Key points
- Shingles rash most commonly appears on the trunk along a thoracic dermatome or on the face.
- People with weakened immune systems are more likely to have atypical presentations.
- Postherpetic neuralgia (PHN) the most common complication of herpes zoster.

Clinical features
People with herpes zoster can have pain, itching, or tingling in the area where the rash will develop.
A person can experience the following symptoms several days before the rash appears:
- Headache
- Photophobia (sensitivity to bright light)
- Malaise
Common symptoms
People with herpes zoster have a rash in one or two adjacent dermatomes. The rash most commonly appears on the trunk along a thoracic dermatome or on the face. It usually does not cross the body's midline.
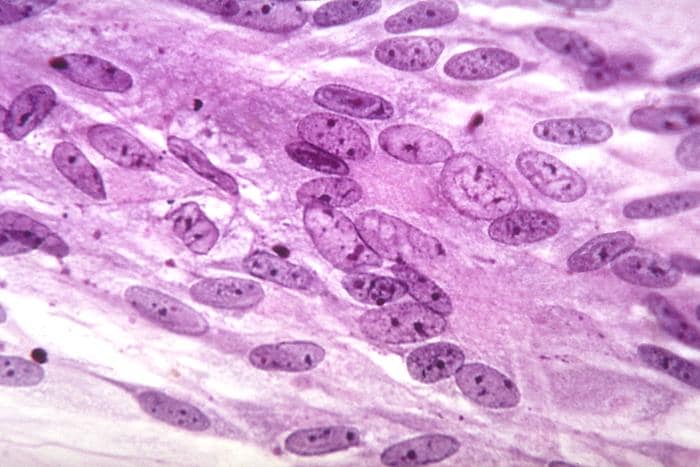
The rash develops into clusters of vesicles. New vesicles continue to form over 3 to 5 days, and the rash progressively dries and scabs over.
The rash usually heals in 2 to 4 weeks. Permanent skin discoloration and scarring can occur.
Clinical diagnosis
The signs and symptoms of herpes zoster are usually distinctive enough to make an accurate clinical diagnosis once the rash appears. However, clinical diagnosis of herpes zoster might not be possible in the absence of a rash. This could be before a rash appears, or in cases of shingles without a rash (called "zoster sine herpete"). Herpes zoster is sometimes confused with the following:
- Herpes simplex, including eczema herpeticum
- Impetigo
- Contact dermatitis and drug eruptions
- Folliculitis
- Scabies, insect bites, and papular urticaria
- Candida infection
- Dermatitis herpetiformitis
Among certain populations
Herpes zoster is hard to diagnose in children and younger adults, especially if the clinical presentation is mild.
People with weakened immune systems are more likely to have atypical presentations (e.g., more severe or generalized rash). To help with diagnosis, consider if patient has:
- A history of VZV exposure.
- A history of a rash that began with a dermatomal pattern.
- Results of VZV antibody testing during or before the time of rash.
Complications
Shingles complications can include:
Postherpetic neuralgia (PHN)
PHN is the most common complication of herpes zoster. PHN is pain that persists in the area where the rash once was located; and continues more than 90 days after rash onset. PHN can last for months or even years.
A person's risk of having PHN after herpes zoster increases with age. Older adults are more likely to have longer lasting and more severe pain. Approximately 10% to 18% of people with herpes zoster will have PHN.
PHN is rare in people younger than 40 years old. The likelihood of PHN is also higher in people who experience more pain with the rash or have a large rash.
Herpes zoster ophthalmicus (HZO)
Herpes zoster that affects the ophthalmic division of the trigeminal nerve is called herpes zoster ophthalmicus. This can result in acute or chronic ocular sequelae, including vision loss.
Disseminated zoster
Disseminated zoster can include generalized skin eruptions where the lesions occur outside of the primary or adjacent dermatomes. It can be difficult to distinguish from varicella.
Visceral involvement of the central nervous system (meningoencephalitis), lungs (pneumonitis), and liver (hepatitis) can also occur. Disseminated zoster generally occurs in people with compromised or suppressed immune systems.
People with compromised or suppressed immune systems are more likely to:
- Have a severe, long-lasting rash.
- Experience more severe complications from herpes zoster.
Other complications
- Bacterial superinfection of the lesions, usually due to Staphylococcus aureus and, less commonly, due to group A beta-hemolytic streptococcus.
- Cranial and peripheral nerve palsies.
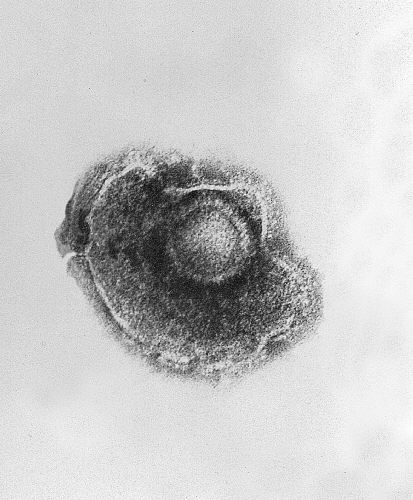
Laboratory testing
Laboratory Testing for Varicella-Zoster Virus (VZV)
Specimen Collection for Varicella-Zoster Virus (VZV) Testing