Key points
- Herpes zoster (shingles) is caused by the reactivation of varicella-zoster virus (VZV) and can be prevented with Shingrix vaccine.
- Herpes zoster is hard to diagnose in children and younger adults, especially if the clinical presentation is mild.
- Older adults and people who are immunocompromised are at high risk for shingles complications.

Cause
Herpes zoster (shingles) is caused by the reactivation of varicella-zoster virus (VZV), the same virus that causes varicella (chickenpox).
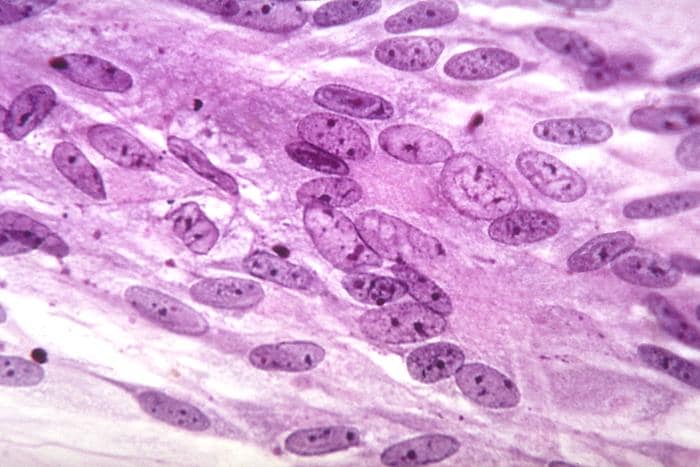
Primary infection with VZV causes varicella. After a person has varicella, the virus remains dormant in the dorsal root ganglia. VZV can reactivate later in a person's life and cause herpes zoster, a painful maculopapular, and then a vesicular rash.
Who is at risk
People who had chickenpox can get shingles.
About 1 in 3 people in the United States will develop herpes zoster during their lifetime. Most people have only one episode, but herpes zoster can recur.
A person's risk for herpes zoster and related complications, including hospitalizations, sharply increases after 50 years of age. The reasons why VZV reactivates and causes herpes zoster are not well understood.
However, a person's risk for herpes zoster increases as their VZV-specific cell-mediated immunity declines. This decline in immunity can result from increasing age and medical conditions or medications that suppress a person's immune system.
People with the following conditions that compromise or suppress their immune system have an increased risk for herpes zoster:
- Bone marrow or solid organ (renal, cardiac, liver, and lung) transplant recipients.
- Cancer, especially leukemia and lymphoma.
- Human immunodeficiency virus (HIV).
- Taking immunosuppressive medications, including steroids.
About 30% of people hospitalized with herpes zoster have compromised or suppressed immune systems.
Other potential risk factors for herpes zoster have been identified, but the findings are inconsistent or unexplained. For example:
- More women than men develop shingles.
- Herpes zoster is less common in black people than in white people.
How it spreads
People with active herpes zoster lesions can spread VZV. VZV causes varicella in people who never had chickenpox or those who didn't receive the varicella vaccine. Once varicella resolves, these people would be at risk for herpes zoster.
Active herpes zoster lesions are infectious through direct contact with vesicular fluid; or breathing in virus particles from the blisters until they dry and scab over.
People with active herpes zoster lesions should cover their lesions; and avoid contact with susceptible people in their household and occupational settings until their lesions are dry and scabbed.
Disease rates
An estimated one million cases of herpes zoster occur annually in the United States. The incidence of herpes zoster varies by age and is approximately two to nine cases per 1,000 US population annually. The precise incidence of recurrence is not known.
Death rates
One study estimated 96 deaths occur each year where herpes zoster was the underlying cause (0.28–0.69 per 1 million population). Almost all of the deaths were in older adults or those with weakened immune systems.
Clinical features
People with herpes zoster can have pain, itching, or tingling in the area where the rash will develop.
People with herpes zoster have a rash in one or two adjacent dermatomes. The rash most commonly appears on the trunk along a thoracic dermatome or on the face. It usually does not cross the body's midline and heals in 2 to 4 weeks.
Shingles complications include postherpetic neuralgia, hearing or vision loss, encephalitis, and pneumonia.
The signs and symptoms of herpes zoster are usually distinctive enough to make an accurate clinical diagnosis once the rash appears. However, clinical diagnosis of herpes zoster might not be possible in the absence of a rash.
Prevention
CDC recommends 2 doses of recombinant zoster vaccine (RZV, Shingrix) to prevent shingles and related complications in adults 50 years and older. Shingrix is also recommended for adults 19 years and older who have weakened immune systems because of disease or therapy.
Varicella vaccines contain live attenuated VZV, which results in latent infection. Although herpes zoster has always been uncommon among children, the rate in U.S. children has declined since the routine varicella vaccination program started in 1995.
- Children (healthy and immunocompromised) vaccinated against varicella have lower rates of herpes zoster when compared to children who had natural infection with varicella.
- Vaccinated children are less likely to become infected with wild-type VZV.
- The risk of reactivation of vaccine-strain VZV in children is lower when compared with reactivation of wild-type VZV.
- Vaccinated children are less likely to become infected with wild-type VZV.
- Few older adults have received the varicella vaccine since it was licensed in 1995. There is very little information on the risk of herpes zoster in people who got varicella vaccine as adults.
The CDC continues to monitor the impacts of the U.S. varicella and herpes zoster vaccination programs among adults and children.
Testing
Varicella-zoster virus (VZV) laboratory testing information applies to testing and diagnosis of primary VZV infection (varicella) and reactivation (herpes zoster). Polymerase chain reaction (PCR) is the most helpful laboratory test for confirming cases of herpes zoster. PCR can detect VZV DNA rapidly.
Treatment and recovery
Diagnose and treat early!
There are three preferred antiviral drugs available for the initial treatment of shingles:
- Acyclovir
- Valacyclovir
- Famciclovir
These antivirals accelerate the resolution of lesions; reduce the development of new lesions and viral shedding; and decrease the severity of acute pain. Discuss treatment options with your patient to provide a specific treatment plan based on their condition.
Trends
Previously, herpes zoster rates in the United States gradually increased over a long period. We don't know the reason for that increase. Recently, herpes zoster rates across age groups have recently plateaued or declined.
CDC studies have found that rates started increasing before the varicella vaccine was introduced in the United States; and did not accelerate after the routine varicella vaccination program started.
Resources
- Shingles Vaccine Information for Healthcare Professionals
- Five things you should know about shingles | Sermo
- Zoster (Shingles) | Immunize.org
- ACIP Recommendations for Use of Herpes Zoster Vaccines | MMWR
- ACIP Recommendations for Use of RZV in Immunocompromised Adults | MMWR
- Common Shingrix Reactions: Which Can Be Prevented? | Medscape
- CDC. Use of Recombinant Zoster Vaccine in Immunocompromised Adults Aged ≥19 Years: Recommendations of the Advisory Committee on Immunization Practices — United States, 2022. MMWR Recomm Rep. 2022;71(3):80-84.
- Leung et al. The Impact of Universal Varicella Vaccination on Herpes Zoster Incidence in the United States: Comparison of Birth Cohorts Preceding and Following Varicella Vaccination Program Launch. Journal of Infection Diseases. 2022.
- Harpaz and Leung. The Epidemiology of Herpes Zoster in the United States During the Era of Varicella and Herpes Zoster Vaccines: Changing Patterns Among Older Adults. Clin Infect Dis.2019;69(2):341-344.
- CDC. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP) Recommendations for use of Herpes Zoster Vaccines. MMWR Recomm Rep. 2018;67(03):103-108.
- Thomas SL, Hall AJ. What does epidemiology tell us about risk factors for herpes zoster?Lancet Infect Dis. 2004;4(1):26-33.
- Tseng HF, Smith N, Harpaz R, et al. Herpes zoster vaccine in older adults and the risk of subsequent herpes zoster disease. JAMA. 2011;305(2):160-6.
- Mahamud A, Marin M, Nickell SP, et al. Herpes zoster-related deaths in the United States: validity of death certificates and mortality rates, 1979-2007. Clin Infect Dis.2012;55(7):960-6.
- Leung J, Harpaz R, Molinari NA, et al. Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clinical Infectious Diseases. 2011;52(3):332-340.
- Yih W, Brooks D, Lett S, et al. The Incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccine coverage. BMC Public Health. 2005;5(68).
- Jumaan AO, Yu O, Jackson LA, et al. Incidence of herpes zoster, before and after varicella vaccination-associated decreases in the incidence of varicella. Journal of Infectious Diseases. 2005;191:2002-7.
- Hales CM, Harpaz R, Joesoef MR, Bialek SR. Examination of links between herpes zoster incidence and childhood varicella vaccination. Annals of Internal Medicine. 2013;159(11):739-45.
- Russell ML, Dover DC, Simmonds KA, Svenson LW. Shingles in Alberta: before and after publicly funded varicella vaccination. Vaccine. 2014;32(47):6319-24.
- Weinmann S, Chun C, Schmid DS, et al. Incidence and clinical characteristics of herpes zoster among children in the varicella vaccine era, 2005–2009. Journal of Infection Diseases. 2013;208(11):1859-68.
- Hardy I, Gershon AA, Steinberg SP, LaRussa P. The incidence of zoster after immunization with live attenuated varicella vaccine. A study in children with leukemia. Varicella Vaccine Collaborative Study Group. N Engl J Med. 1991;325(22):1545-50.