At a glance
- Antibiotic stewardship is the effort to ensure that antibiotics are prescribed and used when they provide a clear health benefit.
- Improving antibiotic use is a key strategy to optimize patient safety and combat antimicrobial resistance in the United States.
- This annual report provides an overview of CDC's surveillance data on antibiotic use, along with guidance and example collaborations aimed at improving antibiotic use to optimize patient safety across all areas of health care.
Introduction
In 2014, the Centers for Disease Control and Prevention (CDC) released the Core Elements of Hospital Antibiotic Stewardship to outline structural and procedural components associated with successful antibiotic stewardship programs. Since then, the Core Elements have been adapted to different healthcare settings and specific implementation strategies have been identified, including small and critical access hospitals and dialysis settings. The Core Elements framework has also been used to support hospital programs to improve healthcare quality in other areas, such as hospital sepsis programs and diagnostic excellence.
Antibiotic stewardship guidance and resources
In 2016, CDC published the Core Elements of Outpatient Antibiotic Stewardship as a framework for clinics and clinicians to improve antibiotic prescribing in outpatient settings. Increasingly, outpatient care is provided under the umbrella of a health system.
In 2026, CDC will update the Outpatient Core Elements to focus on the role health system leadership can play in supporting the development and expansion of outpatient antibiotic stewardship programs within their networks. This updated guidance is applicable to all outpatient settings, including those with limited stewardship capacity and infrastructure, and aligns with published evidence and recommended best practices. For example, health systems can disseminate treatment recommendations based on national guidelines for common outpatient infections. Treatment recommendations can be integrated into the clinical workflow using clinical decision support tools embedded into electronic health records. The updated Core Elements guidance standardizes antibiotic stewardship implementation to improve the quality and consistency of outpatient care.
Although 10% of people in the United States report a penicillin allergy, less than 1% are truly penicillin allergic. Inaccurate penicillin allergy labels can prevent people from getting the best possible treatment for their infection. The Core Elements highlight the importance of healthcare professionals using effective methods to accurately evaluate if an individual is truly allergic to penicillin. CDC developed resources for healthcare professionals managing patients with penicillin allergy labels.
- The Clinical Features of Penicillin Allergy webpage features updated best practices and resources.
- With CDC funding, the Society for Healthcare Epidemiology of America (SHEA) created the Penicillin Allergy Management - Removing Barriers to Optimal Antibiotic Prescribing training course that provides free continuing education credits to healthcare professionals including physicians, pharmacists and advanced practice providers.
The Core Elements of Hospital Antibiotic Stewardship Programs outline opportunities to improve antibiotic use for common infections such as community-acquired pneumonia (CAP). CDC supported activities aimed at improving the treatment of patients with CAP.
- The American College of Chest Physicians created an interactive infographic on diagnostic and treatment considerations for managing CAP. This clinician educational resource was developed with CDC funding.
- A recent CDC-funded study demonstrated that providing feedback reports to clinicians on their antibiotic prescribing practices can improve adherence to treatment guidelines within a children's health system. These feedback reports were created using data from electronic health records, eliminating the need for manual chart reviews. 1
- With support from CDC, the University of Utah developed electronic clinical quality measures (eCQMs) extracted from electronic health records that focus on the appropriate treatment of hospitalized patients with uncomplicated CAP. eCQMs are designed to assess the quality of care provided to patients. University of Utah researchers submitted the quality measures to the Partnership for Quality Measurement and received "endorsed with conditions" status in April 2025.
More information on the two quality measures can be found here:
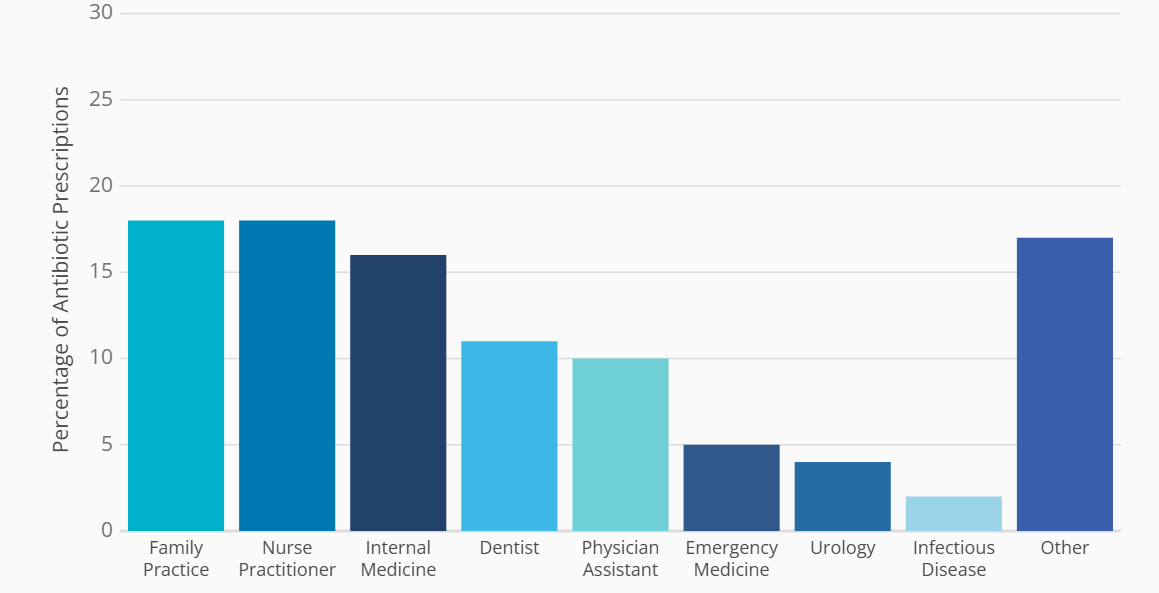
CDC reported that general dentists continue to prescribe more than 10% of all antibiotics in the outpatient setting. Dental prescribing rates remained unchanged from 2018 to 2022 despite clinical practice guidelines meant to improve antibiotic use in dentistry.2 CDC developed resources to support appropriate antibiotic prescribing in the dental setting, including:
- A guide summarizing the American Dental Association's current recommendations for treating patients with dental pain and swelling.
- A checklist outlining best practices for antibiotic prescribing in dentistry.
- Resources for dental stewardship implementation and an annual dental stewardship summit. with post-conference recordings to enhance dissemination of educational content developed by the Association for Dental Safety with support from CDC.
- Strategies dentists can use to improve patient safety by optimizing antibiotic prescribing as discussed by Dr. Erinne Kennedy on CDC's Safe Healthcare Blog.
Antibiotic use and stewardship data
Outpatient antibiotic use
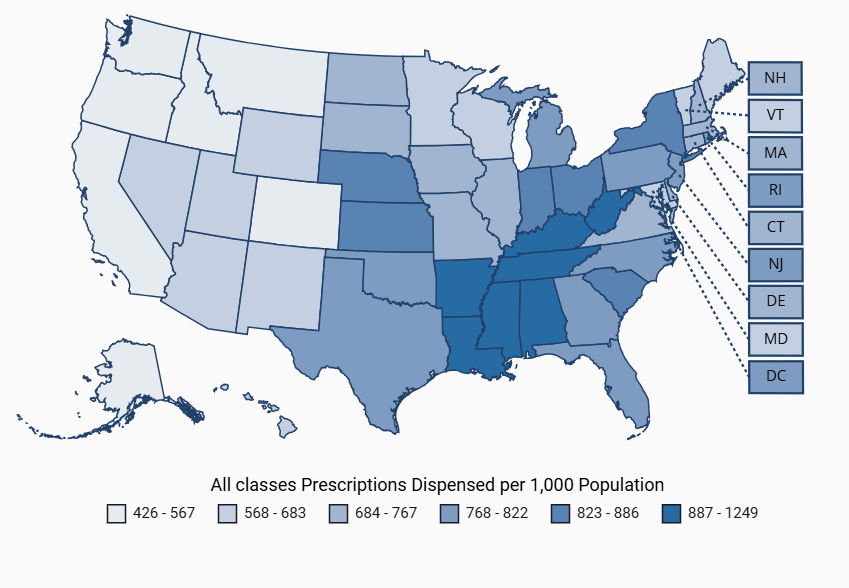
National outpatient antibiotic prescriptions dispensed in U.S. retail pharmacies are reported yearly by state, age, sex, and antibiotic class to characterize prescribing trends and inform antibiotic stewardship interventions. In 2024, the overall antibiotic prescribing rate was 752 prescriptions per 1,000 patient population, reflecting a 1% decline from 2023.
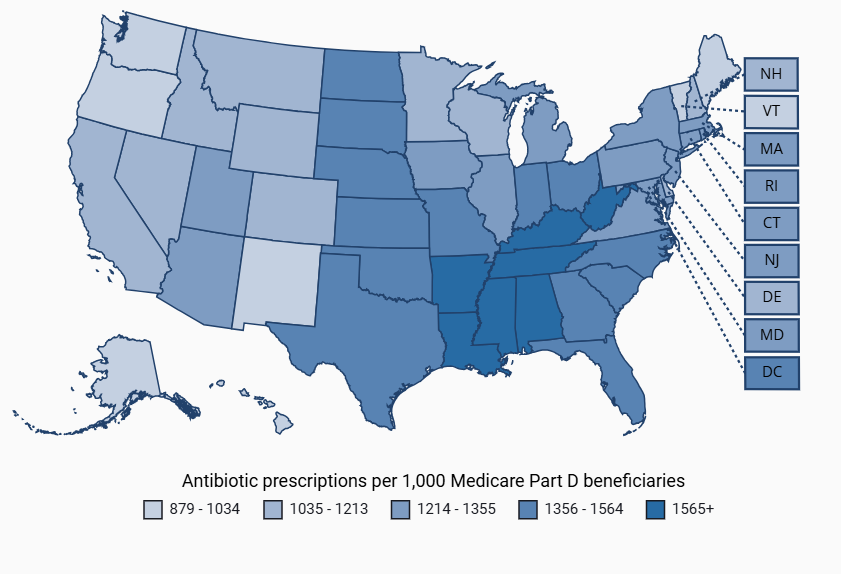
Outpatient antibiotic prescribing data for Medicare Part D enrollees shared publicly by the Centers for Medicare & Medicaid Services (CMS) are also reported by state, geographic region, antibiotic class and prescriber specialty. Outpatient antibiotic prescribing rates differ by prescriber specialty and can vary across states based on local prescribing patterns.
In 2022, family practice, nurse practitioner, and internal medicine clinicians prescribed 52% of the antibiotic prescriptions among Medicare Part D beneficiaries. Engagement with professional societies for specialties with the highest antibiotic prescribing rates provides an opportunity to promote more judicious antibiotic use and improve quality of care.
Hospital antibiotic use
The Antimicrobial Use (AU) Option of the National Healthcare Safety Network (NHSN) is a resource for U.S. acute care hospitals to monitor and compare their antibiotic use data to other facilities. As of January 1, 2025, 4,362 acute care hospitals across the United States have submitted at least one month of data to the NHSN AU Option. While it is anticipated that the remaining hospitals in the United States will be onboard in 2025, hospitals that are already enrolled will continue to report to the NHSN AU Option to fulfill a Centers for Medicare & Medicaid Services (CMS) Promoting Interoperability Program measure requirement.
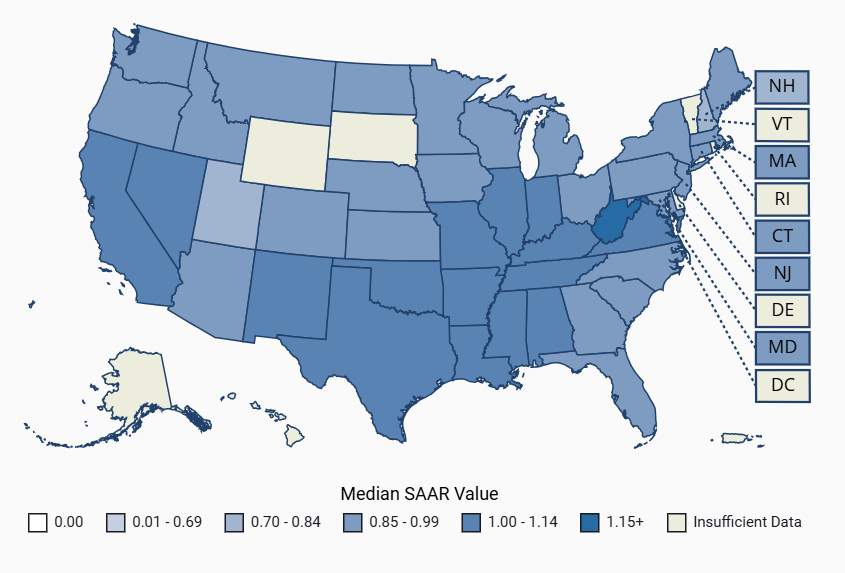
The Standardized Antimicrobial Administration Ratio (SAAR) is a risk-adjusted summary measure available to hospitals participating in the NHSN AU Option. The SAARs were updated using 2023 data, and additional facilities and patient care locations were included. The 2024 AU Option Data Report features the updated SAAR data and provides a summary of SAAR distributions and antibiotic use for each SAAR category across adult, pediatric, and neonatal patient care locations. Data are also reported annually on the Antimicrobial Resistance and Patient Safety Portal, allowing users to explore and visualize SAAR distributions at both national and state levels.
Hospital Antibiotic Stewardship Core Elements and priorities
The implementation of antibiotic stewardship core elements in acute care hospitals is assessed through the NHSN Patient Safety Component Annual Hospital Survey. Hospital staff complete annual survey questions that assess the uptake of CDC's Core Elements. CDC reports the percentage of hospitals meeting the Core Elements by year and state. In 2024, the percentage of hospitals meeting all 7 core elements was 97%.
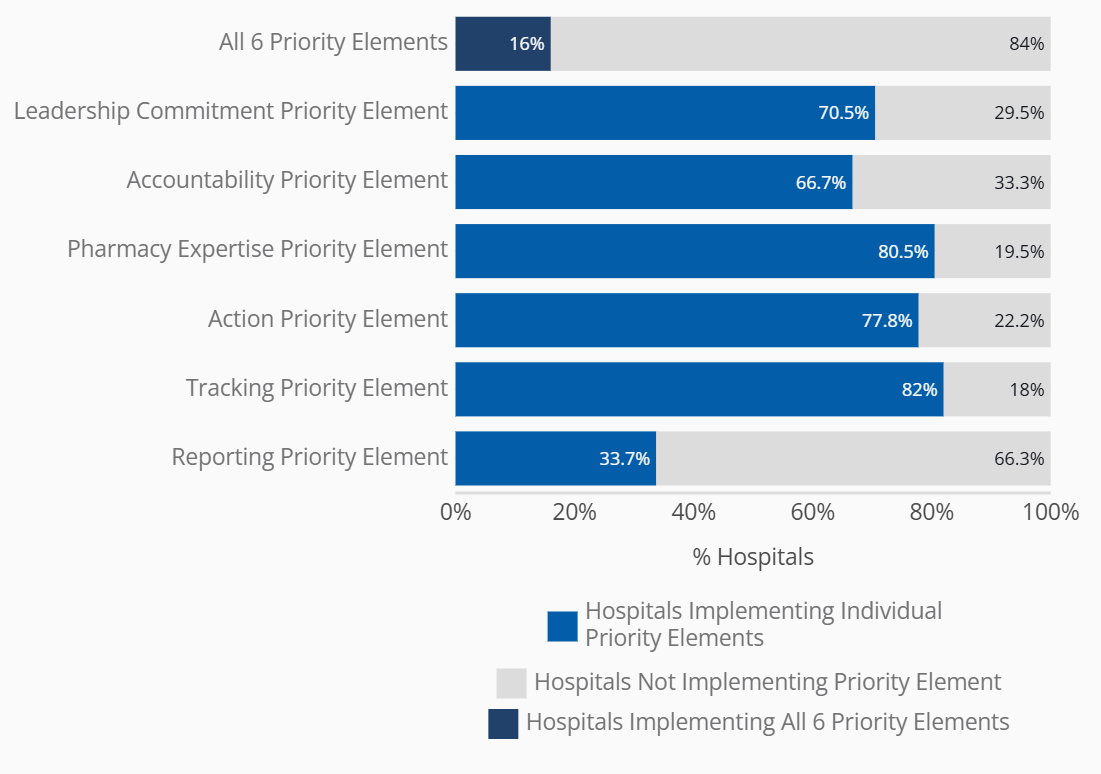
With robust national uptake of the Core Elements, CDC released Priorities for Hospital Core Element Implementation (Priorities) in Fall 2022 to enhance the quality and impact of hospital stewardship programs. In 2024, the percentage of hospitals meeting all six Priorities was 16% and hospitals meeting five of the six Priorities was 36%.
Long-term care antibiotic use
CDC updated resources to support tracking and reporting antibiotic use in long-term care settings. Beginner and advanced versions provide facility staff with an overview of data sources, data elements and antibiotics use measures. CDC is working with long-term care facilities and electronic health record vendors to develop a pilot evaluating the feasibility of reporting antibiotic use data electronically in long-term care settings.
Long-term care Antibiotic Stewardship Core Elements
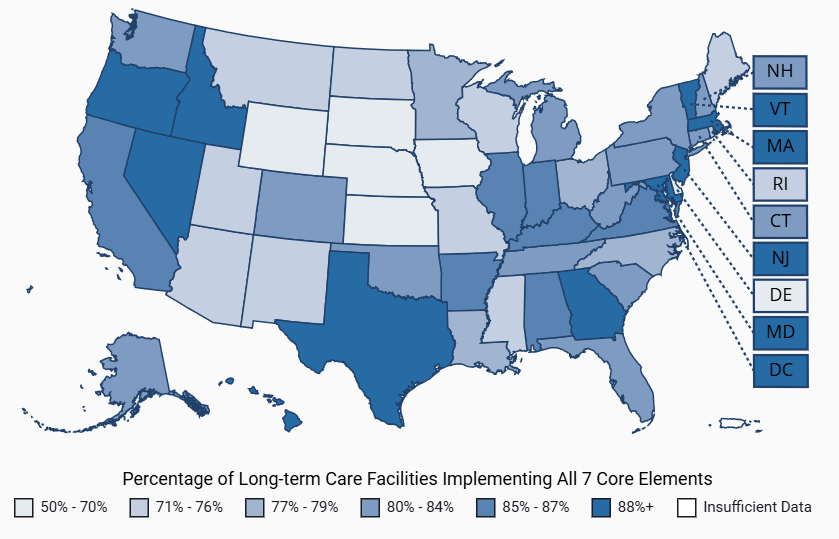
Similar to hospitals, CDC monitors the uptake of the Core Elements of Antibiotic Stewardship in Nursing Homes through the NHSN Long Term Care Facility Component—Annual Facility Survey. CDC reports the percentage of long-term care facilities meeting the Core Elements by year and state. The percentage of long-term care facilities meeting all 7 Core Elements was 82% in 2024.
Findings from CDC studies
Antibiotic Prescribing During Outpatient Telemedicine Visits Among Commercially-Insured Patients and Medicare Part D Beneficiaries, 20213
CDC looked at how antibiotics are prescribed during outpatient telemedicine visits for patients with private insurance or Medicare in 2021. Here are the key points:
- In 2021, 7% to 9% of outpatient visits during which antibiotics were prescribed were telemedicine visits.
- Antibiotic prescribing was common for respiratory conditions for which they are not needed, including acute bronchitis and viral upper respiratory infections.
- For sinusitis, about 75% of visits resulted in a prescription. Most patients with acute uncomplicated sinusitis get better without antibiotics, showing there is room for improvement.
This analysis shows that there are opportunities for improving how antibiotics are prescribed in outpatient telemedicine, especially for respiratory conditions. Adapting antibiotic stewardship strategies to virtual visits is important to ensure that antibiotics are prescribed appropriately.
Trends in intravenous antimicrobial start rates in outpatient hemodialysis centers, United States, 2012-20214
Almost one in three people on hemodialysis receives an intravenous antibiotic each year, but nearly half of those antibiotics may not be necessary. A study using NHSN data looked at the trends in new intravenous antibiotics prescription rates for patients on hemodialysis. The important takeaways are:
- From January 2012 to March 2020, the adjusted rates of intravenous antibiotics decreased by nearly 7% each year, and then, during the COVID-19 pandemic, they decreased by ~9% annually until December 2021.
- People on hemodialysis with central venous catheters had much higher rates of receiving intravenous antibiotics compared to those with another type of access like a graft or fistula.
The decrease in antibiotic use rates may be due to greater awareness of infection prevention practices and better messaging on antibiotic stewardship in hemodialysis facilities, particularly during the COVID-19 pandemic. Evaluating how clinical factors contribute to antibiotic use can help support dialysis facility staff in using data reported to NHSN and help describe the impact of stewardship efforts.
Antibiotic and Opioid Prescribing for Medicare Part D Beneficiaries, 20215
Understanding high-volume co-prescribing of antibiotics and opioids by clinicians may help inform the development of initiatives that optimize prescribing practices. A study using 2021 Medicare Part D data describing antibiotics prescribed for older adults found:
- Out of 350, 890 prescribers, the top 10% of antibiotic prescribers by volume were responsible for 12.5 million (36%) antibiotic prescriptions, while the top 10% of opioid prescribers accounted for 22.3 million (52%) opioid prescriptions.
- It was common for clinicians who prescribed a high volume of antibiotics to also prescribe a high volume of opioids.
- Prescribers in the Southern United States and in rural areas were more likely to be high-volume prescribers of both types of medications compared to other regions and urban areas.
This study highlights the potential benefit of engaging with high-volume prescribers of antibiotics and opioids, particularly those prescribing for older adult patients and in rural areas.
Antibiotic and Antiviral Prescribing for Long-Term Care Residents with a COVID-19 Diagnosis, 2020-20236
A study looked at how antibiotics and antivirals were prescribed for long-term care residents with COVID-19 from March 1, 2020, to July 31, 2023, using electronic health record data. Key findings include:
- Prior to FDA authorization of oral antivirals for treatment of COVID-19 in December 2021, 23% of COVID-19 diagnoses were associated with an antibiotic order.
- After the authorizations in December 2021, this number dropped to 17%, while 18% were associated with an antiviral prescription.
These results suggest that the availability of an effective alternative to an antibiotic (i.e., antiviral) may have reduced the inclination to prescribe antibiotics. This highlights the need to improve treatment of viral infections by using appropriate antiviral therapy and avoiding unnecessary antibiotics.
Be Antibiotics Aware campaign updates
CDC's Be Antibiotics Aware national educational effort aims to optimize antibiotic prescribing and use to improve patient safety and healthcare quality, combat antimicrobial resistance by raising knowledge and awareness about antibiotic use, and encourage changes in habits or actions among healthcare professionals and the general public.
CDC's Clostridioides difficile (C. diff) educational effort is a part of Be Antibiotics Aware and aims to optimize antibiotic prescribing and use to improve patient safety, combat antimicrobial resistance, and prevent C. diff infections by raising knowledge and awareness and encourage changes in habits or actions among healthcare professionals.
Through the award-winning national educational efforts, Be Antibiotics Aware, C. diff, and Get Ahead of Sepsis, CDC educates the public and healthcare professionals about the importance of antibiotic stewardship to ensure appropriate and timely antibiotic use. This includes the optimization of sepsis management and reduction of C. diff infection risk.
Paid media
From August 2024 to January 2025, Be Antibiotics Aware leveraged a mix of high-performing online channels (e.g., social media) to deliver messaging to both healthcare professionals and the general public to raise awareness of Be Antibiotics Aware and C. diff messages and materials, increase traffic to web pages and/or content, and generate engagement. Paid advertisements included Meta (Facebook and Instagram), LinkedIn, programmatic display ads, and out of home advertisement placements (doctor offices and pharmacies through online, on-screen advertising) which collectively garnered 14.4 million impressions and 210k+ link clicks. All paid media campaigns were paused on January 21, 2025.
Web
From May 16, 2024, to June 30, 2025, CDC's antibiotic use website garnered 6 million page views and 154,000+ material downloads. There were 6,600+ page views of the Be Antibiotics Aware partner toolkit leading up to and during U.S. Antibiotic Awareness Week (October-November 2024).
Social media
Social media remains a highly effective tool for reaching and engaging Be Antibiotics Aware consumer and healthcare professional audiences across Instagram, Facebook, X, and LinkedIn. From June 2024 to June 2025, the campaign generated 1 million impressions and 46,000+ engagements.
The path forward
This report includes updated annual data from CDC's Antimicrobial Resistance & Patient Safety Portal and summarizes national efforts to improve antibiotic prescribing in the United States. It highlights CDC's ongoing work to update antibiotic stewardship guidance and resources for common infections, including respiratory and dental infections. These updates incorporate the latest scientific evidence and reflects changes in healthcare delivery. CDC is committed to working with public health and healthcare partners including healthcare payers to improve outpatient antibiotic use. Healthcare payers can monitor the quality of antibiotic prescribing and provide feedback to healthcare professionals to facilitate quality improvement. To support these efforts, CDC shares timely and actionable antibiotic use data to guide quality improvement, ensure patient safety and address antimicrobial resistance.
Past reports
- 2024 Report: Antibiotic Use in the United States
- 2023 Report: Antibiotic Use in the United States
- 2022 Report: Antibiotic Use in the United States
- 2021 Report: Antibiotic Use in the United States
- 2020 Report: Antibiotic Use in the United States
- 2018 Report: Antibiotic Use in the United States
- 2017 Report: Antibiotic Use in the United States
- Chiotos K, Dutcher L, Grundmeier RW, Meyahnwi D, Lautenbach E, Neuhauser MM, Hicks LA, Hamilton KW, Li Y, Szymczak JE, Muller BM, Congdon M, Kane E, Hart J, Utidjian L, Cressman L, Jaskowiak-Barr A, Gerber JS. Impact of Clinician Feedback Reports on Antibiotic Use in Children Hospitalized With Community-acquired Pneumonia. Clin Infect Dis. 2025 Feb 24;80(2):263-270. doi: 10.1093/cid/ciae593. PMID: 39656188; PMCID: PMC12120840.
- Huynh CT, Gouin KA, Hicks LA, Kabbani S, Neuburger M, McDonald E. Outpatient antibiotic prescribing by general dentists in the United States from 2018 through 2022. J Am Dent Assoc. 2025 May;156(5):382-389.e2. doi: 10.1016/j.adaj.2024.12.003. Epub 2025 Mar 6. PMID: 40047737; PMCID: PMC12058375.
- Sanchez GV, Bizune D, Kim C, Hicks L, Hersh AL, Kabbani S. Antibiotic prescribing during outpatient telemedicine visits among commercially insured patients and Medicare Part D beneficiaries, 2021. Infect Control Hosp Epidemiol. 2025 Nov 19. doi:10.1017/ice.2025.10250
- Wilson WW, Hua H, Li Q, Soe MM, Apata IW, Meng L, Bell JM, McDonald E, Edwards JR, Kabbani S, Novosad S. Trends in intravenous antimicrobial start rates in outpatient hemodialysis centers, United States, 2012-2021. Antimicrob Steward Healthc Epidemiol. 2025 Mar 26;5(1):e87. doi: 10.1017/ash.2025.37. PMID: 40160227; PMCID: PMC11951228.
- Vazquez Deida AA, Kim C, Gouin KA, Zhang K, Mikosz CA, Neuhauser MM, Kabbani S. Assessment of high-volume antibiotic and opioid prescribing by Medicare Part D prescribers—United States, 2021. Public Health Rep. 2025 Nov 24. doi: 10.1177/00333549251384449.
- Schwarze TC, Gouin KA, Neuhauser MM, Hicks LA, Kabbani S. Antibiotic and Antiviral Prescribing for Long-Term Care Residents With a COVID-19 Diagnosis, March 2020-July 2023. J Am Geriatr Soc. 2025 Sep 2. doi: 10.1111/jgs.70022.