions.2
Antibiotic Use
CDC analyzed antibiotic dispense data from long-term care pharmacies from 2013 to 2021.
- The percent of residents receiving at least one antibiotic each year decreased from 51% in 2013 to 44% in 2021.
- Fluoroquinolone and macrolide prescribing decreased by 49% and 30% respectively, whereas tetracycline prescribing (e.g., doxycycline) increased by 56%.
- Regulatory requirements for antibiotic stewardship programs in long-term care facilities, safety concern for specific antimicrobial agents, and the COVID-19 pandemic may have contributed to these changes.3
Ongoing measurement of antimicrobial use in long-term care is critical to informing antibiotic stewardship efforts.
Long-Term Care Antibiotic Stewardship Core Elements
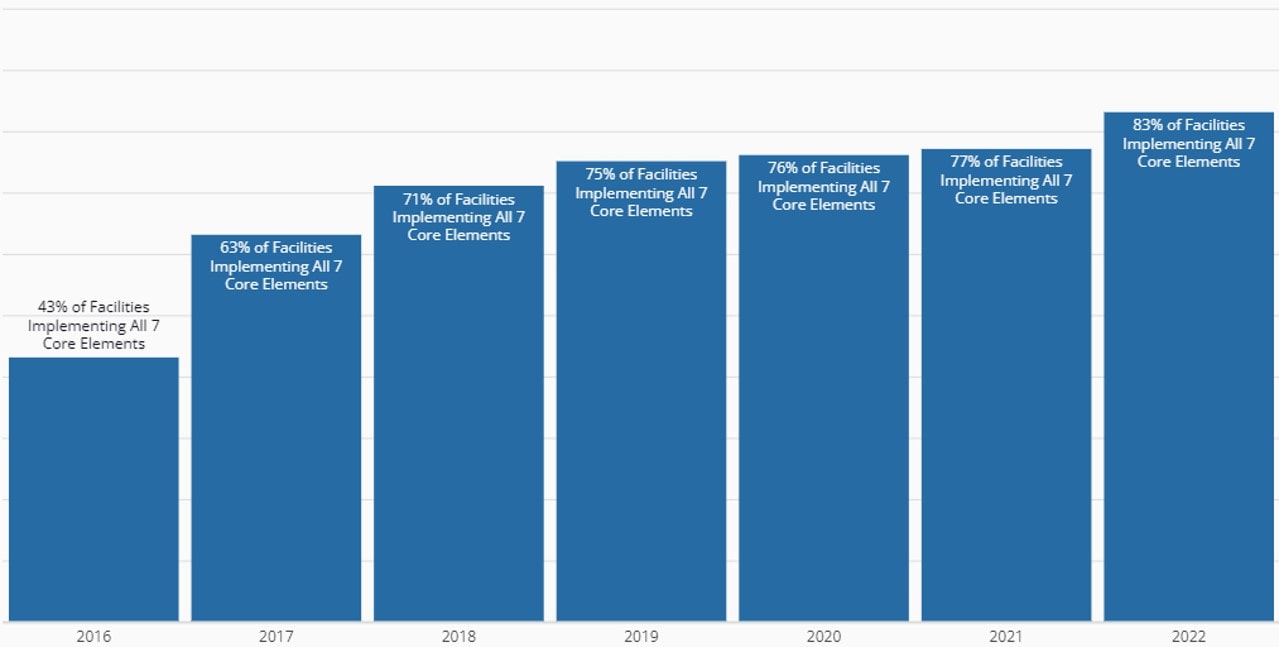
Similar to hospitals, CDC monitors the uptake of the Core Elements of Antibiotic Stewardship in Nursing Homes through the NHSN Long Term Care Facility Component—Annual Facility Survey. Staff who work in long-term care facilities, including skilled nursing facilities/nursing homes, complete annual surveys. CDC reports the percentage of long-term care facilities meeting the Core Elements by year and state.
- The percentage of long-term care facilities meeting all 7 Core Elements increased from 43% in 2016 to 82% in 2023.
Core Elements between 2019-2022
In 2022, most facilities completing the NHSN long-term care annual facility survey reported having access to electronic health records, with medication order and medication administration capabilities.
- Tracking antibiotic use was performed using manual tracking (48%), electronic health records (31%), and pharmacy data (25%).
- Electronic reporting of antibiotic use may help reduce burden on long-term care staff and provide standardized AU reports for identifying improvement opportunities and assessing the intervention effectiveness.4
Findings from CDC studies
Studies supported by CDC's Office of Antibiotic Stewardship help guide stewardship implementation strategies and identify opportunities for partners to optimize antibiotic use.
CDC characterized antibiotic prescribing by general dentists during 2018–2022 to assess whether antibiotic use changed after the release of American Dental Association (ADA) guidelines for the treatment of dental pain and swelling in 2019. The results highlight the importance of antibiotic stewardship in the dental setting.
- Despite evidence of opportunities to improve antibiotic use and the release of the ADA guidelines, total antibiotic prescribing by general dentists remained relatively stable during 2018–2022.
- Meanwhile, general dentists' relative share of all outpatient antibiotic prescriptions increased to over 10% in recent years.5
CDC examined antibiotic prescribing patterns for outpatient visits for acute sinusitis among privately-insured adults <65. The study emphasizes the opportunity to improve antibiotic prescribing for acute sinusitis in adults, especially in rural and urgent care settings.
- Approximately 30% of patient encounters resulted in antibiotic prescriptions that weren't consistent with clinical practice guideline recommendations.
- A large portion of first- (75%) and second-line (63%) agents prescribed exceeded the recommended duration for therapy.
- People living in rural areas or seeking care in urgent care settings were less likely to receive antibiotic prescriptions consistent with guideline recommendations.6
- Multiplex molecular syndromic panels are rapid diagnostic assays that can detect multiple bacteria and antimicrobial resistance genes simultaneously. This increased test sensitivity can make clinical decision-making more complex because test results do not reliably predict whether bacteria, pathogens, and resistance genes are the causes of a disease.
- Multiplex molecular panels for the diagnosis of urinary tract infections (UTIs) lack clinical data supporting their use in routine clinical care. They also have the potential to exacerbate inappropriate antibiotic use.
- The number of Medicare claims for multiplex molecular tests for urinary tract infections increased over a 50-fold between 2016-2023.
- The median cost of multiplex testing is over 70 times higher than the median cost of a urine culture, which are recommended by clinical guidelines for the diagnosis of urinary tract infections.7
CDC's Core Elements of Hospital Diagnostic Excellence described key elements and actions to improve diagnosis of infections in the hospital.
The impact of COVID-19 on antibiotic use
CDC has leveraged a variety of data sources to characterize antibiotic use in different healthcare settings during the COVID-19 pandemic to support appropriate antibiotic use.
Outpatient antibiotic prescribing volume (prescriptions per 1000 persons) was lower during 2020 to 2022 compared to 2019.
- However, CDC observed that antibiotic prescribing approached or exceeded this 2019 baseline in the last quarter of 2022 for all antibiotics, including for azithromycin, suggesting a return to antibiotic prescribing trends observed prior to the pandemic.
- Effective implementation of antibiotic stewardship combined with tracking of antibiotic prescribing are needed to optimize antibiotic use in outpatient settings following the COVID-19 pandemic.8
- From January 2019 through July 2022, although increases in antibiotic use were expected early in the pandemic while the incidence of secondary bacterial infections and antibiotic treatment benefits were unclear, rates of azithromycin and ceftriaxone use increased during each subsequent COVID-19 wave even though data emerged showing antibiotics provide no benefit.
- This emphasizes the need for effective communication and healthcare facility resiliency and support to maintain antibiotic stewardship program activities during pandemics.9
CDC described antibiotic use among U.S. adults discharged with a COVID-19 diagnosis from 711 hospitals between March 2020-June 2022.
- Despite a decrease in overall antibiotic use, most patients hospitalized with COVID-19 were started on antibiotics during their hospital admission (88.1%), regardless of critical care status.
- Since antibiotics do not treat COVID-19, this suggests that antibiotic use may be higher than necessary among patients with COVID-19, highlighting that more efforts are needed to optimize antibiotic therapy in hospitalized patients with COVID-19. 10
Antibiotic stewardship in health departments
State and local health department antibiotic stewardship programs play an important role in promoting appropriate antibiotic use in their communities and in guiding antibiotic stewardship across different healthcare settings. The Health Department Core Elements framework was adapted to outline structural and procedural components that are associated with successful public health antibiotic stewardship programs.
- In 2020, CDC expanded funding to state and local health departments to ensure that all healthcare settings have access to antibiotic stewardship expertise.
- From August 2022 to July 2023, with funding from CDC, 56 public health department antibiotic stewardship programs implemented over 380 activities aimed at improving antibiotic use.
- Most health departments hired antibiotic stewardship leads/co-leads, most commonly a pharmacist and/or physician, to support stewardship activities.
- Antibiotic stewardship activities most commonly included an education and communication component (68% of reported activities). These stewardship activities include engaging with healthcare professionals, disseminating education resources to patients and providers, and collaborating with a variety of partners to tailor antibiotic stewardship efforts to local communities.
The increased funding enabled increased engagement with healthcare facilities, outreach to healthcare professionals, and enhanced capacity for antibiotic stewardship implementation across the spectrum of human health care.
Be Antibiotics Aware campaign updates
CDC's Be Antibiotics Aware national educational effort aims to optimize antibiotic prescribing and use to improve patient safety and healthcare quality and combat antimicrobial resistance by raising knowledge, awareness and motivating behavior change among target consumer and healthcare professional (HCP) audiences. Over the past year, Be Antibiotics Aware has engaged in continuous paid media buys, developed new campaign graphics and materials for target audience groups, and increased social media presence across CDC platforms. The Clostridiodes difficile (C. diff) educational effort is a part of Be Antibiotics Aware and aims to optimize antibiotic prescribing and use to improve patient safety, combat antibiotic resistance, and prevent C. diff infections by raising knowledge, increasing awareness, and motivating behavior change among intended HCPs.
Through the award-winning national educational efforts, Be Antibiotics Aware and Get Ahead of Sepsis, CDC educates the public and healthcare professionals about the importance of antibiotic stewardship to ensure appropriate and timely antibiotic use. This includes the optimization of sepsis management and reduction of C. diff infection risk.
Paid media
For the first time ever, since December 2023, Be Antibiotics Aware has run continuous paid advertisements to raise awareness of key messages and materials, drive traffic to relevant content pages, and generate engagement. From Dec 2023-July 2024 paid advertisements included programmatic ads, social media content (Instagram, Facebook, LinkedIn, and YouTube), and out of home advertisement placements which collectively generated over 23 million impressions and 210,000 link clicks to the CDC website.
Web
From June 1, 2023-May 15, 2024, CDC's antibiotic use website garnered 11M+ page views and 302K+ material downloads
- 18K+ partner toolkit page views during USAAW 2023
Antibiotic stewardship resources
CDC's Office of Antibiotic Stewardship worked with professional society and academic partners to develop resources to support improving antibiotic use.
- CDC funded the Duke Antimicrobial Stewardship Outreach Network to develop interactive web-based tools to leverage NHSN AU Option data to inform, implement, and assess antibiotic stewardship activities. The guide illustrates 15 clinical scenarios for using NHSN AU Option data for action.
- The Infectious Diseases Society of America (IDSA) created a clinical pathway for the diagnosis and treatment of inpatient community- acquired pneumonia as a part of a collaboration between IDSA and CDC. The clinical pathway incorporates diagnostic and antibiotic stewardship principles.
- CDC funded the Society for Healthcare Epidemiology of America (SHEA) to develop online educational modules on Penicillin Allergy Delabeling.
- CDC funded the Association for Dental Safety (ADS) (formerly known as OSAP) to organize and host the 2nd annual national Antibiotic Stewardship Summit to disseminate knowledge and resources for antibiotic stewardship in the dental setting.
- The Antibiotic Stewardship Resource Bundles organize CDC and partner stewardship resources for antibiotic stewards and healthcare professionals by setting of care, audience, and type of resource.
Spotlight
The path forward
This report provides a summary of the CDC's antibiotic stewardship efforts and initiatives. CDC is expanding access to publicly available surveillance data on the Antimicrobial Resistance & Patient Safety Portal. CDC continues to support state and local health department antibiotic stewardship programs to guide and coordinate stewardship activities and collaboratives with a variety of partners in their jurisdictions. Expanding antibiotic stewardship educational materials for families and school-aged children can help better ensure that the next generation of patients and patient safety advocates will grow up antibiotics aware. CDC will continue to update antibiotic stewardship guidance and healthcare professional resources to better account for new evidence-based strategies and changes in health care delivery.
- Neuhauser MM, Webb AK, Srinivasan A. National Healthcare Safety Network Antimicrobial Use Option reporting … finding the path forward. Antimicrob Steward Healthc Epidemiol. 2023;3(1):e183. doi:10.1017/ash.2023.430
- O'Leary EN, Neuhauser MM, McLees A, Paek M, Tappe J, Srinivasan A. An Update From the National Healthcare Safety Network on Hospital Antibiotic Stewardship Programs in the United States, 2014-2021. Open Forum Infect Dis. Feb 2024;11(2):ofad684. doi:10.1093/ofid/ofad684
- Gouin KA, Creasy S, Beckerson M, Wdowicki M, Hicks LA, Kabbani S. Description of national antibiotic prescribing rates in U.S. long-term care facilities, 2013-2021. In press. Antibiotic Stewardship and Hospital Epidemiology. November 2024;
- Luciano A, Kabbani S, Neuhauser M, McCray T, Robinson L, Rowe T, Gouin KA. Implementation of the Core Elements of Antibiotic Stewardship in Long-term Care Facilities, 2019-2022. Provisionally accepted in October 2024. Antibiotic Stewardship and Hospital Epidemiology.
- Huynh CT, Gouin KA, Hicks LA, Kabbani S, Neuberger M, McDonald E. Outpatient antibiotic prescribing by general dentists in the United States, 2018–2022. Journal of the American Dental Association. 2024;
- Vazquez Deida AA, Bizune DJ, Kim C, Sahrmann JM, Sanchez GV, Hersh AL, Butler AM Hicks LA, Kabbani S. Opportunities to Improve Antibiotic Prescribing for Adults With Acute Sinusitis, United States, 2016-2020. Open Forum Infect Dis. 2024 Jul 23;11(8):ofae420. doi: 10.1093/ofid/ofae420. eCollection 2024 Aug. doi:10.1093/ofid/ofab324
- Hatfield Kelly et al. Multiplex UTIs Testing Manuscript. JAMA Network Open. 2024.
- Bizune D, Gouin K, Powell L, Hersh AL, Hicks LA, Kabbani S. Update on outpatient antibiotic prescribing during the COVID-19 pandemic: United States, 2020–2022. Antimicrobial Stewardship & Healthcare Epidemiology. 2024;4(1):e193. e193. doi:10.1017/ash.2024.398
- O'Leary EN, Neuhauser MM, Srinivasan A, Dubendris H, Webb AK, Soe MM, Hicks LA, Wu H, Kabbani S, Edwards JR. Impact of the COVID-19 Pandemic on Inpatient Antibiotic Use in the United States, January 2019 Through July 2022. Clin Infect Dis. Jan 25 2024;78(1):24-26. doi:10.1093/cid/ciad453
- Kim C, Wolford H, Baggs J, Reddy S, Hicks LA, Neuhauser MM, Kabbani S. Antibiotic Use Among Hospitalized Patients With COVID-19 in the United States, March 2020-June 2022. Open Forum Infect Dis. Nov 2023;10(11):ofad503. doi:10.1093/ofid/ofad503