Key points
- Tuberculosis (TB) screening programs for health care personnel are part of TB infection control plans.
- CDC recommends all U.S. health care personnel should be screened for TB upon hire.
- Annual TB testing is not recommended unless there is a known exposure or ongoing transmission.
- State and local TB regulations may differ.

TB screening programs in health care settings
TB screening programs should include anyone working or volunteering in health care settings, including:
- Inpatient settings
- Outpatient settings
- Laboratories
- Emergency medical services
- Medical settings in correctional facilities
- Home-based health care and outreach settings
- Long-term care facilities
- Clinics in homeless shelters
Determining an approach
Follow your state's TB regulations.
Contact your state TB control program for the testing regulations in your state.
Screening guidelines
Resource
CDC and the National TB Coalition of America released updated recommendations for TB screening, testing, and treatment of health care personnel on May 17, 2019.
These recommendations update the health care personnel screening and testing section of the 2005 CDC Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Settings.
All U.S. health care personnel should be screened for TB upon hire (i.e., preplacement).
TB screening includes:
- A baseline individual TB risk assessment,
- TB symptom evaluation
- A TB test (e.g., TB blood test or a TB skin test), and
- Additional evaluation for TB disease as needed.
Annual TB testing of health care personnel is not recommended unless there is a known exposure or ongoing transmission at a health care facility.
U.S. health care personnel without latent TB infection should not undergo routine serial TB screening or testing at any interval after baseline (e.g., annually). Health care personnel should have a timely symptom evaluation and additional testing, if indicated, after known exposure to a person with potentially infectious TB disease, or ongoing transmission at a facility.
Treatment for latent TB infection is highly recommended.
Short course, rifamycin-based regimens are the preferred treatment options for latent TB infection because they have higher completion rates.
If health care personnel diagnosed with latent TB infection do not receive treatment:
- Perform annual screening for symptoms of TB disease.
- Annually reevaluate the risk and benefits of treatment for latent TB infection
- Ensure health care personnel know the symptoms of TB disease that should prompt an immediate evaluation between screening
All health care personnel should receive annual TB education.
TB education should include:
- Information on TB risk factors,
- Signs and symptoms of TB disease, and
- TB infection control policies and procedures.
When to report cases
Notify the health department immediately if TB disease is presumed or confirmed.
Resources
Health Care Personnel Baseline Individual Tuberculosis Risk Assessment
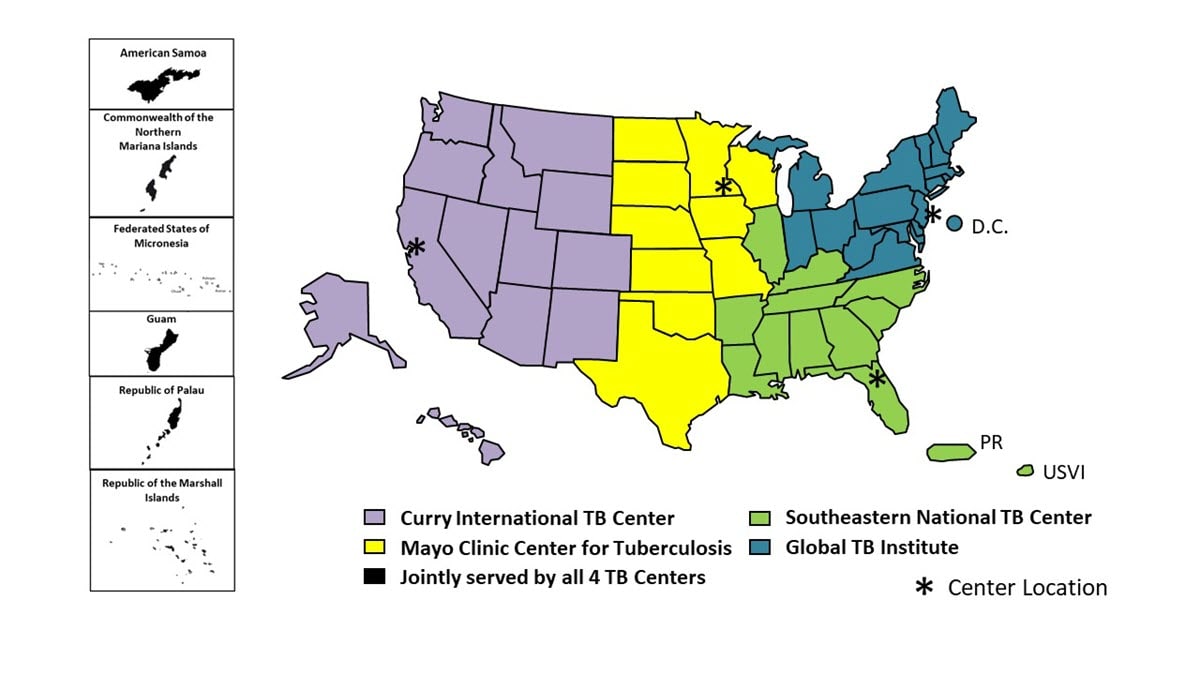
Tuberculosis Centers of Excellence for Training, Education, and Medical Consultation
- Sosa LE, Njie GJ, Lobato MN, et al. Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations from the National Tuberculosis Controllers Association and CDC, 2019. MMWR Morb Mortal Wkly Rep 2019;68:439–443. DOI: http://dx.doi.org/10.15585/mmwr.mm6819a3
- Jensen PA, Lambert LA, Iademarco MF, Ridzon R. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep 2005;54(No. RR-17). https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.htm