What to know
All U.S. health care personnel should be screened for tuberculosis (TB) upon hire (i.e., preplacement). This process includes a risk assessment, symptom evaluation, and TB blood test or TB skin test.
TB Screening and Testing for Health Care Personnel
The TB screening process for health care personnel includes:
- A baseline individual TB risk assessment,
- TB symptom evaluation
- A TB test (e.g., TB blood test or a TB skin test), and
- Additional evaluation for TB disease as needed.
Follow your state's TB regulations.
CDC recommendations do not override or replace state regulations. State and local regulations may differ to meet local needs.
Contact your state or local TB control program for the testing regulations in your state.
Health Care Personnel Baseline Individual TB Risk Assessment
Health care personnel should be considered at increased risk for TB if any of the following risk factors are present:
- Exposure to TB disease,
- Time spent in countries where TB is common (e.g., born in or frequent travel to countries with a high rate of TB), and
- Current or planned immune system suppression (e.g., HIV infection or taking medication that suppresses the immune system).
Use an individual TB risk assessment to help interpret test results and determine whether health care personnel are at increased risk. Health care personnel at lower risk for TB who have a positive test result for TB infection should have a second TB test (either a TB blood test or TB skin test).
- For example, health care personnel who do not have any TB symptoms, are unlikely to be infected (based on risk factors for exposure) and are at low risk for progression to TB disease should receive a second TB test if their first test result is positive.
- Health care personnel are considered to have TB infection only if both the first and second test results are positive and should then be evaluated with a chest x-ray and TB symptom screening.
TB Symptom Evaluation
Symptoms of active TB disease include:
- A cough that lasts three weeks or longer
- Chest pain
- Coughing up blood or sputum (phlegm from deep inside the lungs)
- Weakness or fatigue
- Weight loss
- Loss of appetite
- Chills
- Fever
- Night sweats
Baseline TB Blood Test for Health Care Personnel
If baseline testing is performed using a TB blood test (also known as Interferon Gamma Release Assay or IGRA):
- Administer TB blood test following proper protocol.
- Review result, using the individual TB risk assessment to help interpret test results.
- If the result is negative, consider not infected.
- If the result is positive and the health care personnel is at low risk, administer a second test.
- If the result of the second test is also positive (for health care personnel at low risk) or the health care personnel is at risk, consider the health care personnel to be infected with TB and evaluate for TB disease.
- If the result is negative, consider not infected.
- Document result.
Using a TB blood test for baseline testing of health care personnel does not require two-step testing.
TB blood tests are the preferred TB test for people who have received the Bacille Calmette-Guérin (BCG) vaccine.
Baseline Two-Step TB Skin Test for Health Care Personnel
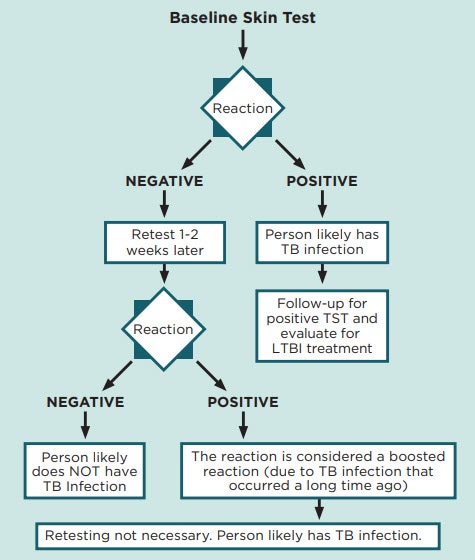
If the Mantoux tuberculin skin test (TST) is used for baseline testing of health care personnel, use two-step testing.
Purpose
Two-step testing is recommended for the initial TB skin test for adults who may be tested periodically, such as health care personnel. This procedure is especially important for settings that are classified as low risk where testing is indicated only upon exposure.
Some people with latent TB infection have a negative reaction to the TB skin test when tested years after being infected. However, if they are tested again within a year of the first test, they may have a positive reaction. The first TB skin test can "trigger the memory" of the immune system, boosting its ability to react to the second TB skin test.
It may appear that these people were infected between the first and second tests. However, the second positive test reaction is actually a boosted reaction due to TB infection that occurred a long time ago.
Two-step TB skin test process
The TB skin test should be placed and read by a designated, trained health care provider. Consult with your state and local public health authorities to determine who is authorized to place and read TB skin tests in your state.
Step 1
- Administer first TB skin test following proper protocol.
- Review result, using the individual TB risk assessment to help interpret test results.
- If the result is negative, a second TB skin test is needed (see step 2). Retest the health care personnel 1 to 3 weeks after the first TB skin test result is read.
- If the result is positive and the health care personnel is at low risk, administer a second test.
- If the result of the second test is also positive (for health care personnel at low risk) or the health care personnel is at risk, consider the health care personnel to be infected with TB and evaluate for TB disease.
- If the result is negative, a second TB skin test is needed (see step 2). Retest the health care personnel 1 to 3 weeks after the first TB skin test result is read.
- Document result.
Step 2
- Administer second TB skin test 1 to 3 weeks after the first TB skin test result is read following proper protocol.
- Review results. If positive, consider the health care personnel to be infected with TB and evaluate for TB disease. Use the individual TB risk assessment to help interpret test results. If negative, consider not infected.
- Document result.
If the second test result of a two-step TB skin test is not read within 48–72 hours:
- Administer a TB skin test as soon as possible (even if several months have elapsed). Read the result within 48–72 hours.
- If a person fails to return within 72 hours and has a negative test result, repeat the TB skin test. TB skin tests can be repeated at any time. In general, there's no health risk associated with repeated TB skin tests.
A second TB skin test is not needed if the person has a documented TB skin test result from any time during the previous 12 months.
- If a person has had a documented negative TB skin test result within the previous 12 months, a single TB skin test can be administered.
- This additional TB skin test represents the second stage of two-step testing.
Screening Health Care Personnel with a Prior Positive TB Test Result
Health care personnel with a documented history of a prior positive TB test result should receive an individual TB risk assessment and TB symptom screen upon hire (i.e., pre-placement). Repeating the TB test (e.g., TB blood test or TB skin test) is not required.
In most cases, repeat chest x-rays are not required
Health care personnel with a prior positive TB test should also receive a chest x-ray or provide documentation of a normal chest x-ray. Repeat chest x-rays are not required unless health care personnel develop signs or symptoms of TB disease or as part of the repeat evaluation prior to starting treatment for latent TB infection.
Local or state regulations may determine the requirements regarding acceptable documentation. Contact your state TB program for the regulations in your state.
Conduct an annual TB symptom screen
Health care personnel with untreated latent TB infection should receive a yearly TB symptom screen to detect early evidence of TB disease and to reevaluate the risks and benefits of treatment for latent TB infection.
Encourage treatment for latent TB infection
Treatment is strongly encouraged for health care personnel diagnosed with latent TB infection. Short course, rifamycin-based regimens are the preferred treatment options for latent TB infection because they have higher completion rates.
- Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations from the National Tuberculosis Controllers Association and CDC, 2019 | MMWR
- Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Settings, 2005 (cdc.gov)
- Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children | Clinical Infectious Diseases | Oxford Academic (oup.com)
