Key points
- Plague should be considered in any patient with clinical signs of plague and a recent history of residence in or travel to the western United States or other plague endemic areas.
- If plague is suspected, pre-treatment specimens should be taken if possible, but treatment should not be delayed. Local and state health departments should be notified immediately.
Considerations
DO NOT WAIT FOR DIAGNOSTIC TEST RESULTS IF YOU SUSPECT PLAGUE
Never delay or withhold treatment pending the receipt of laboratory test results. The decision to initiate antibiotic therapy for plague should be made based on clinical signs and symptoms and a careful patient history. A recent flea bite, exposure to areas with rodents, or contact with a sick or dead animal are risk factors for plague in endemic areas.
Specimen collection
If plague is suspected, pre-treatment specimens should be taken if possible, but treatment should not be delayed. Specimens should be obtained from appropriate sites for isolating the bacteria, based on the clinical presentation, and may include:
- Lymph node aspirate: An affected bubo typically contains numerous organisms that can be evaluated microscopically and by culture.
- Blood: Routine blood cultures are a sensitive means of detecting Y. pestis. In later stages of disease, levels of bacteremia are high enough that organisms may occasionally be seen by microscopy on blood smears.
- Respiratory Specimens: Culture is possible from sputum of very ill patients with pneumonic plague; however, blood is usually culture positive at this time as well.
- Biopsy or autopsy specimen: Lymphoid, spleen, lung, or liver tissue can be evaluated by culture.
Recommended tests
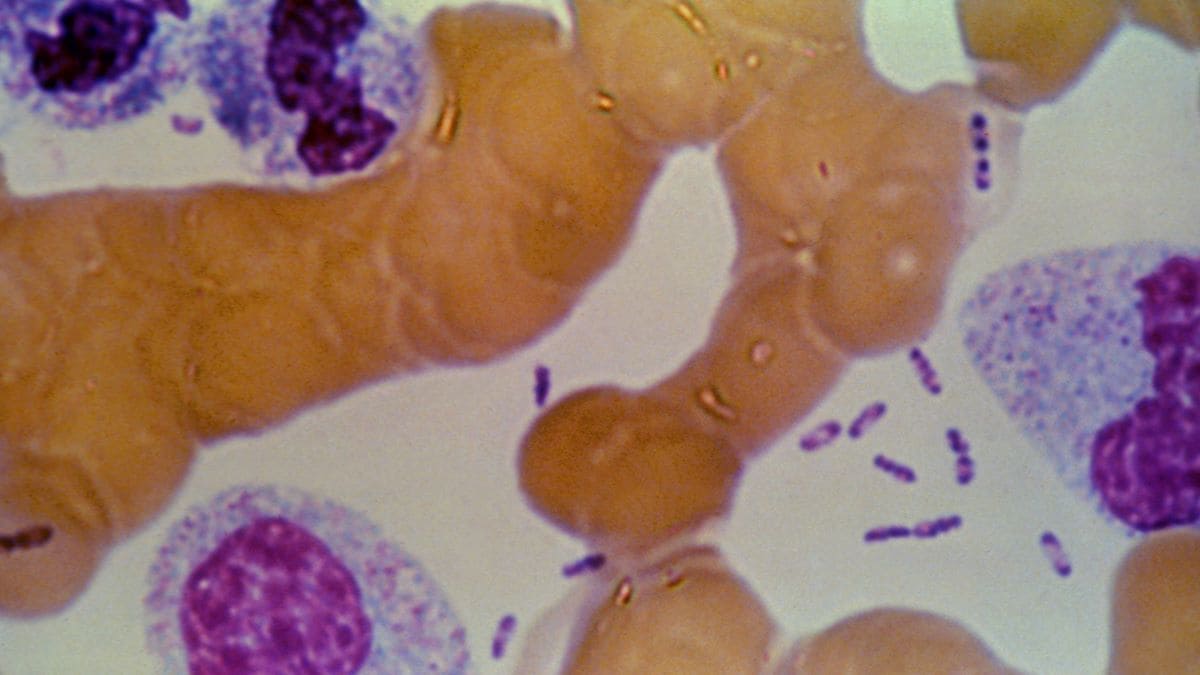
Microscopic examination of Gram, Wright, Giemsa, or Wayson's stained smears of peripheral blood, lymph node specimen, or sputum may yield evidence of Y. pestis infection. Visualization of small Gram negative rods with Gram stain and bipolar-staining with Wright, Giemsa or Wayson stains, (organisms with a "safety pin" appearance) should trigger the suspicion of plague.
Blood cultures are a sensitive means of isolating Y. pestis. If cultures yield negative results and plague is still suspected, serologic testing is possible to confirm the diagnosis. One serum specimen should be taken as early in the illness as possible, followed by a convalescent sample 4-6 weeks or more after disease onset.
NOTE: Automated biochemical identification systems and matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) identification systems may not contain Y. pestis in their databases, which can result in a misidentification of an Y. pestis isolate as Yersinia pseudotuberculosis.
Diagnosis
Plague should be considered in any patient with clinical signs of plague and a recent history of residence in or travel to the western United States or other plague endemic areas. Bubonic plague is the most common primary manifestation, with a bubo usually occurring in the groin, axilla, or cervical nodes. Buboes are often so painful that patients are generally guarded and have restricted movement in the affected region. The incubation period for bubonic plague is usually 2 to 8 days. If bubonic plague is untreated, Yersinia pestis can invade the bloodstream and spread rapidly, causing sepsis; if the lungs are seeded, pneumonia can develop.
Sepsis and pneumonia can also be primary manifestations of plague. The incubation period of septicemic plague is poorly defined but likely occurs within days of exposure, while the incubation period of pneumonic plague is usually just 1 to 3 days. A person with pneumonic plague may experience high fever, chills, cough, and dyspnea and may expel bloody sputum. If patients with pneumonic or septicemic plague are not given specific antibiotic therapy, the disease can progress rapidly to death.
Although the majority of patients with plague present with a bubo, some may have nonspecific symptoms. For example, septicemic plague can present with prominent gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain (MMWR, 2006). Additional rare forms of plague include pharyngeal, meningeal, and cutaneous.
If plague is suspected, local and state health departments should be notified immediately. If the patient has signs of pneumonic plague, they should also be isolated and placed on droplet precautions to reduce the risk of person-to-person transmission of plague.
Reporting cases
If plague is suspected, local and state health departments should be notified immediately. If the patient has signs of pneumonic plague, they should also be isolated and placed on droplet precautions to reduce the risk of person-to-person transmission.
Plague Case Report Form (for public health officials’ use)
