Overview
Gay and bisexual men account for about two-thirds (66%) of new HIV infections each year. Black/African American and Hispanic/Latino gay and bisexual men** are among the most affected. From 2010 to 2019, new HIV infections declined among White gay and bisexual men but remained higher and relatively stable among Black/African American and Hispanic/Latino gay and bisexual men. Social and structural barriers such as systemic racism, stigma, discrimination, homophobia, poverty, and homelessness can make it difficult to access HIV testing, care, and prevention services.
There have been significant advances in HIV prevention and treatment but missed testing opportunities in healthcare settings are preventing some gay and bisexual men from knowing their HIV status and benefitting from these advances. More HIV testing is needed to prevent new HIV infections and improve the health outcomes of gay and bisexual men with HIV.
- Gay and bisexual men who test negative can benefit from pre-exposure prophylaxis (PrEP). PrEP is highly effective in preventing HIV when taken as prescribed.
- Gay and bisexual men who learn they have HIV can start and stay on HIV treatment, get the virus down to an undetectable level (become virally suppressed), live long and healthy lives, and prevent sexual transmission to others.
The government’s Ending the HIV Epidemic in the U.S. initiative (EHE) aims to reduce new HIV infections in the United States by 75% by 2025 and by 90% by 2030. This goal can only be achieved by dramatically reducing new HIV infections among the most affected groups, including Black/African American and Hispanic/Latino gay and bisexual men, and expanding and sustaining investments in HIV services.
Overview
Gay and bisexual men account for about two-thirds (66%) of new HIV infections each year. Black/African American and Hispanic/Latino gay and bisexual men** are among the most affected. From 2010 to 2019, new HIV infections declined among White gay and bisexual men but remained higher and relatively stable among Black/African American and Hispanic/Latino gay and bisexual men. Social and structural barriers such as systemic racism, stigma, discrimination, homophobia, poverty, and homelessness can make it difficult to access HIV testing, care, and prevention services.
There have been significant advances in HIV prevention and treatment but missed testing opportunities in healthcare settings are preventing some gay and bisexual men from knowing their HIV status and benefitting from these advances. More HIV testing is needed to prevent new HIV infections and improve the health outcomes of gay and bisexual men with HIV.
- Gay and bisexual men who test negative can benefit from pre-exposure prophylaxis (PrEP). PrEP is highly effective in preventing HIV when taken as prescribed.
- Gay and bisexual men who learn they have HIV can start and stay on HIV treatment, get the virus down to an undetectable level (become virally suppressed), live long and healthy lives, and prevent sexual transmission to others.
The government’s Ending the HIV Epidemic in the U.S. initiative (EHE) aims to reduce new HIV infections in the United States by 75% by 2025 and by 90% by 2030. This goal can only be achieved by dramatically reducing new HIV infections among the most affected groups, including Black/African American and Hispanic/Latino gay and bisexual men, and expanding and sustaining investments in HIV services.
There are ongoing racial/ethnic differences in knowledge of status and HIV prevention and treatment outcomes among gay and bisexual men.
- About 20% of Hispanic/Latino, 17% of Black/African American, and 10% of White gay and bisexual men are unaware of their HIV status.
- Among gay and bisexual men who could benefit from PrEP, only 27% of Black/African American, 31% of Hispanic/Latino, and 42% of White gay and bisexual men reported using PrEP in 2017.
- Around 38% of Black/African American, 33% of Hispanic/Latino, and 26% of White gay and bisexual men with HIV are not virally suppressed.‡
- Black/African American and Hispanic/Latino gay and bisexual men experience higher levels of HIV stigma, with scores more than twice the national goal.††
New HIV Infections Among Gay and Bisexual Men Over Time
New HIV infections decreased among White gay and bisexual men but did not decrease among Black/African American and Hispanic/Latino gay and bisexual men.
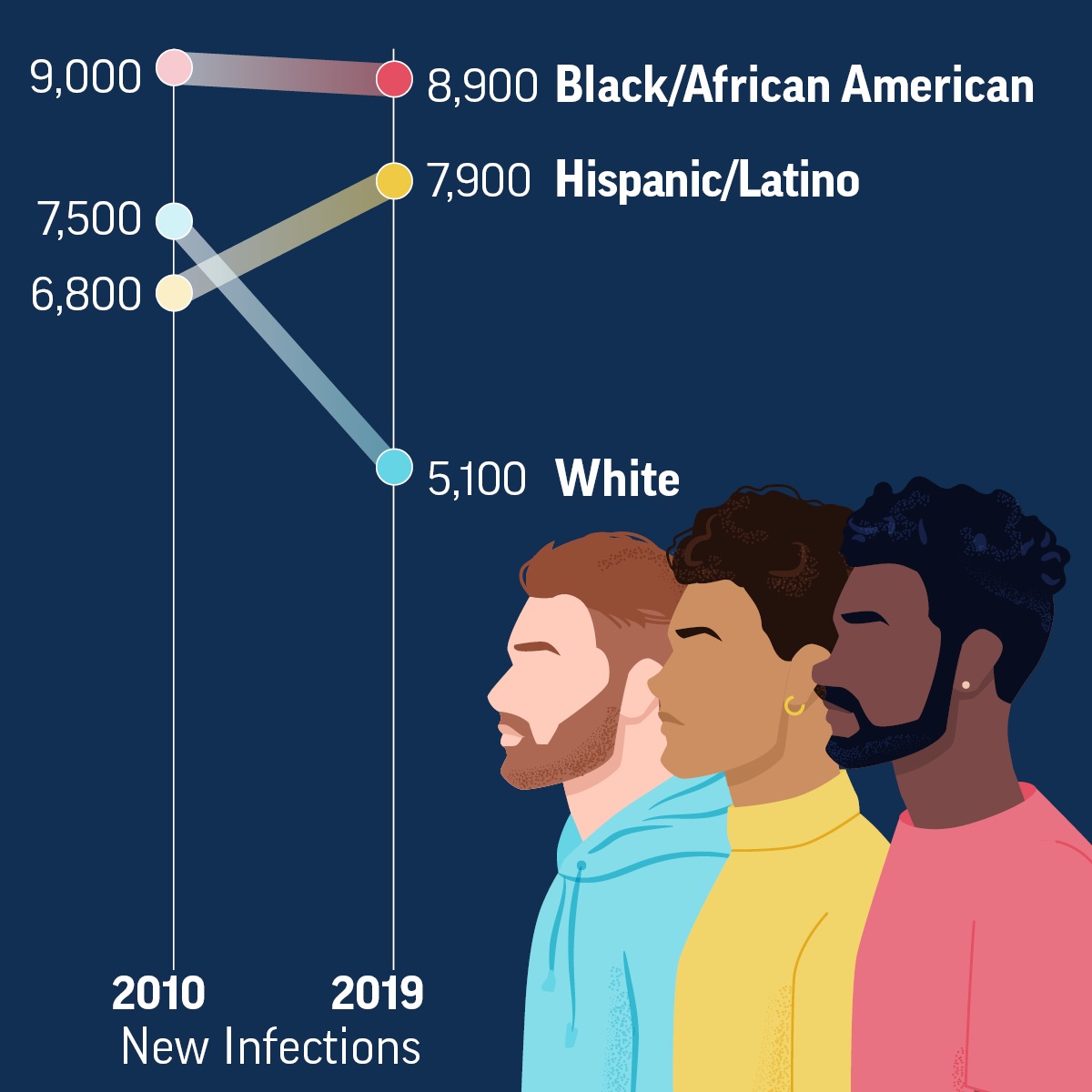
New HIV Infections Among Gay and Bisexual Men Over Time
Slope graph showing that from 2010–2019, new HIV infections decreased among White gay and bisexual men, but did not decrease among Black/African American and Hispanic/Latino gay and bisexual men.
New infections:
2010 – 9,000 Black/African American
2019 – 8,900 Black/African American
2010 – 6,800 Hispanic/Latino
2019 – 7,900 Hispanic/Latino
2010 – 7,500 White
2019 – 5,100 White
Higher Levels of Stigma Affect All Aspects of HIV
High levels of HIV stigma—negative attitudes and beliefs about people with HIV—make gay and bisexual men less likely to get tested, use prevention services like PrEP, receive care, and be virally suppressed.

Higher Levels of Stigma Affect All Aspects of HIV

HIV testing
Medications to prevent & treat HIV
Safer sex
Treatment & care
HIV Stigma
• Misinformation
• Homophobia
• Negative Attitudes
• Judgment
• Discrimination
• Racism
Differences Among Gay and Bisexual Men
Differences in knowledge of HIV status, PrEP usage, treatment adherence, and viral suppression for those with HIV continue to exist among gay and bisexual men.
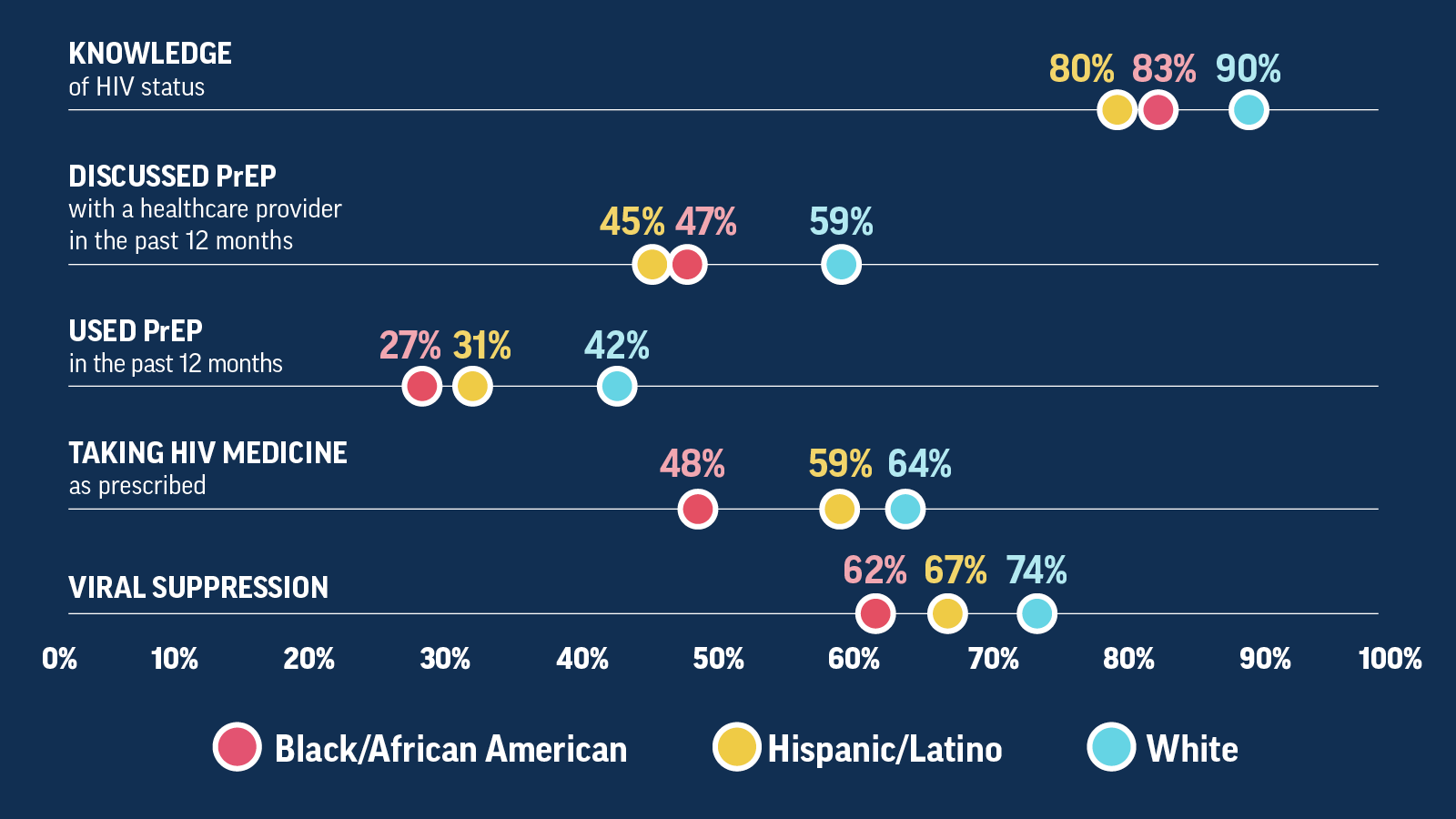
Differences Among Gay and Bisexual Men
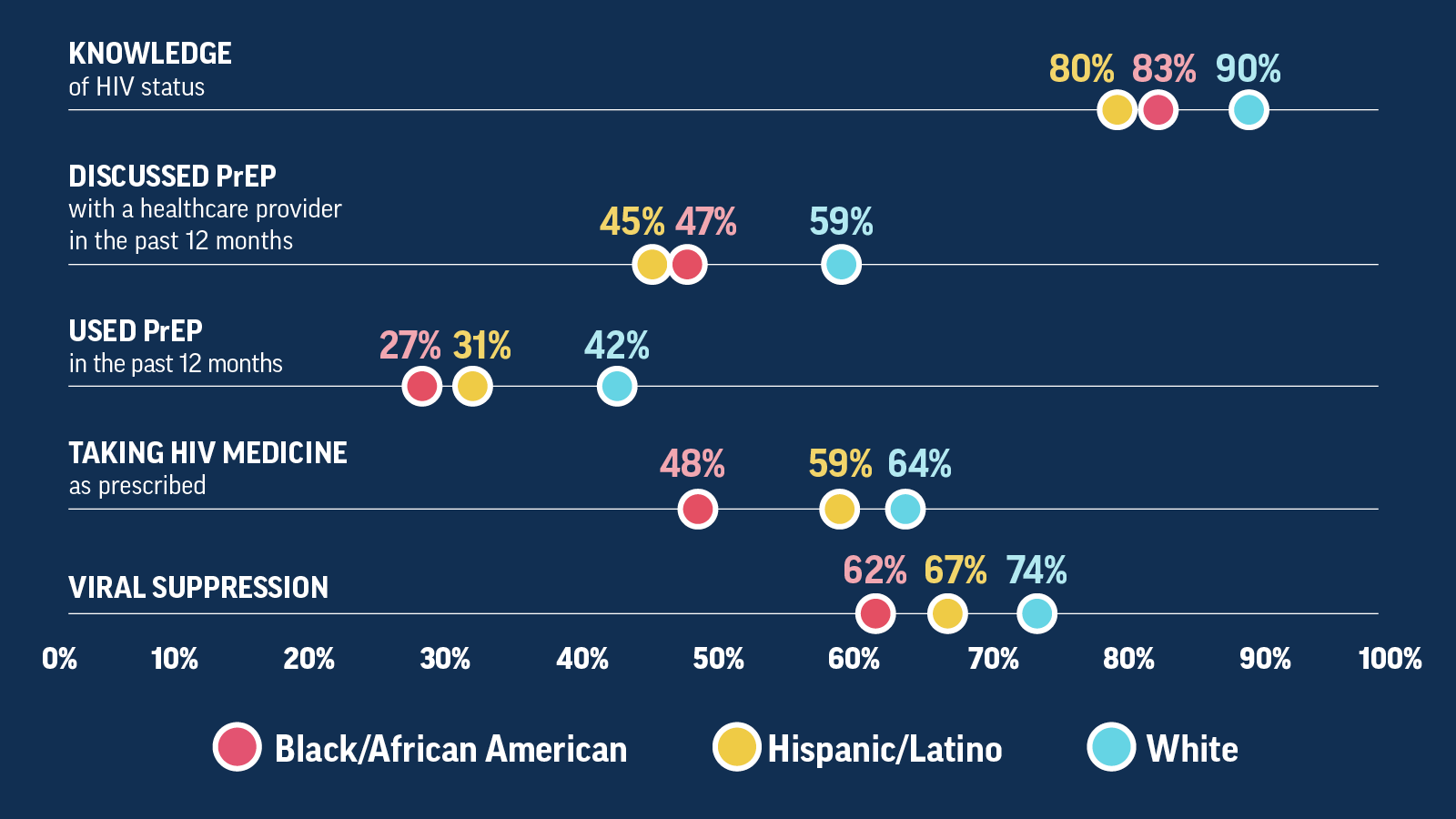
Table showing the percentages of White, Black/African American, and Hispanic/Latino gay and bisexual men who knew their HIV status, discussed PreP with a healthcare provider in the past 12 months, used PrEP in the past 12 months, took HIV medicine as prescribed, and were virally suppressed.
KNOWLEDGE of HIV status
Hispanic Latino – 80%
Black/African American – 83%
White – 90%
DISCUSSED PrEP with a healthcare provider in the past 12 months
Hispanic/Latino – 45%
Black/African American – 47%
White – 59%
USED PrEP in the past 12 months
Hispanic/Latino – 31%
Black/African American – 27%
White – 42%
TAKING HIV MEDICINE as prescribed
Hispanic/Latino – 48%
Black/African American – 59%
White – 64%
VIRAL SUPPRESSION
Hispanic/Latino – 62%
Black/African American – 67%
White – 74%
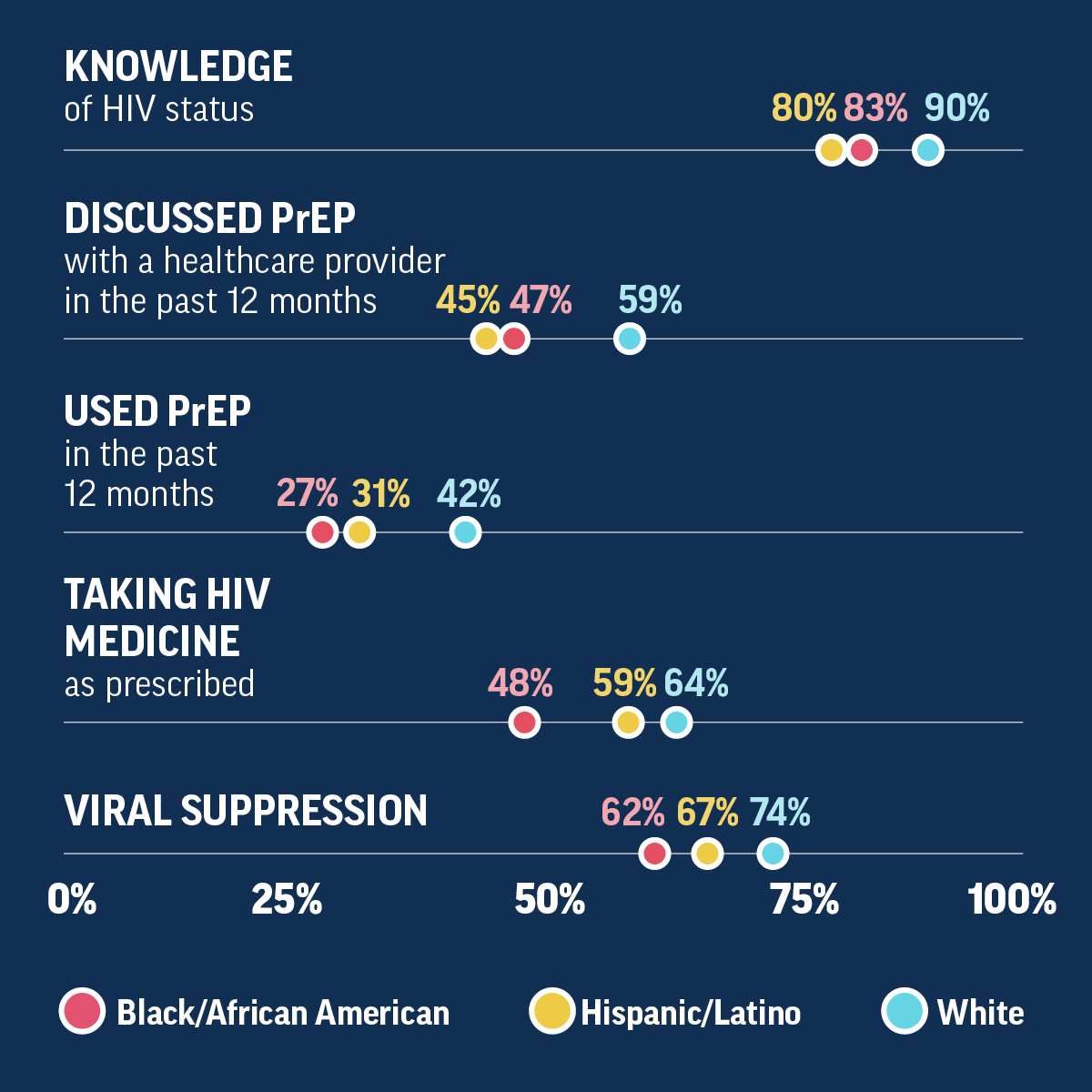
Differences Among Gay and Bisexual Men
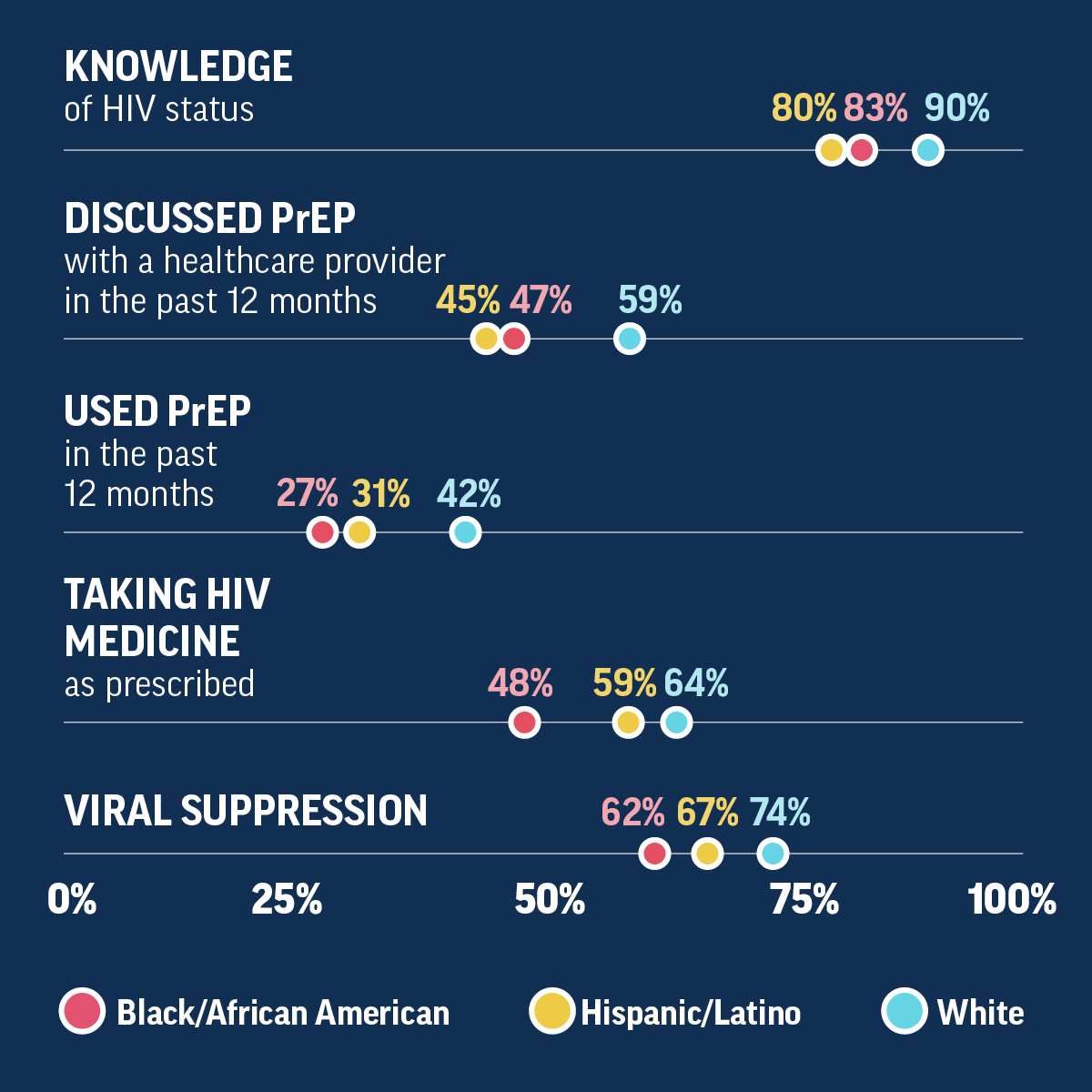
Table showing the percentages of White, Black/African American, and Hispanic/Latino gay and bisexual men who knew their HIV status, discussed PreP with a healthcare provider in the past 12 months, used PrEP in the past 12 months, took HIV medicine as prescribed, and were virally suppressed.
KNOWLEDGE of HIV status
Hispanic Latino – 80%
Black/African American – 83%
White – 90%
DISCUSSED PrEP with a healthcare provider in the past 12 months
Hispanic/Latino – 45%
Black/African American – 47%
White – 59%
USED PrEP in the past 12 months
Hispanic/Latino – 31%
Black/African American – 27%
White – 42%
TAKING HIV MEDICINE as prescribed
Hispanic/Latino – 48%
Black/African American – 59%
White – 64%
VIRAL SUPPRESSION
Hispanic/Latino – 62%
Black/African American – 67%
White – 74%
Innovative and culturally responsive strategies that address gay and bisexual men’s needs can reduce barriers that keep men from knowing their HIV status and receiving HIV prevention and treatment services. HIV service providers should consider:
- Implementing programs to give HIV self-testing kits to gay and bisexual men who may not have access to in-person testing services.
- Adapting Ryan White Program service models to other settings where comprehensive care and other support services are provided to gay and bisexual men with HIV. This includes enhanced collaboration with local partners and increased community engagement, effective data collection, and provider training.
- Making PrEP more available, especially for Black/African American and Hispanic/Latino gay and bisexual men, so that everyone who may benefit from it can get it.
- Engaging gay and bisexual men in HIV care (a status-neutral approach) to reduce stigma and racial barriers and help men receive HIV services regardless of their status.‡‡
- Addressing the root causes that drive inequality, including systemic racism, stigma, discrimination, homophobia, poverty, homelessness, and unequal access to care and prevention services.
Addressing HIV service inequities by race, sexual orientation, and socioeconomic status and tailoring strategies to meet the needs of local communities and reach the most affected groups, especially Black/African American and Hispanic/Latino gay and bisexual men, can help end the HIV epidemic.
Source: CDC Vital Signs, November 2021

Innovative and culturally responsive strategies that address gay and bisexual men’s needs can reduce barriers that keep men from knowing their HIV status and receiving HIV prevention and treatment services. HIV service providers should consider:
- Implementing programs to give HIV self-testing kits to gay and bisexual men who may not have access to in-person testing services.
- Adapting Ryan White Program service models to other settings where comprehensive care and other support services are provided to gay and bisexual men with HIV. This includes enhanced collaboration with local partners and increased community engagement, effective data collection, and provider training.
- Making PrEP more available, especially for Black/African American and Hispanic/Latino gay and bisexual men, so that everyone who may benefit from it can get it.
- Engaging gay and bisexual men in HIV care (a status-neutral approach) to reduce stigma and racial barriers and help men receive HIV services regardless of their status.‡‡
- Addressing the root causes that drive inequality, including systemic racism, stigma, discrimination, homophobia, poverty, homelessness, and unequal access to care and prevention services.
Addressing HIV service inequities by race, sexual orientation, and socioeconomic status and tailoring strategies to meet the needs of local communities and reach the most affected groups, especially Black/African American and Hispanic/Latino gay and bisexual men, can help end the HIV epidemic.
Source: CDC Vital Signs, November 2021

Increase HIV testing:
- Reduce barriers and missed opportunities to test gay and bisexual men in a variety of settings.
- Test sexually active gay and bisexual men at least once a year.
- Some gay and bisexual men may benefit from more frequent testing (every 3 to 6 months).
- Expand the use of HIV self-tests for gay and bisexual men.
Prevent new HIV infections:
- Talk to all gay and bisexual men about the benefits of using PrEP to prevent HIV.
- Prescribe PrEP to those who could benefit from it.
- Discuss other prevention options like condoms and the right way to use them.
- Ensure PrEP providers are in communities most affected by HIV.
- Use telehealth to expand access to HIV prevention.
Treat HIV quickly and effectively:
- Link gay and bisexual men diagnosed with HIV immediately to care and treatment.
- Find those who fall out of HIV care and link them back to care as soon as possible.
- Help gay and bisexual men with HIV stay in care and take their medicine as prescribed.Talk to those with HIV about any problems they have taking HIV medicine.
Everyone can:
- Get tested for HIV. Find an HIV test, including an HIV self-test.
- Talk to their healthcare provider about HIV prevention options, including PrEP.
- Get into care and take medicine to treat HIV if needed.
- Help end HIV stigma.
Increase HIV testing:
- Reduce barriers and missed opportunities to test gay and bisexual men in a variety of settings.
- Test sexually active gay and bisexual men at least once a year.
- Some gay and bisexual men may benefit from more frequent testing (every 3 to 6 months).
- Expand the use of HIV self-tests for gay and bisexual men.
Prevent new HIV infections:
- Talk to all gay and bisexual men about the benefits of using PrEP to prevent HIV.
- Prescribe PrEP to those who could benefit from it.
- Discuss other prevention options like condoms and the right way to use them.
- Ensure PrEP providers are in communities most affected by HIV.
- Use telehealth to expand access to HIV prevention.
Treat HIV quickly and effectively:
- Link gay and bisexual men diagnosed with HIV immediately to care and treatment.
- Find those who fall out of HIV care and link them back to care as soon as possible.
- Help gay and bisexual men with HIV stay in care and take their medicine as prescribed.Talk to those with HIV about any problems they have taking HIV medicine.
Everyone can:
- Get tested for HIV. Find an HIV test, including an HIV self-test.
- Talk to their healthcare provider about HIV prevention options, including PrEP.
- Get into care and take medicine to treat HIV if needed.
- Help end HIV stigma.
Footnotes
*This web page uses the term gay and bisexual men to represent gay, bisexual, and other men who reported male-to-male sexual contact.
†Includes infections attributed to male-to-male sexual contact only.
‡Being virally suppressed means having a very low amount of HIV in the blood (less than 200 copies of HIV per milliliter of blood). People who remain virally suppressed (or get and keep an undetectable viral load) have effectively no risk of transmitting HIV to their sex partners.
**Hispanic/Latino gay and bisexual men can be of any race.
††The National Strategic Plan goal is to decrease stigma among people with diagnosed HIV by 50% by 2025, from a 2018 baseline median score of 31.2 on a 10-item questionnaire.
‡‡A status-neutral approach integrates health services so that HIV prevention and treatment are part of comprehensive primary care.
Related Pages and Resources
- Vital Signs: Media Statement – Nuevo informe de Signos Vitales de los CDC revela una década de inequidades continuas respecto del VIH en la víspera del Día Mundial del Sida [Spanish]
- Morbidity and Mortality Weekly Report (MMWR): Vital Signs: HIV Infection, Diagnosis, Treatment, and Prevention Among Gay, Bisexual, and Other Men Who Have Sex with Men—United States, 2010–2019
- CDC: HIV and Gay and Bisexual Men
- CDC: HIV Basics
- CDC HIV Nexus: Resources for Clinicians
- CDC: HIV Risk Reduction Tool
- CDC: Let’s Stop HIV Together
- CDC: Get Tested
- CDC National Prevention Information Network (NPIN)
Other Sites
Get email updates about Vital Signs
VITAL SIGNS RESOURCES