Specimen Collection and Diagnostic Testing
Scientists consider culture the gold standard because it is the only 100% specific method for Bordetella pertussis identification. Other tests that can be performed include polymerase chain reaction (PCR) and serology.
Obtaining a nasopharyngeal (NP) swab or aspirate
Determining who has pertussis can be difficult. Whenever possible, clinicians should obtain an NP swab or aspirate from all persons with suspected pertussis. A properly obtained NP swab or aspirate is essential for optimal diagnostic results. The same specimen can be used both for culture and PCR.
Pertussis Testing Video: Collecting a Nasopharyngeal Swab Clinical Specimen
(4:12 minutes, Date Released: 2/14/2011)
This video demonstrates proper techniques for collecting and transporting a pertussis clinical specimen obtained by swabbing the posterior nasopharynx.
Pertussis Testing Video: Collecting a Nasopharyngeal Aspirate Clinical Specimen
(4:14 minutes, Date Released: 2/14/2011)
This video demonstrates proper techniques for collecting and transporting a pertussis clinical specimen from the posterior nasopharynx obtained by aspiration.
Proper technique for obtaining an NP specimen for isolation
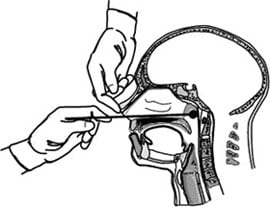
Image: Manual for the Surveillance of Vaccine-Preventable Diseases, 2015
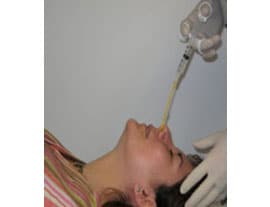
Image: Courtesy of CDC
Culture
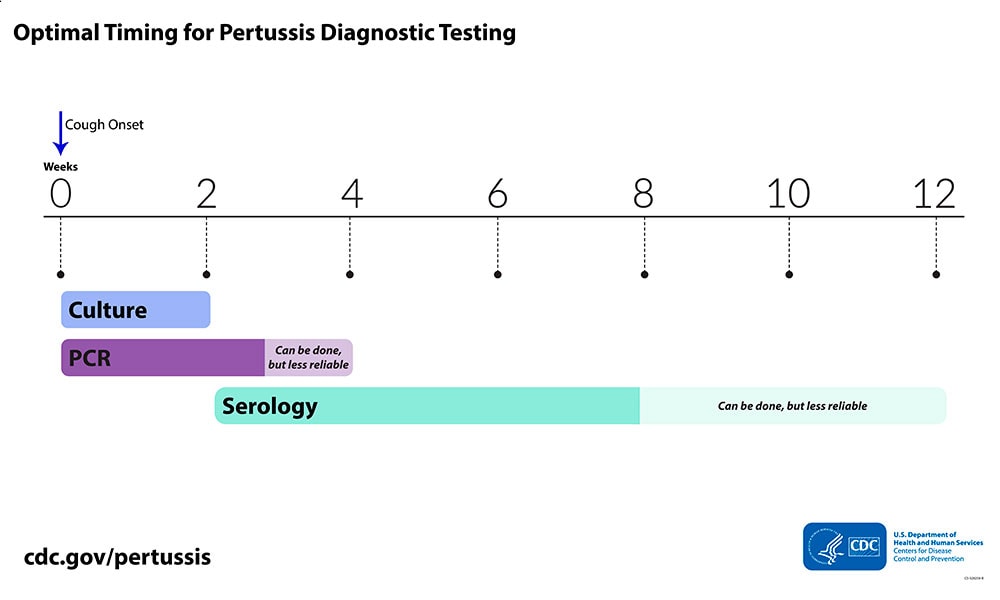
- Use during the first 2 weeks following cough onset; sensitivity decreases and the risk of false negatives increases after 2 weeks
- Gold standard for pertussis diagnosis; the only 100% specific method for identification
Since culture has excellent specificity, it is particularly useful for confirming pertussis diagnosis when an outbreak is suspected. Many other respiratory pathogens have similar clinical symptoms to pertussis and co-infections do occur. Obtaining isolates from culture allows for strain identification and antimicrobial resistance testing. Identifying which strains of B. pertussis are causing disease is of public health importance.
Timing of specimen collection for culture
Ideally, specimens should be collected during the first 2 weeks of illness following cough onset. This is when viable bacteria are still present in the nasopharynx. After the first 2 weeks, sensitivity decreases and the risk of false-negatives increases.
If culture is planned, directly plate the collected NP swab or immediately place it into transport medium. Laboratory scientists should plate NP swabs and aspirates within 24 hours of collection.
Culture has better specificity than PCR, but takes up to 7 days to obtain results.
PCR
- Use up to 3 to 4 weeks following cough onset
- The most rapid test available
PCR is a rapid test and has excellent sensitivity. However, PCR tests vary in specificity. Results should be interpreted along with the clinical symptoms and epidemiological information and in the setting of an outbreak, culture confirmation of at least one case should occur. PCR assay protocols that include multiple target sequences allow for speciation among Bordetella species. The high sensitivity of PCR increases the risk of false-positivity, but following some simple best practices can reduce the risk of obtaining inaccurate results.
Timing of specimen collection for PCR
Ideally, you should collect the specimen during the first 3 weeks of illness following cough onset, but PCR may provide accurate results on specimens collected up to 4 weeks. The same specimen can be used both for culture and PCR. After the fourth week of cough, the amount of bacterial DNA in the nasopharynx rapidly diminishes, which increases the risk of obtaining a false-negative result.
Use of polymerase chain reaction (PCR) for diagnosing pertussis: Best practices
Serology
- Use 2 to 8 weeks following cough onset for optimal results but can be used up to 12 weeks following cough onset
- Can be performed much later than culture and PCR, more useful later in the course of disease
CDC and the U.S. Food and Drug Administration (FDA) developed a serologic assay that has been useful for confirming diagnosis, especially during suspected pertussis outbreaks. A few state public health laboratories have included this assay as part of their testing regimen for pertussis. This assay is also available for research or surveillance purposes through CDC’s test directory.
Commercially, there are several different serologic tests used in the United States with unproven or unknown clinical accuracy. CDC performed an evaluation of several commercially available assays in the United States and found great variability between them, depending on the antigen or antibody used and whether they were calibrated to an international reference serum. Analysis found the most promising assays were those that measured IgG antibodies against pertussis toxin only and were calibrated to a reference standard.
Timing of specimen collection for serology
For the CDC single point serology test, the optimal timing for specimen collection is 2 to 8 weeks following cough onset, when the antibody titers are at their highest. However, testing may be performed on specimens collected up to 12 weeks following cough onset as serologic tests are more useful for diagnosis in later phases of the disease.