At a glance
There are many important features to consider when creating an IPS program, including:
Considering an IPS program
There are several features that are important to consider when developing an IPS program, such as adapting patient interviews to include questions about online sex partners, creating profiles, developing email language, and understanding how to confidentially notify partners through the various mediums. These features will be described in this toolkit. See Appendix A for an example of an IPS program checklist.
4.1 Creating profiles, screen names, and email addresses
In order to access many of the online sites or mobile apps, programs may need to create a user or member profile. When creating a profile, it is suggested that an official health department email should be associated with the profile, the official health department logo should be used as the account picture when possible, and other identifying information should be provided respective to ISP/website protocol for health departments.
Several caveats exist:
- Some sites will not allow logos; rather the profile picture must be of a person.
- Some websites may require certain information to be contained within your profile.
- Some profile fields are required for membership but may not be applicable to the IPS program. These could include age, sexual preferences, etc. When this occurs, we suggest that programs choose the least complicated option. In some cases, programs have selected the lowest risk option or the option that most closely relates to the at-risk population. While not perfect, until such time that online venues create an option for public health memberships, those doing PS must work within the requirements of a regular member profile.
- Some online venues do not allow URLs or links to be used in open narrative fields, while others have provided fields for websites and social media accounts.
For examples of health department social media and dating app profiles, go to Appendix B.
4.2 Interviewing and elicitation
4.2.1 IPS-specific parts of the original interview
The CDC's Program Operation Guidelines state, "While interviewing the patient, the DIS should make every attempt to enlist the patient as a resource, making it clear that the information the patient provides will be confidential and very helpful to the DIS, the patient, and the patient's partners. The DIS can incorporate elements of patient-centered counseling by acknowledging and treating the patient as a partner in reducing additional STDs in their community. The partnership should be clear to the patient."1
Questions related to IPS should be asked in all interviews, whether the patient specifically mentions online venues/apps or not. Until the original patient (OP) indicates otherwise, it can be assumed that the OP has met or communicated with at least some of their sex partners through an app or online site.
When interviewing patients, DIS can ask about sex partners met online or through apps by using open-ended questions and specifically naming current dating and sex-seeking websites and mobile apps. By naming specific dating sites or apps, the DIS is communicating to patients that the DIS is familiar with and comfortable discussing such venues.
It is important for DIS to be aware of popular online websites and apps used for meeting sex partners. Collecting and recording the names of these websites and mobile apps within a data management system such as MAVEN will help DIS stay abreast of the most current trends and use the information when interviewing patients. See Appendix C for examples of IPS-related questions to ask during interviews.
At a minimum, it is important that DIS attempt to obtain the patient’s screen names, associated venues (website, mobile app), and email addresses and verify physical identifying and location information of partners. Marginal information should also be collected in a program’s data management system. For example, someone may have a tattoo on the back of their left hand or use the screen name “The Rock.” Some programs capture this information in the AKA field.
This information will be useful if a partner references the OP in an interview. If the OP’s screen name is named as a partner in future cases, location information will already exist in the database, and partner notification can be initiated. It is equally important for DIS to gather and confirm the exact spelling of partner screen names, email addresses, and physical location information. Confirming the exact spelling is extremely important, because numbers or other characters are often used in lieu of letters or words, e.g., Man4you vs. Manforu.
However, it is important to remember that all information provided within a profile is subject to change and that the profile itself can be deleted at any time. Lastly, DIS can ask about physical locations where sexual encounters took place such as a person’s home or hotel. This information can help give an approximate geographic location of a partner.
4.2.2 Access to internet/mobile devices during the interview
Having computers and mobile devices with internet access available during the interview can improve the information obtained during an interview. Having access to named websites allows the OP or the DIS to immediately log on to that site to access and verify information about sex partners and can lead to an increase in the number of partners named. Notification emails can also be sent to all sex partners at the time of the interview either through the program's profile or from the patient's personal member profile.
4.2.3 Geographic location of a partner
Prior to initiating IPN, it is important to attempt to obtain and confirm the geographic location of the individual being contacted. Knowing the geographic location of the sex partner will allow the DIS to confirm whether the client resides within the DIS's jurisdiction and provide appropriate referral information (e.g., clinic locations, clinic times). A website member's physical location is often listed within the individual's online profile.
However, due to the ability to change location within many online and mobile sites, the true physical location of a partner may not be known until contact is made. Thus, the location provided in a profile at any given time may not actually reflect the user's residency; it may instead indicate that the partner is "surfing" the site for members in a particular geographic area.
4.2.4 Out of jurisdiction (OOJ) issues
Email addresses and screen names with an identified geographic location outside of a program's jurisdiction may require an "out of jurisdiction" (OOJ) field record to be initiated. Once traditional location information is added to the field record and the record is an OOJ, it should be handled based on existing protocols. It is important to discuss the situation with the appropriate program in the jurisdiction in which the partner is believed to reside to understand that jurisdiction's protocols for handling internet- or app-based location information and IPN.
If traditional location information is not available, but additional contact information is gathered and it is established that the partner is OOJ, programs are encouraged to reach out to the presumed jurisdiction to determine next steps. Protocols can help guide how these different scenarios are handled. If there are no established standards of practice for handling OOJ, these situations will need to be handled on a case-by-case basis.
4.3 Language used for technology-based partner notification
The language used for partner notification varies depending on several factors, including the specific person you are contacting (e.g., someone under age 18 versus over age 18), the venue through which you are attempting to contact a person (e.g., email versus website versus text), the type of infection to which the person has been exposed (e.g., virus versus bacterial STI), and state and local regulations on what can be disclosed via technology. Internet partner services work best when protocols and guidelines allow for notification language to be adjusted based on these factors.
Legitimacy of the notification is enhanced when the following information is included: name of the contacting DIS, program or health department affiliation, contact information, and a brief message encouraging the partner to contact the DIS as soon as possible. If space permits, other information can be included, such as times the DIS can be reached in the office; frequency with which emails, voicemails, etc. are checked; how the patient can confirm the DIS’s identity, such as the name of a supervisor and his/her telephone number; and the case referral number.
It may also be helpful to mention that leaving a voicemail message is confidential, if this is indeed the case. Some programs require all outgoing emails to have a legal disclaimer. Programs can discuss if a legal disclaimer is necessary and what language to use with their legal department.
Sending notifications from and to official health department email addresses or profiles also helps to legitimize the notification for the recipient. Partner notification from any personal account, including personal email addresses or profiles, is discouraged and may be in violation of your program's operating procedures. Whenever possible, messages should be accompanied by an automatic request for notification when the message is read.
4.3.1 Language specificity
Patient characteristics (e.g., adolescent versus adult) and the venue through which you are trying to reach a patient will determine the type of language you use. When deciding what type of language to use when sending a message, care and consideration should be given to both the person you are attempting to reach and the medium through which you are trying to reach them.
Programs typically err on the side of caution and use the most conservative or vague language when there is any concern about potentially breaching confidentiality. Below, we describe the three different ways that messages can be crafted based on the medium. See Appendix D for additional examples of initial IPN emails.
4.3.1.1 "Urgent health matter"
For messages which may be seen by others, like email, and for certain social networking sites where profiles are shared with friends or may be monitored by parents, like Facebook, broad or generic language such as "urgent health matter" is suggested. Instant messaging is not recommended for partner notification, but in cases where it is used, broad or generic language should be employed.
Example 1:
Dear <>
***This message is intentionally vague in order to protect your privacy. ***
I am contacting you about an urgent health matter. It is most important that you report to the _______________ Health Center located at _________________.
Please print a copy of this email and bring it with you as it can reduce your waiting time. If you are unable to bring a copy of the email, please let the health center staff know that you were contacted by me and asked to visit the clinic. If you have any questions regarding this notice, please feel free to contact me at (555) 555-5555 Monday through Friday from 8:30 a.m. to 4:00 p.m.
Services at the health center are free and confidential. If you prefer to consult a private physician, please ask him or her to contact me for information on the health matter I am contacting you about.
If I am not available at the time of your call, please leave a number and time when I can reach you. My voicemail is private, confidential, and password-protected.
This message is intentionally vague in order to protect your privacy. Please visit the health center or contact me by telephone for more information.
Sincerely,
DIS name & accompanying information such as email and telephone number, and clinic address and hours
4.3.1.2 "Exposure to an infectious disease"
Sexual networking sites and certain email addresses, such as those found on dating sites, are more amenable to language that indicates exposure to an unknown infection, such as "you may have been exposed to an infectious disease."
Example 2:
Hi/Hello:
My name is ___________________, and I work for the [insert health department name]. Please contact me as soon as possible; you may have been exposed to an infectious disease. You will need to be examined, even if you do not feel sick.
Please call me at 555-555-5555. If I am not at my desk, please leave a message on my confidential voicemail with your name, phone number, and the best time to reach you.
We offer confidential screening and treatment at no cost at [insert address]. To be seen more quickly, please bring this letter with you when you come in and/or ask for me by name. Our drop-in hours are listed below.
Sincerely,
DIS name & accompanying information such as email and telephone number, and clinic address and hours
** CONFIDENTIALITY NOTICE** This letter and any attachments are solely for the intended recipient and may contain confidential or privileged information. If you are not the intended recipient, any disclosure, copying, use or distribution of the information included in this message and any attachments is prohibited. If you have received this communication in error, please notify the sender immediately and permanently delete or otherwise destroy the information.
4.3.1.3 "Exposure to a specific disease"
Lastly, some sexual networking sites may require the use of disease-specific language when reaching out to their members for partner notification, e.g., "someone you may have had sex with tested positive for syphilis." It is important to review the site or app's TOS and determine what actions are allowed.
Example 3:
To:
From: Name@tn.gov
Subject: (leave blank)
Hello , (do not use screen name)
A few days ago, I sent you an email, but I have not heard back from you.
My name is ____ and I work for the [insert health department name]. I am contacting you because someone who was recently diagnosed with laboratory confirmed asked that you be notified of an exposure to this infection.
It is important that you call me at 555-555-5555 so I can speak with you confidentially about the specific exposure and provide you with options for testing and treatment.
To confirm this email is authentic and legitimate, you can call my supervisor ________ at ####. [If relevant, email can include language describing how the recipient of the email can confirm the legitimacy of the email, e.g., "If you would like to confirm that this email/profile is real, you can contact the {insert website/app name} at {insert email or number}."]
Thank you for your prompt response.
Sincerely,
DIS name & accompanying information such as email and telephone number, and clinic address and hours
End of example
To date, no formal studies have been conducted to determine the most effective means of getting a contacted partner to respond to a DIS; however, anecdotal evidence from experienced programs has found that including specific disease information in proprietary email systems is safe and acceptable to the recipients. In general, proprietary systems are password-protected, and members of websites with proprietary email systems typically have individual accounts. If members choose to share an account with another person, it may be because they are in an open relationship where both partners agree that each may have sex with others or may be looking for group sexual encounters.
The messages you send to contacts may at first be perceived as spam (unsolicited email) or a hoax. To encourage patients to read your message and avoid appearing as spam, some programs leave the subject field blank, containing no text. Other programs have standard subject lines such as "Confidential message from the (insert local health department name)," or, "Please call the (insert local health department name)." If messages aren't being read, new subject lines and methods can be considered.
Where appropriate, subsequent attempts to contact the partner may include additional information to increase the sense of urgency; request the individual's consent to receive information via another medium, such as a private email address; or provide disease-specific exposure information.
Programs will need to determine the allowable number of times a patient may be contacted. Experienced programs recommend no more than three attempts to initiate contact with the patient.
Some websites have policies regarding the number of times a health department or CBO may contact their members, with most limiting it to a maximum of three attempts. It is important to remember that each situation may require different strategies.
See Example 3 above and Appendix E for examples of follow-up emails.
4.4 Confidentiality during partner notification/partner services
4.4.1 Reaching the right person
It's very important to ensure that all emails and messages are sent to the intended recipients. Locating online partners has become much more challenging due to the variable ease and frequency with which email addresses, screen names, and IM and smartphone app accounts can be obtained and changed. Screen names may be very similar and sound the same. For example, members with the screen names "partyboi" or "Man4U" are likely different users than members with the screen names "partyboy" or "Manforyou."
When feasible, have the OP access email and app messages, social media profiles, and text messages to confirm the spelling of partners' profile names during the original interview. If using STD program equipment, be sure that the OP has logged completely out of their account when done. Additionally, eliciting descriptive details about partners, such as race, height, weight, interests, location, and other identifying characteristics like tattoos, can help DIS verify that the correct person is being contacted. Many STD programs report that patient confidentiality can be maintained in the same way that confidentiality is maintained when conducting partner notification via the telephone.
4.4.2 Protecting confidentiality
In some cases, the use of individual identifiers (screen names, email addresses, profile names, etc.) combined with language that specifically mentions exposure to a specific infection, such as HIV, may be interpreted as a confidentiality breach. As mentioned earlier, certain venues may be less secure than others. For example, contacting a minor through Facebook using language such as "someone you had sex with was recently diagnosed with an infectious disease" may be a breach of confidentiality, as many parents monitor their child's Facebook account. However, when contacting the same individual through an online sex-seeking venue where his or her account would most likely not be known to or monitored by a parent, using the same language may be appropriate.
It is important to take extra precaution, however, if the partner is found on another site. For example, if you are looking for ATLDavid on one app but he shows up on another app with the same profile name, one must consider who may see that message on that specific app or website before reaching out to that individual. Individuals we are attempting to contact could also share an email account or profile with another person. However, anecdotally, experienced programs have found that most email addresses and profiles reported are not shared. Profile names that indicate that a profile may be shared by two or more people (e.g., "2hotmen") should be closely reviewed before sending information. If there is evidence that an email or profile is shared, or if any level of uncertainty exists, then information should not be sent and should be discussed with a supervisor.
Some barriers related to confidentiality and messaging can be avoided by using broad or generic messaging that omits any mention of sexual activity. Examples of broad or generic messaging include "potential exposure to an infection" and "urgent health matter."
4.4.3 Making contact with patients
Some health departments have found IPS to be more successful when the OP first contacts the named partners with follow up by DIS, rather than being contacted by the DIS first.
DIS can provide support and guidance to the OP about how to notify their sex partners, including what language to use, available resources (such as testing sites), or example emails. Patient-initiated IPN messages should include the name and contact information of the DIS.
When the OP makes first contact with a potentially infected partner, there are generally three ways in which contact can occur:
- The OP can contact their partner(s) directly on their own initiative, notifying partners of their potential exposure and indicating that a DIS will be reaching out to the partner for STD screening and partner services. Afterward, the OP will follow up with the DIS on whether partners were contacted.
- The OP can notify their partner(s) in the presence of a DIS by contacting partners through health department computers or phones, or by using their own device (e.g., mobile phone). This method provides evidence that partners were, indeed, contacted and notified.
- Lastly, OPs can use third-party sites, which allow them to contact and notify partners anonymously. There are limited outcome evaluation data available on these third-party notification sites, and there is potential for false or "joke" notifications. These sites may have the potential to improve PS for STDs such as chlamydia and gonorrhea, which often do not fall within the purview of PS. However, for STDs such as HIV and syphilis, the DIS model is still recommended, because there is no way of verifying that a partner was notified or that the individual sending the notification has a laboratory-confirmed STD.
When a partner calls or comes to the clinic, it is important to ask how the partner was notified of a potential exposure. If the individual was notified via IPS, the DIS may not have the real name of the individual. Disease intervention specialists should ask the individual for the referral letter or number or his/her online profile name or email address, then search the case management data system (e.g., MAVEN). Once the DIS confirms the identity of the individual through other identifying information obtained from the original patient, the field record needs to be updated. It is important to retain the IPS information such as the profile name and website or app within the data management system for future cross references and for evaluation purposes.
4.5 Text notification & mobile applications
Mobile technologies, specifically texting and the use of mobile apps, have become increasingly relevant to STD prevention and partner notification.
In the U.S., 96% of adults (persons 18 years and older) have a cell phone2 and 81% own a smartphone.3 Increasingly, cell phones are replacing landline telephones. The 2018 National Health Interview Survey found that more than half of American homes (57%) did not have landline telephones but did have at least one wireless phone.4 Smartphones are used for much more than making phone calls—they are used for sending and receiving texts and emails, accessing the internet and social networking sites, getting directions, listening to music, watching TV or movies, and more.567
More is now known about the use of sex-seeking mobile apps and their impact on STDs. Current knowledge about sex-seeking apps has primarily focused on those apps that cater to gay, bisexual, and other men who have sex with men (MSM). Three systematic reviews found that men who use dating and sex partnering apps are engaging in behaviors that put them at increased risk for HIV/STI, such as unprotected anal sex, substance use, and having a high number of sex partners. Additionally, when compared to MSM who do not use these apps, app users were more likely to report a diagnosis of gonorrhea, chlamydia, or syphilis, though no differences were seen in HIV rates.89
4.5.1 Using text messaging/Short Message Service (SMS) for partner notification
A cell phone number is often the only form of contact information available for a partner. As a result, many health departments are exploring how to conduct partner notification through text. Some health departments have already incorporated text messaging into their standard notification attempts. For example, if a mobile phone number is known, then a text message is sent in conjunction with other notification efforts such as telephone calls and emails. Other programs resort to text messaging only when other notification efforts have failed. Regardless of when texting is used, the goal of texting is to get the patient to call the DIS.
Programs have found that texting improves outcomes, reaches people for whom other notification efforts were unsuccessful, and reduces the need for mailing letters or making field visits.1011121314 Programs are encouraged to develop protocols to provide guidance on when the use of texting for partner notification is permitted, the type of language that may be used, how often DIS may text partners, and any program rules that should be followed. See Appendix F for examples of text messaging policies for partner services.
4.5.2 Confidentiality and risks of text messaging
Maintaining patient confidentiality is of the utmost importance when using texts for partner notification. Text messages carry similar risks to other forms of partner notification. Just like a letter or voicemail message that can be read or listened to by someone other than the intended recipient, text messages can also be sent to or read by others. It is important to remember that text messages can be copied, forwarded to others, altered, or stored electronically without authorization or detection. Programs can minimize these risks by taking the following suggested precautions.
- Use broad partner notification language, e.g., "important health matter." Sending disease-specific information via text message is not recommended.
- Send text messages from work-issued devices only. We do not recommend the use of personal cell phones or computers when communicating with clients or their partner(s).
- Ensure that all mobile devices are password protected.
- Send text messages from a private space where no one can see what or who you are texting.
- Use delivery confirmation, if that is an option. Some cell phone carriers will provide you with an option to receive a text message delivery confirmation. This service can be activated through the settings on your mobile phone or through your carrier account preferences.
A concerted effort should be made to ensure that the correct telephone number is being used for contact. This can be done by confirming the contact number with the information on file or by using reverse search tools to confirm the number is connected to a mobile device. At the time of this writing, the website http://www.phonelookup.comexternal icon could reveal whether a number was a mobile or landline phone number and the general location, but it does not provide names or street addresses. It is important to be aware that the information obtained through a reverse lookup may not be the most current information.
4.5.3 Communication etiquette
Understanding and using texting etiquette is important and can help improve response rates from patients and their partners. Following are some helpful tips when communicating by text:
- Be professional at all times. Avoid the use of emoticons, jargon, acronyms, or images.
- Be timely in your response to returned texts. Returned texts can come at any time of the day. Be prepared to respond as soon as possible.
- Recognize that it is extremely difficult to discern tone (humor, sarcasm, etc.) in text messages.
- Know that some users may have a limited text messaging plan and that each incoming and outgoing text may cost them money.
- Texts may be limited in character count. For example, a text message over 160 characters may be split into two messages.
- If, after contacting a patient or partner, you would like to text to confirm an appointment or meeting time, it is important to obtain the person's permission.
4.5.4 Using mobile applications (apps) for partner notification
As with cell phones, sometimes a mobile app profile name may be the only information known about a partner. Health departments are exploring ways to conduct partner notification through mobile apps and are discovering that apps come with a unique set of issues that can make notifying a partner challenging.
Presently, we only know of one dating service, Adam4Adam (aka A4A), that allows DIS and other health specialists to operate on their site for public health purposes. No other dating or sex partnering apps have officially sanctioned the use of their apps for partner services. The programs that are attempting to use mobile apps for partner services have done so without express permission, and many have had their profiles blocked on occasion by the managers of the app.
Most dating and sex partnering apps use a global positioning system (GPS) to increase the speed and efficiency of meeting potential partners. Through GPS, mobile apps can locate users in space and provide that information to other users who are within a designated radius. This geographic specificity creates challenges for partner notification because when a person closes the app or is outside the designated radius, their profile may not be seen. In order to be located via the app, the person the DIS is searching for must be both actively using the app and within the required radius for their profile to appear.
Some DIS may only be permitted by their program to access mobile apps to gather partner information and may not be permitted to send partner notification messages through the app. Additionally, many of the apps do not have a search function, thus preventing DIS from quickly searching the entire mobile app for a specific user.
Another major challenge is ensuring you are reaching the right person. Many mobile apps do not require a unique profile name, so there may be multiple profiles with the same name (e.g., James). Some apps do not require a profile name at all.
Profile names are not always static; the user can change their profile name at any time or delete their profile all together. Finally, a user can block other profiles, including the OP’s and/or the health department’s. As a result, it can be very difficult to ascertain if you are reaching the right person. Using information gathered in the OP interview can help DIS to confirm that they have found the correct partner. If DIS cannot reasonably ensure that they are reaching the right partner, they should not send a partner notification message.
4.5.5 Reaching the right person
The chances of reaching the right person can be improved by working with the OP to access and gather information using the OP's personal mobile app account. The DIS can ask the OP to log onto the mobile app during the interview to look for the partner or to gather identifying information from certain sections of the app. Accessing a patient's mobile app profile can help confirm the spelling of profile names, provide physical descriptions and pictures, and provide forgotten or overlooked information (e.g., cell phone numbers, physical addresses, and profile names of additional sex partners).
Many apps have an internal messaging system as well as a way for users to mark other users so that they can find them quickly in the future. This is often called "favorites" or "followers" within apps. Contact and identifying information can often be found in the "favorites" or "followers" section, as well as in the trash and/or sent folders of the messaging system. Be aware that some app internal messaging systems will purge user messages after a designated period of time.
If the named partner is found on the app when the OP is with the DIS, the DIS can encourage the OP to send a message to the partner in that moment. Studies have found that people prefer to be contacted directly by a partner rather than a DIS when being notified of a possible exposure.15
While it is not necessary for the DIS to look at an OP's mobile phone or mobile app profiles, doing so can be extremely helpful when gathering and verifying partner information. It is always up to the discretion of the patient to determine whether they want to show their profile to the DIS. Allowing someone else to view a personal profile, especially a sex-seeking profile, can make the patient feel vulnerable and subject to judgment. It is important to practice respect and emphasize confidentiality when a patient provides DIS access to their profiles. It is also important to remember that an app profile is a marketing tool to attract sex partners and may contain fantasy, false, or omitted information.
If a patient is unwilling to access their mobile app profiles in the presence of the DIS, the DIS should encourage the patient to email or call with a list of partners and their information. It may be helpful to provide the patient with a list of the types of information sought, e.g., name or user name spellings, physical descriptions, profile names on other social networking sites like Facebook or Instagram, and any location information (telephone, physical address, email address). It is important to emphasize the need to be timely in providing the information.
4.5.6 Other apps and websites to consider for partner notification or gathering partner information
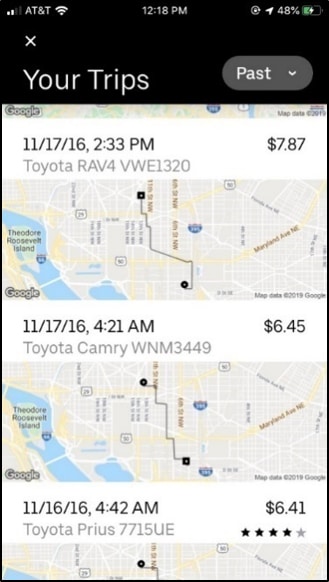
Most people with a smartphone (i.e., iPhone or Android) use a variety of apps beyond dating and sex partnering apps. These other apps can provide useful information to DIS. Rideshare apps (e.g., Uber and Lyft) and navigation and map apps (e.g., Waze and Google Maps) often maintain past travel histories that can help a patient recall a location where they met a partner, including a partner's home.
Google Maps provides aerial and satellite images, as well as 360° panoramic views of streets known as Street View. When a general location or specific address is entered in Google Maps, images of the actual building, home, street, and other surrounding landmarks are often available for viewing.
Free text and voice messaging apps (e.g., WhatsApp) are also growing in popularity. These apps allow users to send and receive messages, and they are an additional way to gather partner information, including contact information like phone numbers and confirmatory information such as photos.
Google Images, an online image catalog, can be used to identify or locate clients or obtain important demographic information. Google Images allows users to search the internet for image content using terms and keywords or to conduct a reverse image search by uploading an image. Images obtained from clients can be uploaded to the Google Image search service and matched against images in Google's index. Any publicly available social media accounts or personal websites of the potential client may be revealed through this search.
The DIS can encourage patients to check these apps during the interview, which may spur the patient's memory of past encounters and provide information that will help locate the partner(s).
- Centers for Disease Control and Prevention. Program Operations Guidelines for STD Prevention: Partner Services. Atlanta, GA. Retrieved from https://www.cdc.gov/std/program/partners.pdf.
- Pew Research Center. (June 12, 2019). Mobile Fact Sheet. Retrieved from Pew Research Center, Internet & Technology website: https://www.pewresearch.org/internet/fact-sheet/mobile/.
- Pew Research Center. (June 13, 2019). Mobile Technology and Home Broadband 2019. Retrieved from Pew Research Center, Internet & Technology website: https://www.pewresearch.org/internet/2019/06/13/mobile-technology-and-home-broadband-2019/.
- Blumberg SJ, Luke JV. Wireless substitution: Early release of estimates from the National Health Interview Survey, July-December 2018. National Center for Health Statistics. June 2019.
- Perrin, A. 10 facts about smartphones as the iPhone turns 10 (June 28, 2017). Pew Research Center. https://www.pewresearch.org/fact-tank/2017/06/28/10-facts-about-smartphones/ (retrieved 12/12/19).
- Pew Research Center. (June 10, 2015). Cell Phone Activities. Retrieved from Pew Research Center, Internet & Technology website: https://www.pewresearch.org/internet/chart/cell-phone-activities/.
- Anderson, M. (January 29, 2016). More Americans using smartphones for getting directions, streaming TV. Pew Research Center. Retrieved from Pew Research Center, Internet & Technology website: https://www.pewresearch.org/fact-tank/2016/01/29/us-smartphone-use/.
- Zou H, Fan S. Characteristics of men who have sex with men who use smartphone geosocial networking applications and implications for HIV interventions: A systematic review and meta-analysis. Archives of Sexual Behavior. 2017; 46(4):885-894.
- Wang H, Zhang L, Zhou Y, Wang K, Zhang X, Wu J, Wang G. The use of geosocial networking smartphone applications and the risk of sexually transmitted infections among men who have sex with men: A systematic review and meta-analysis. BMC Public Health. 2018;18 (1):1178
- Kachur RE, Hall W, Coor, A, Kinsey J, Collins D, Strona F. The use of technology for sexually transmitted disease partner services in the United States: A structured review. 2018; 45(11):707-712.
- Kachur R, Adelson S, Firenze K, Herrera M. Reaching patients and their partners through mobile: Text messaging for case management and partner notification. Sexually transmitted diseases. 2011;38(2):149-150
- Mendez J, Maher J. Evidence supporting the use of text messaging for partner services. Sexually transmitted diseases. 2012;39(3):238-239.
- Hightow-Weidman L, Beagle S, Pike E, et al. "No one's at home and they won't pick up the phone": using the Internet and text messaging to enhance partner services in North Carolina. Sexually transmitted diseases. 2014;41(2):143-148.
- Udeagu CC, Bocour A, Shah S, Ramos Y, Gutierrez R, Shepard CW. Bringing HIV partner services into the age of social media and mobile connectivity. Sexually transmitted diseases. 2014;41(10):631-636.
- Contesse MG, Fredericksen RJ, Wohlfeiler D, Hecht J, Kachur R, Strona FV, Katz DA. Attitudes about the use of geosocial networking applications for HIV/STD partner notification: A qualitative study. AIDS Education and Prevention. 2019:31(3), 273–285.
