At a glance
A suicide cluster may be defined as a group of suicides, suicide attempts, or self-harm events that occur closer together in time and space than would normally be expected in a given community. This page describes how to report a suicide cluster or get assistance.
What is a suicide cluster?
Definition
When a group of suicides or suicide attempts occur closer together in time, space, or both than would normally be expected in a community, the deaths are defined as a suicide cluster.
The two most commonly reported types of suicide clusters are:
- Point clusters (or spatial-temporal clusters) represent a greater-than-expected number of suicides or suicide attempts that occur within a time period in a specific location. Point clusters might occur in a community/county or an institution such as a school, university, or psychiatric inpatient setting.
- Mass clusters (or temporal clusters) represent a greater-than-expected number of suicides or suicide attempts spread out geographically within a time period.
Who is at risk?
People and place
Published investigations of suicide clusters show that there is no one place that clusters are more likely to occur. They occur in a variety of locations and settings, such as:
- American Indian and Alaska Native communities
- People experiencing incarceration
- People in psychiatric inpatient facilities
- Teenagers and young adults
- Hospitals
- Military institutions
- Schools
Other risk factors
Other risk factors for individuals involved in suicide clusters are thought to be similar to general risk factors for suicide. They may include:
- Being male
- A history of substance use, self-harm, or mental illness
Suicide as a contagion
Suicide clusters, especially mass clusters, might occur through a process of contagion. Suicide contagion occurs when the exposure to suicide or suicidal behavior of one or more people influences others to attempt suicide.
Exposure can be direct by having a personal connection to the person who died by suicide, or indirect through media reporting or social media posts about a person who was not a personal connection.
Influence of media
Media influence can be both a risk and protective factor depending on how long the coverage lasts, how prominent the source is, what is being shared, and the language being used. This could include social media, news reports, and entertainment media.
Media as a protective factor
Media can play an important role in preventing suicide risk or deaths by following Best Practices and Recommendations for Reporting on Suicide. For example, media can:
- Use appropriate language such as "died by suicide" instead of "committed suicide"
- Report suicide as a public health problem and provide resources such as 988 Suicide & Crisis Lifeline and treatment options
- Provide information on warning signs of suicide risk
- Engage suicide prevention or mental health experts to share facts about suicide and how to prevent it
- Emphasize messages of help and hope
- Educate the public about coping strategies and treatment
Media as a risk factor
Media reporting of suicides might be a risk factor when it unintentionally influences increases in suicides, particularly when media reports do not follow best practices and include things like:
- Dramatic or graphic headlines or images
- Explicitly describing the suicide method or showing pictures of it
- A statement that suicide is inevitable
- Repeatedly reporting on the same suicide, including high-profile celebrities who may be considered models for imitation
- Showing the site of the suicide and pictures of those who are grieving
How to report a suspected suicide-related cluster
Contact your local or state health department if you suspect a suicide-related cluster in your community or if you would like information such as suicide statistics or trends in your area. You can also find suicide data for your state or local area using CDC WISQARS or CDC WONDER.
Note: When you report a suspected suicide-related cluster the local or state health department will gather information from you, develop a case definition, and determine whether there is a greater-than-expected number of cases to meet the criteria for a suicide cluster.
How to assess and investigate a suicide cluster
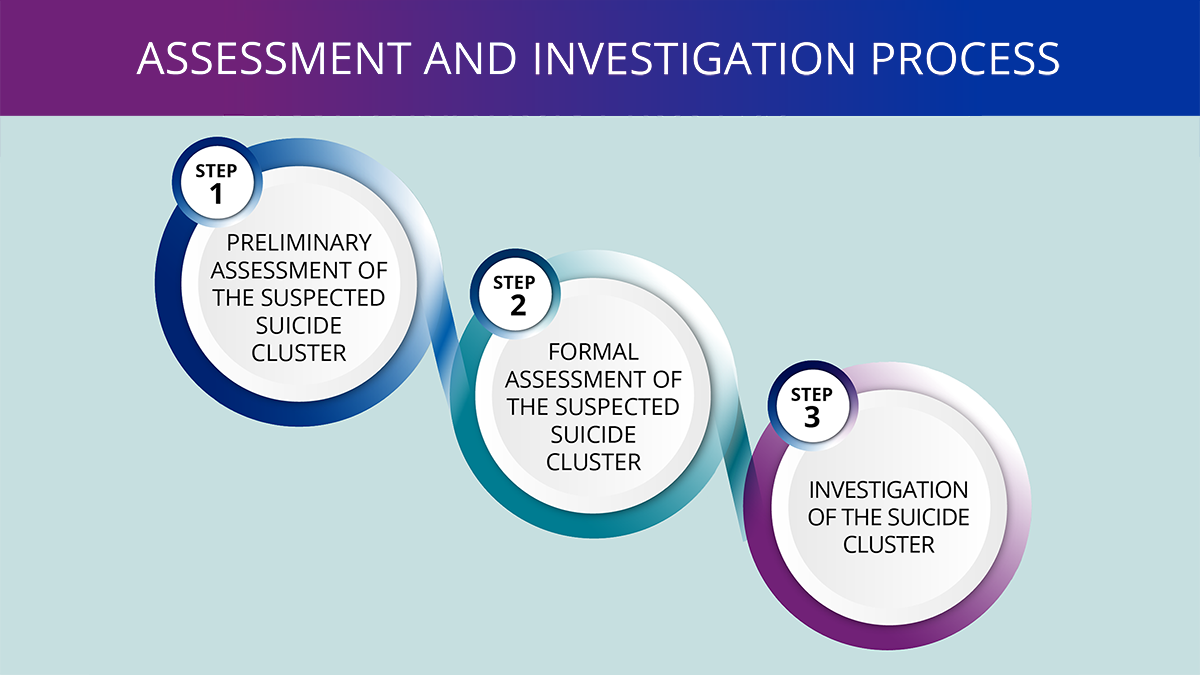
Monitoring suicide-related events is a key component of prevention and might reveal when an unusual pattern, or a cluster, of suicides or suicide attempts have occurred.
The following steps from the CDC Guidance for Community Assessment and Investigation of Suspected Suicide Clusters — United States, 2024 Morbidity and Mortality Weekly Report (MMWR) help communities to assess and investigate suspected suicide clusters to ultimately inform public health action to prevent further suicides.
Step 1: Conduct a preliminary assessment of the information obtained to determine whether a formal assessment is warranted. This step includes the following tasks:
- Collect details about the suspected cluster
- Convene or form a suicide cluster coordinating committee
- Determine whether to conduct a formal assessment of the suspected cluster
Step 2: Conduct a formal assessment of the suspected cluster to determine if it meets the definition of a cluster. This step includes the following tasks:
- Develop a case definition
- Determine the time frame
- Identifying data sources
- Select and carry out analytic methods*
- Determine whether to conduct further investigation
* Remember, it may be difficult to prove that a cluster occurred because of small numbers. There are statistical methods available that can be applied, such as geographic information systems, Knox, Poisson, or Scan tests.
Step 3: Conduct an investigation to identify commonalities or similarities in cases that can inform a community response. This step includes the following tasks:
- Develop and implement an investigation plan
- Report findings to inform public health action
Sometimes, initiating a community response simultaneously during any of the steps might be warranted. View the How to Respond to a Suicide Cluster section to learn more about community response planning.
Read the MMWR to learn more about how to assess and investigate a suicide cluster.
How to respond to a suicide cluster
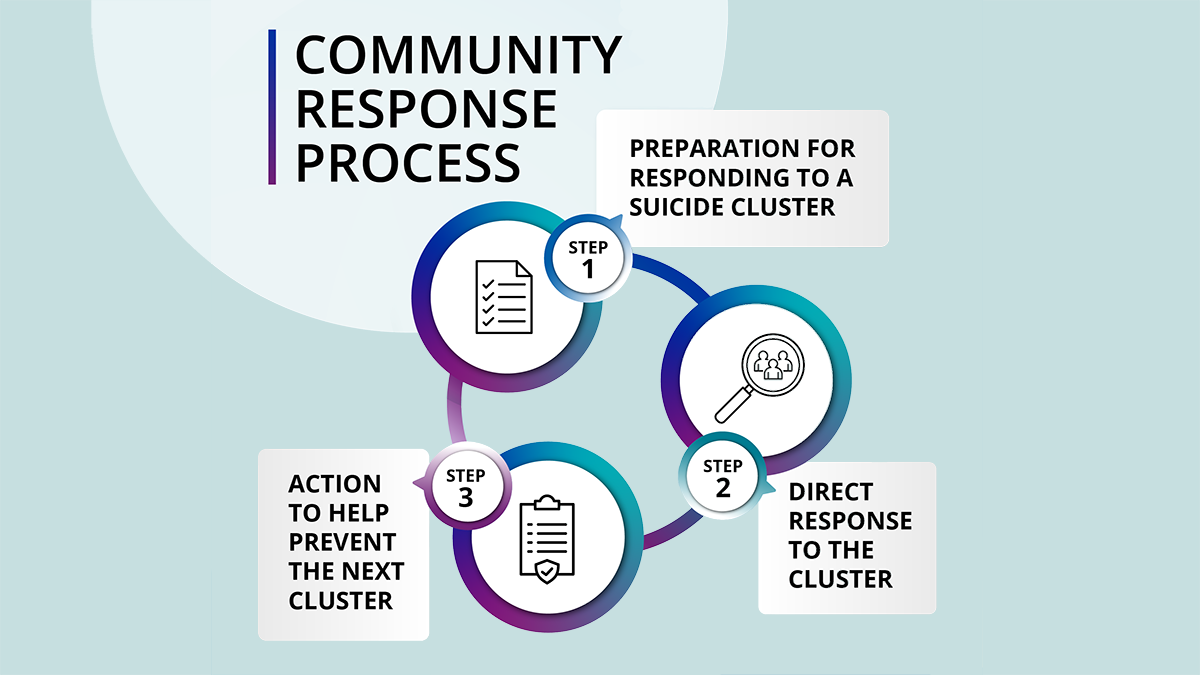
The overall goal of a community response plan is to contain the cluster and prevent additional deaths and attempts. A community response plan should consider identifying and referring persons who may be at high risk of suicide, regardless of whether the community-identified cluster involves a statistically significant greater-than-expected number of cases.
The following steps from the CDC Guidance for Community Response to Suicide Clusters — United States, 2024 Morbidity and Mortality Weekly Report (MMWR) help local public health and community leaders develop a response plan for suicide clusters or clusters of suicide attempts based on resources, cultural context, and health equity needs of the community.
Step 1: Prepare to respond to a suicide cluster. This step includes the following tasks:
- Review guidance and develop a community-specific response plan
- Engage partners in a suicide cluster coordinating committee
- Identify relevant community resources
- Determine the conditions under which a response plan should be implemented
Step 2: Direct response to the suicide cluster. This step includes the following tasks:
- Notify and prepare the identified groups
- Identify, screen, and refer those at high risk
- Avoid glorifying suicide decedents and minimize sensationalism
- Provide a timely flow of accurate, appropriate information to the media
- Consider the relevance and respond to the impact of social media
Step 3: Act to help prevent the next suicide cluster. This step includes the following tasks:
- Identify and change elements in the environment that might increase the likelihood of further suicides or suicide attempts
- Address long-term issues suggested by the nature of this cluster
- Consider evaluating the response
Read the MMWR to learn more about how to respond to a suicide cluster.
Reference15
How to request CDC assistance
When a situation meets suicide cluster criteria you may want CDC assistance either through informal technical assistance or an Epi-Aid request.
Informal technical assistance consists of guidance or resources that CDC can provide to help you. An Epi-Aid is an onsite, rapid, short-term (1–3 weeks) investigation of an urgent public health problem, such as a suicide cluster, by Epidemic Intelligence Service (EIS) officers and other CDC subject matter experts. The Epi-Aid investigation helps you make rapid, practical decisions for actions to prevent and control the public health problem.
Use the following steps to request an Epi-Aid:
- The requesting official with authority for public health contacts the subject matter expert at CDC or the EIS program (EpiAid@cdc.gov) for an initial discussion of the technical assistance needed.
- The CDC subject matter expert and the EIS program discuss the Epi-Aid request and determine if CDC can support the Epi-Aid. Once CDC determines it can support the Epi-Aid, CDC notifies the requesting official.
- If CDC can support the Epi-Aid, the requesting official must send a written invitation by email to the CDC subject matter expert or to the EIS Program at EpiAid@cdc.gov.
Use the following steps to request informal technical assistance:
Email CDC's Division of Injury Prevention at injuryprevention@cdc.gov. Put "TA request for suspected suicide cluster" in the subject line.
Published Reports on Suicide Epi-Aids
- Increase in youth suicides — Stark County, Ohio, 2018 This report provides a cross-sectional view of the prevalence of suicidal behaviors, key risk and protective factors among youth, media coverage of suicide, and suicide prevention initiatives taking place in Stark County.
- Undetermined risk factors for suicide among youth, ages 10-24 — Santa Clara County, CA, 2016 This report investigates youth suicide clusters in Santa Clara County, exploring characteristics, trends, and factors related to fatal and nonfatal suicidal behavior, analyzing media reporting, evaluating local prevention efforts, and identifying prevention strategies across different levels.
- Undetermined risk factors for suicide among youth, ages 10-24 — Fairfax County, VA, 2014 This report examined trends of fatal and non-fatal suicidal behaviors among youth in Fairfax County to guide the prevention strategies of local health departments and community partners.
Additional information and resources
Access additional resources on suicide prevention.
MMWR supplement papers
- Ballesteros MF, Ivey-Stephenson AZ, Trinh E, Stone DM. Background and rationale — CDC guidance for communities assessing, investigating, and responding to suicide clusters, United States, 2024. MMWR: Supplement 2024; 73(2), 1-7.
- Trinh E, Ivey-Stephenson AZ, Ballesteros MF, Idaikkadar N, Wang J, Stone DM. CDC Guidance for community assessment and investigation of suspected suicide clusters — United States, 2024. MMWR: Supplement 2024; 73(2), 8-16.
- Ivey-Stephenson AZ, Ballesteros MF, Trinh E, Stone DM, Crosby A. CDC Guidance for community response to suicide clusters — United States, 2024. MMWR: Supplement 2024; 73(2), 17-26.
Other resources
- Best Practices and Recommendations for Reporting on Suicide
- CDC's Suicide Prevention Resource for Action
- Suicide Prevention | Suicide | CDC
- National Violent Death Reporting System (NVDRS): State Profiles and Program Contact Information
- Suicide Prevention Resource Center (SPRC): State Suicide Prevention Infrastructure Recommendations
Need help? Know someone who does?
Contact the 988 Suicide and Crisis Lifeline if you are experiencing mental health-related distress or are worried about a loved one who may need crisis support.
- Call or text 988
- Chat at 988lifeline.org
Connect with a trained crisis counselor. 988 is confidential, free, and available 24/7/365.
Visit the 988 Suicide and Crisis Lifeline for more information at 988lifeline.org.
- Ballesteros MF, Ivey-Stephenson AZ, Trinh E, Stone DM. Background and rationale — CDC guidance for communities assessing, investigating, and responding to suicide clusters, United States, 2024. MMWR: Supplement 2024; 73(2), 1-7.
- Gould MS, Wallenstein S, Kleinman M. Time-space clustering of teenage suicide. American Journal of Epidemiology 1990;131(1):71-8. https://doi.org/10.1093/oxfordjournals.aje.a115487 PMID:2293755
- Mueller AS, Abrutyn S. Adolescents under Pressure: A New Durkheimian Framework for Understanding Adolescent Suicide in a Cohesive Community. American Sociological Review. 2016; 81: 877-899.
- Masecar D. Suicide clusters: A discussion. Ottawa, ON: First Nations Inuit Health Branch, Health Canada, 2009.
- Haw C, Hawton K, Niedzwiedz C, Platt S. Suicide clusters: A review of risk factors and mechanisms. Suicide Life Threat Behav. 2013; 43(1): 97-108.
- O’Carroll P. Suicide prevention: Clusters and contagion. In: Berman AL, editor. Suicide Prevention: Case Consultations. New York: Springer, 1990.
- Cheng Q, Li H, Silenzio V, Caine ED. Suicide contagion: A systematic review of definitions and research utility. PLoS One. 2014; 9(9): e108724. doi: 1371/journal.pone.0108724.
- Gould M, Jamieson P, Romer D. Media contagion and suicide among the young. American Behavioral Scientist. 2003; 46(9): 1269-1284.
- Suicide Awareness and Voices of Education. Best Practices and Recommendations for Reporting on Suicide. 2020.
- Niederkrotenthaler T, Voracek M, Herberth A, Till B, Strauss M, Etzersdorfer E, & Sonnec, G. (2010). Role of media reports in completed and prevented suicide: Werther v. Papageno effects. The British Journal of Psychiatry. 2010; 197(3): 234-243.
- World Health Organization: Preventing Suicide: A resource for media professionals.
- Trinh E, Ivey-Stephenson AZ, Ballesteros MF, Idaikkadar N, Wang J, Stone DM. CDC Guidance for community assessment and investigation of suspected suicide clusters — United States, 2024. MMWR: Supplement 2024; 73(2), 8-16.
- Gibbons RD, Clark DC, Fawcett J. A statistical method for evaluating suicide clusters and implementing cluster surveillance. Am J Epidemiol. 1990; 132(1 Suppl): S183-91. doi: 1093/oxfordjournals.aje.a115781.
- O'Carroll PW, Mercy JA. Responding to community-identified suicide clusters: Statistical verification of the cluster is not the primary issue. Am J Epidemiol. 1990. pp. S196–202.
- Ivey-Stephenson AZ, Ballesteros MF, Trinh E, Stone DM, Crosby A. CDC Guidance for community response to suicide clusters — United States, 2024. MMWR: Supplement 2024; 73(2), 17-26.
- Gould MS, Wallenstein S, Kleinman MH, et al. Suicide clusters: An examination of age-specific effects. Am J Public Health. 1990; 80: 211-212.
- Niedzwiedz C, Haw C, Hawton K, Platt S. The definition and epidemiology of clusters of suicidal behavior: A systematic review. Suicide Life Threat Behav. 2014; 44(5): 569-81.
