
Dialysis More Available Than Patient Education in Counties With High Diabetes Prevalence
ORIGINAL RESEARCH — Volume 21 — August 15, 2024
Janice C. Probst, PhD1; Nicholas Yell, MS1; Gabriel A. Benavidez, MPH, PhD2; Mary Katherine McNatt, DrPH, MPH3; Teri Browne, PhD, MSW4; Laura Herbert, DNP5; Whitney E. Zahnd, PhD6; Elizabeth Crouch, PhD1 (View author affiliations)
Suggested citation for this article: Probst JC, Yell N, Benavidez GA, McNatt MK, Browne T, Herbert L, et al. Dialysis More Available Than Patient Education in Counties With High Diabetes Prevalence. Prev Chronic Dis 2024;21:240052. DOI: http://dx.doi.org/10.5888/pcd21.240052.
PEER REVIEWED
What is already known?
Diabetes is a major contributor to the development of end stage renal disease (ESRD). Diabetes self-management education and support (DSMES), which could delay or avoid the onset of ESRD, is not used by all people with diabetes.
What is added by this report?
We compared the geographic availability, at the county level, of DSMES and dialysis, the principal treatment for ESRD. DSMES was less available than dialysis in counties falling in the top quartile for estimated diabetes prevalence.
What are the implications for public health practice?
Public health planners need to assess local availability of DSMES and partner to improve availability where needed.
Abstract
Introduction
Poorly controlled diabetes is a principal cause of end stage renal disease (ESRD), generating an estimated 44% of new cases. Diabetes self-management education and support (DSMES) has been documented to reduce adverse outcomes such as ESRD. Helping patients better manage their condition could ultimately reduce ESRD prevalence.
Methods
We compared the county-level availability of DSMES and dialysis as of November 2022 sorted by the estimated prevalence of diabetes among residents aged 18 years or older. The locations of DSMES programs and ESRD dialysis facilities were obtained from 2 professional organizations and the Centers for Medicare & Medicade Services. Estimated diabetes prevalence was obtained from the Centers for Disease Control and Prevention’s PLACES data set. Counties were considered to have high diabetes prevalence if they fell into the top quartile for diabetes prevalence in 2019 (≥14.4% of adults). Analyses were conducted in 2023.
Results
DSMES was available in 41.0% of counties but in only 20.7% of counties with high diabetes prevalence versus 47.9% of low prevalence counties. Dialysis facilities were present in 59.2% of all counties, in 52.8% of all high diabetes prevalence counties, and in 61.4% of other counties. DSMES availability was linked to the presence of a hospital in the county, with only 6.3% of counties without a hospital offering the service.
Implications
DSMES could play a role in reducing the prevalence of ESRD. Public health professionals need to be aware of the differing levels of local availability of this service and work to develop partnerships to provide DSMES in high-prevalence areas not currently served.
Introduction
Diabetes is a debilitating chronic disease and a major contributor to other chronic conditions (1). The disorder affected an estimated 11.6% of the US population in 2022, about 34 million people (2), and generated annual medical care costs estimated at $412.9 billion (3). In 2020 it was the eighth leading cause of death (4). Of particular importance, an estimated 44.0% of new diagnoses of end stage renal disease (ESRD) are diabetes-related (5,6). Both type 1 and type 2 diabetes contribute to the onset of kidney disease, principally through the adverse effects of excess glucose on blood vessels in the kidney (7).
Chronic kidney disease is estimated to affect 14% of US adults, with Black adults being particularly affected (18.8%) (8). When the disease progresses to the point where the kidneys no longer function — ESRD — the patient must receive dialysis or a kidney transplant to survive. As of 2021, 808,526 people in the US were living with ESRD.
ESRD care places burdens on the patient, the patient’s family, and the health care system. When the kidneys no longer function, waste must be cleared from the body by external devices. The most common treatment, hemodialysisis, is conducted at a dedicated facility 3 or 4 times a week, and sessions can interfere with work or other activities. The resources and stress associated with both the transplant process and hemodialysis affect family well-being (9). Finally, the cost of ESRD to the US health care system exceeded $50 billion in 2021 and made up about 6.8% of Medicare expenditures (8).
Improved diabetes care may help reduce the prevalence of kidney disease. The adverse effects of diabetes are reduced when people with the disorder successfully manage their condition. They must monitor their blood glucose levels, adhere to diet and exercise guidelines, and take appropriate medications. Because the complexity of diabetes management goes beyond typical instructions for outpatient care, diabetes self-management education and support (DSMES) programs that use standardized, evidence-based curricula have been developed (10,11). DSMES has been shown to improve glycemic control and reduce mortality among people with diabetes (12,13), and it is a covered service under Medicare. In addition, 43 states require DSMES coverage for private insurers and Medicaid (14). Despite these efforts to promote DSMES, patient participation remains low, with one estimate showing that slightly more than half of people with diabetes report receiving this education (15). Lack of DSMES providers at the local level may be one factor affecting patient participation (16).
Because diabetes is an important pathway to the development of ESRD, we sought to compare the relative geographic availability of DSMES and dialysis services. From a prevention viewpoint, ensuring that DSMES is available might serve to reduce the need for ESRD treatment over the long term. Areas that have only dialysis facilities for treatment of this major diabetes outcome but lack DSMES for prevention require public health attention. We used a combination of data sources to identify counties that have a high need for DSMES, based on estimated diabetes prevalence, and assessed the services available in these counties.
Methods
We conducted a cross-sectional analysis in 2023 of the availability of DSMES and dialysis facilities in US counties (N = 3,141). Data from the multiple sources that follow were linked for the analysis.
Diabetes self-management education
We obtained addresses of all accredited DSMES providers as of December 2022 from the American Diabetes Association and the Association of Diabetes Care and Education Specialists. All locations offering DSMES, both main and branch locations, were included in these lists. This information is also publicly available on the respective organizations’ websites. Addresses were geocoded to the county level by using the US Housing and Urban Development’s (HUD’s) USPS ZIP Code Crosswalk Files (17). Because zip codes can overlap county boundaries, the HUD algorithm uses the physical location of most businesses and residences to assign a zip code to a county. Assessment suggests that the rate of misassignment at the county level is minimal (18). Online accredited programs and services of the Veterans Administration and Department of Defense were not included.
Dialysis
We downloaded a list of Medicare-certified dialysis facilities as of November 16, 2022, from the Centers for Medicare & Medicaid Services (CMS) website (19). Addresses were geocoded to the county level. Dialysis is not the only treatment for kidney failure; a kidney transplant is an alternative approach. However, the presence of a dialysis facility in the county suggests access to clinicians such as nephrologists who could refer patients for transplant (20).
Estimated population with diabetes
The CDC PLACES (Population Level Analysis and Community Estimates) data set provided estimates for the proportion of the adult population with diabetes (21). PLACES prevalence values are based on self-report of diabetes in the 2019 Behavioral Risk Factor Surveillance System survey, with statistical modeling used to create county-level estimates. The PLACES data set did not include information for 2 of the 3,143 US county equivalents, the Chugach Census Area and the Copper River Census Area in Alaska; thus, the total counties studied was 3,141. Counties were designated as high prevalence if the estimated proportion of the adult population with diabetes was in the highest quartile across all counties (≥14.4%, n = 790, range 14.4% – 25.9%) versus all lower quartiles (≤14.3%, n = 2,351, range 7.3% – 14.3%).
County characteristics
Characteristics such as population size, demographics, areas with shortages of health care clinicians per Health Professional Shortage Area (HPSA) guidelines, and access to health care resources such as a hospital or a federally qualified health center (FQHC), were drawn from the Robert Wood Johnson Foundation County Health Rankings data set, 2022 edition (22,23). Definitions for rurality were obtained from the Economic Research Service of the US Department of Agriculture and are based on Urban Influence Codes (24).
Analysis
We used χ2 cross-sectional analyses to test for categorical differences and the Mann–Whitney test to examine medians. Because the study was primarily descriptive, we did not conduct multivariable analyses. All analyses were conducted in Stata version 18 (StataCorp LLC) with an α level of .05. We used ArcGIS version 10 (Esri) to produce all maps. Our research was deemed exempt by the institutional review board of the University of South Carolina.
Results
Estimated diabetes prevalence
The national estimated county-level prevalence of diabetes among adults ranged from a low of 6.2% to a high of 25.9%. Counties falling in the highest quartile for prevalence had an average adult prevalence of 16.2%, versus 11.6% in other counties.
The Southern region had the highest proportion of counties with high diabetes prevalence (47.5%) (Table 1). Overall, most counties with high diabetes prevalence were in the South (675 of 790 [85.4%] high-prevalence counties). High prevalence counties were more likely than their counterparts to be rural, to have entire or partial shortages of primary care clinicians, to be served by a federally qualified health center, and to lack a hospital (Table 1). Examining demographic characteristics, high prevalence counties contained relatively high proportions of non-White residents, uninsured adults, and child poverty households (Table 2). Of relevance for access to online DSME, the median proportion of households with broadband access in high-prevalence counties was 71.4%, versus 81.6% in low-prevalence counties (Table 2).
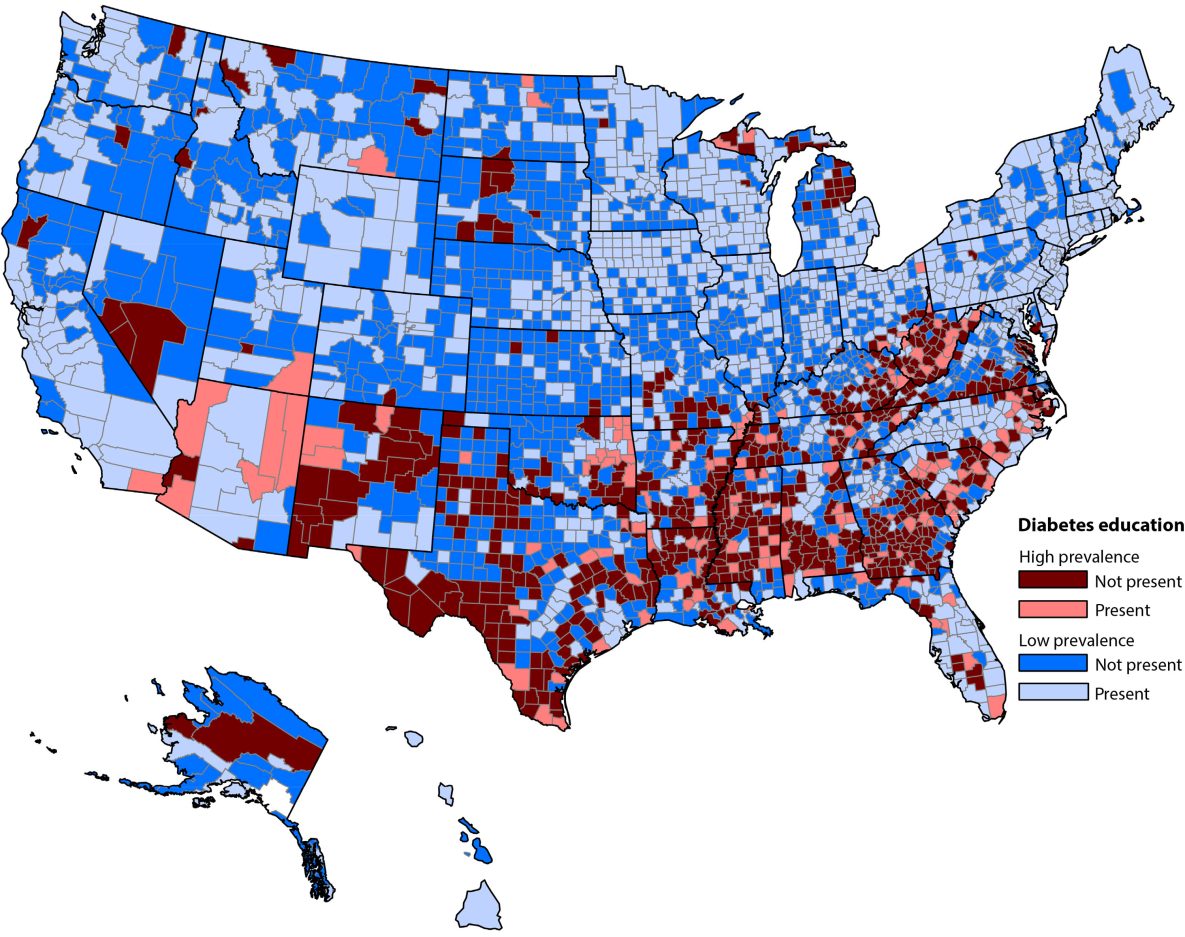
DSMES availability
Across the US, 41.0% of all counties contained at least 1 location where DSMES was offered (1,289 counties) (Table 1). However, DSMES was available in only 20.7% of counties with high diabetes prevalence, versus 47.9% of low-prevalence counties (Figure 1). Of note, only 30.1% of rural counties had an in-county DSMES program (Table 3). DSMES availability was linked to the presence of health care resources in the county. Counties designated as whole county Health Professional Shortage Areas for primary care were unlikely to have locally available DSMES (Table 3).
![]()
Figure 1.
Availability of diabetes self-management education and support (DSMES) and county (N = 3,141) diabetes prevalence (top quartile [≥14.4%] versus all lower quartiles [≤14.3%], 2019 estimates) (21). The PLACES data set does not include information for 2 county equivalents in Alaska, the Chugach Census Area and the Copper River Census Area. Source: Centers for Disease Control and Prevention. PLACES: Local Data for Better Health (21). [A text version of this figure is available.]
Examination of the infrastructure associated with in-county DSMES showed that counties that had both a hospital and an FQHC were most likely to also contain DSMES (57.1%), followed by counties with a hospital but not an FQHC (37.2%) (Table 4). Only 272 of 3,141 counties studied (8.7%) did not have at least 1 of these facilities. However, even among counties with both a hospital and an FQHC, 42.9% lacked DSMES.
Dialysis availability
Dialysis services were more broadly available than DSMES, with at least 1 facility present in 59.2% of all counties (Table 1). Within the 790 counties with high diabetes prevalence, dialysis, either alone (36.5%) or with DSMES (16.3%) (Table 3), was available in 417 counties (52.8%) (Figure 2). Having a dialysis facility but no DSMES, that is, treatment facilities but no prevention activities, was more common in high-prevalence than low-prevalence counties, 36.5% versus 20.7%, respectively.
![]()
Figure 2.
Dialysis availability and county diabetes prevalence (top quartile [≥14.4%] versus all lower quartiles [≤14.3%]), 2019 estimates) (21). DSMES, either alone or with dialysis, was available in 417 (52.8%) counties. The PLACES data set does not include information for 2 county equivalents in Alaska, the Chugach Census Area and the Copper River Census Area. Source: Centers for Disease Control and Prevention. PLACES: Local Data for Better Health (21). [A text version of this figure is available.]
Discussion
Reflecting the inverse care law (25), DSMES was less available in counties in the top quartile for estimated diabetes prevalence than in other counties. Paradoxically, a larger proportion of high-prevalence counties had the resources to treat ESRD (52.8%) than to provide education that might lower its prevalence (20.7%). Nearly all counties studied contained either a hospital or an FQHC; only a small fraction had neither (8.7%). Nonetheless, many counties that housed these facilities did not have a local DSMES program. Even when a county had both types of facilities, 42.9% did not have DSMES.
Public health practitioners could partner with hospitals and FQHCs to expand DSMES availability. Nonprofit hospitals are required to provide community benefit services to maintain their tax-exempt status; however, most funding for community benefit goes to charity care. Only a small portion is allocated for education (26).
Several potential barriers need to be addressed for partnerships to be successful at expanding DSMES availability. Unlike dialysis, DSMES does not have a guaranteed funder, nor is it a substantial revenue source. Since 1973, Medicare has been the guaranteed payor for all ESRD care, including dialysis (27,28). Dialysis generates considerable income for providers. Its annual cost in 2021 was estimated at approximately $99,000 per patient for hemodialysis and $87,000 for peritoneal dialysis (8). DSMES, on the other hand, is billed at roughly $56 per 30-minute individual session, and about $16 per person for group sessions (2022 national average rates) (29). In addition, clinicians cannot bill Medicare for DSMES on the same day as a visit for other purposes, making it difficult to bundle services to promote patient engagement. Not only does this reduce potential income for the clinician, but it may also decrease patient participation. Of note for underserved populations, Medicare restricts the degree to which FQHCs may bill for DSMES (30). Finally, because DSMES providers can bill Medicare for only 10 sessions during a patient’s first year of a diabetes diagnosis or first year on Medicare, and 2 hours per year thereafter, DSMES is not a substantial revenue-generating service.
Another factor affecting availability of DSMES is that a diabetes education provider must meet certain requirements to be certified (10). DSMES educators must document their education, the curriculum they will use for patient education, quality control activities, and other features of the education program. Public health agencies may need to partner with local hospitals or other health care professionals to find ways to subsidize the process of obtaining DSMES certification and the cost of providing the service to patients. Finally, multiple barriers restrict use of DSMES, some of which could be reduced by policy changes. For DSMES to be billable, the patient’s health care provider must provide a written or electronic order for that service (31). Thus, communication with clinicians is necessary to make DSMES programs available to patients, including online, virtual, or in-person courses. Adjustments to patient flow or prompts in the electronic health record may be needed for referrals to take place. Allowing patients to seek out reimbursable DSMES on their own if they had not received it in the past might reduce this barrier. In addition, the Centers for Medicare & Medicaid Services restricts locations where in-person DSMES may be offered, requiring that for DSMES to be billable, it must take place in a medical setting such as a hospital outpatient department or private clinical practice. The only allowable community location is a pharmacy. Permitting the use of other spaces for DSMES, such as schools, libraries, or faith-based organizations, would expand options for rural communities that lack health care facilities.
Certified online DSMES could ameliorate the lack of local, in-person education programs. However, we found that broadband access was lower in counties with high diabetes prevalence than in other counties, and broadband access has consistently been lower in rural areas (32,33). The Bipartisan Infrastructure Law, which allocated $65 billion to extending internet access nationally, provided funding both for installation of broadband technology in unserved communities and for subsidies to allow low-income households to pay for services (34). As of this writing, however, the $30 per month broadband subsidy for low-income households has not been renewed, raising concerns that improvements in broadband access will be reversed (35). In addition, although the proportion of households lacking broadband will probably decline over the next decade, public health planners will still have to address the issues of health and internet literacy among populations learning to use these tools.
When DSMES is available locally, it may not be within financial reach of all patients. Although Medicare and Medicaid, as well as private insurers in nearly all states, treat DSMES as a reimbursable service, they do not waive patient financial responsibility. Low-income and uninsured people are less likely to report having had DSMES than their counterparts, suggesting that cost may be a barrier (15). Similarly, uptake of DSMES among Medicare fee-for-service beneficiaries is not optimal (36). The federal government has moved to cap the cost of insulin for Medicare beneficiaries (37), with possible spillover effects on private insurers (38). Similar initiatives or targeted subsidies could address reducing the cost of DSMES for patients. Incentives might also be needed to prompt clinicians to offer this low-revenue service. These relatively low-cost investments in DSMES may be an effective strategy in the long run for reducing the prevalence of ESRD.
Limitations
Our study had several limitations. First, it was ecological, examining counties. Relatedly, the county measure may include a small number of facilities incorrectly assigned by the US Department of Housing and Urban Development’s Zip Code Crosswalk Files (18). Second, our measure of need, diabetes prevalence among adults, is based on model-based estimates and thus subject to any limitations present in the modeling process. Third, we may not have captured all diabetes education. Although insurers will pay only for DSMES provided by certified programs, organizations may elect to offer diabetes education informally. However, the extent to which providers offer services that cannot be billed is likely to be low; in addition, the quality of such education could not be documented. CDC recommends that DSMES providers become certified (39). Next, our analysis did not include Indian Health Service DSMES programs unless they were CMS certified. The Indian Health Service both promotes diabetes education and supports the Special Diabetes Program for Indians, which reported 301 sites in 2020 (40). Finally, although the benefits of DSMES participation have been documented, whether geographic availability of DSMES is linked to patient participation or overall health outcomes is unknown.
Conclusion
We recommend that state and local public health departments assess the availability of DSMES in their service areas to determine whether the needs of people with diabetes are adequately addressed. Expanding the availability of DSMES is essential for reducing the adverse sequelae of this disease. Three options may improve access to DSMES: prompting additional providers to offer the service, expanded availability of online DSMES, and reducing associated patient costs, regardless of mode. Improved access could reduce both the immediate and long-term health effects and costs of diabetes and the incidence of ESRD, both for patients and for the health care system as a whole.
Acknowledgments
This project was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant number no. U1CRH45498, Rural Health Research Grant Program Cooperative Agreement. Tables detailing diabetes prevalence and availability of DSMES and dialysis for 3,141 US counties are available from the corresponding author. The information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the US government. The authors declared no potential conflicts of interest with respect to the research, authorship, or publication of this article and received no additional external financial support for its research, authorship, or publication. No copyrighted material, surveys, instruments, or tools were used in this article.
Author Information
Corresponding Author: Janice C. Probst, PhD, Rural and Minority Health Research Center, retired, Arnold School of Public Health, University of South Carolina, 220 Stoneridge Drive, Suite 204, Columbia, SC 29210 (Probst.rural@gmail.com).
Author Affiliations: 1Rural and Minority Health Research Center, Arnold School of Public Health, University of South Carolina, Columbia. 2Department of Public Health, Baylor University, Waco, Texas. 3Department of Public Health, A.T. Still University College of Graduate Health Studies, Kirksville, Missouri. 4College of Social Work, University of South Carolina, Columbia. 5College of Nursing, University of South Carolina, Columbia. 6Department of Health Management and Policy, RUPRI Center for Rural Health Policy Analysis, University of Iowa, Iowa City.
References
- National Institute of Diabetes and Digesting and Kidney Disease. Preventing diabetes problems. Accessed February 9, 2024. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems
- Centers for Disease Control and Prevention. National diabetes statistics report. Accessed February 9, 2024. https://www.cdc.gov/diabetes/php/data-research/?CDC_AAref_Val=https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Parker ED, Lin J, Mahoney T, Ume N, Yang G, Gabbay RA, et al. . Economic costs of diabetes in the US in 2022. Diabetes Care. 2024;47(1):26–43. PubMed doi:10.2337/dci23-0085
- Curtin SC, Tejada-Vera B, Bastian BA. Deaths: leading causes for 2020. Natl Vital Stat Rep. 2023;72(13):1–115. PubMed
- Burrows NR, Hora I, Geiss LS, Gregg EW, Albright A. Incidence of end-stage renal disease attributed to diabetes among persons with diagnosed diabetes — United States and Puerto Rico, 2000–2014. MMWR Morb Mortal Wkly Rep. 2017;66(43):1165–1170. PubMed doi:10.15585/mmwr.mm6643a2
- Zheng L, Chen X, Luo T, Ran X, Hu J, Cheng Q, et al. . Early-onset type 2 diabetes as a risk factor for end-stage renal disease in patients with diabetic kidney disease. Prev Chronic Dis. 2020;17:E50. PubMed doi:10.5888/pcd17.200076
- Nordheim E, Geir Jenssen T. Chronic kidney disease in patients with diabetes mellitus. Endocr Connect. 2021;10(5):R151–R159. PubMed doi:10.1530/EC-21-0097
- United States Renal Data System, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. 2023 Annual Data Report. 2023. Accessed May 6, 2024. https://usrds-adr.niddk.nih.gov/2023
- Matthews M, Reid J, McKeaveney C, Noble H. Knowledge requirements and unmet needs of informal caregivers of patients with end-stage kidney disease (ESKD) receiving haemodialysis: a narrative review. Healthcare (Basel). 2021;10(1):57. PubMed doi:10.3390/healthcare10010057
- Davis J, Fischl AH, Beck J, Browning L, Carter A, Condon JE, et al. . 2022 National Standards for Diabetes Self-Management Education and Support. Diabetes Care. 2022;45(2):484–494. PubMed doi:10.2337/dc21-2396
- Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. . Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, The Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Educ. 2020;46(4):350–369. PubMed doi:10.1177/0145721720930959
- Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926–943. PubMed doi:10.1016/j.pec.2015.11.003
- He X, Li J, Wang B, Yao Q, Li L, Song R, et al. . Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine. 2017;55(3):712–731. PubMed doi:10.1007/s12020-016-1168-2
- The Policy Surveillance Program. Temple University. Health insurance coverage laws for diabetes self management education and training. Accessed December 30, 2023. https://lawatlas.org/datasets/diabetes-self-management-education-laws
- Adjei Boakye E, Varble A, Rojek R, Peavler O, Trainer AK, Osazuwa-Peters N, et al. . Sociodemographic factors associated with engagement in diabetes self-management education among people with diabetes in the United States. Public Health Rep. 2018;133(6):685–691. PubMed doi:10.1177/0033354918794935
- Rutledge SA, Masalovich S, Blacher RJ, Saunders MM. Diabetes Self-Management Education programs in nonmetropolitan counties — United States, 2016. MMWR Surveill Summ. 2017;66(10):1–6. PubMed doi:10.15585/mmwr.ss6610a1
- US Department of Housing and Urban Development. HUD USPS ZIP Code Crosswalk Files. Accessed September 15, 2022. https://www.huduser.gov/portal/datasets/usps_crosswalk.html
- Wilson R, Din A. Understanding and enhancing the U.S. Department of Housing and Urban Development’s Zip Code Crosswalk Files. Cityscape (Wash, DC). 2018;20(2):277–294. Accessed June 7, 2024. https://www.huduser.gov/portal/periodicals/cityscpe/vol20num2/Cityscape-July_2018.pdf
- Centers for Medicare & Medicaid Services. Dialysis facilities archived data snapshots. Accessed Jan 4, 2023. https://data.cms.gov/provider-data/archived-data/dialysis-facilities
- 9 CFR Title 42 PART 494 – Conditions For Coverage For End-Stage Renal Disease Facilities Subpart D § 494.140(a). Federal Register, April 15, 2008. https://www.cms.gov/regulations-and-guidance/legislation/cfcsandcops/downloads/esrdfinalrule0415.pdf
- Centers for Disease Control and Prevention. PLACES: Local Data for Better Health. 2021 release. Accessed May 30, 2022. https://www.cdc.gov/places/help/explore-data-portal/index.html
- Bureau of Health Workforce, Health Resources and Services Administration, USDHHS. What is shortage designation? Accessed April 12, 2024. https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation
- University of Wisconsin Population Health Institute. County Health Rankings & Roadmaps 2022. Accessed May 30, 2022. www.countyhealthrankings.org
- US Department of Agriculture, Economic Research Service. County-level data sets. 2023. Accessed March 1, 2023. https://www.ers.usda.gov/data-products/county-level-data-sets/
- Hart JT. The inverse care law. Lancet. 1971;1(7696):405–412. PubMed doi:10.1016/S0140-6736(71)92410-X
- James J. Nonprofit hospitals’ community benefit requirements. Health Policy Brief, Health Affairs. February 25, 2016. Accessed February 6, 2024. https://www.healthaffairs.org/do/10.1377/hpb20160225.954803/
- Rettig RA. Origins of the Medicare kidney disease entitlement: the Social Security amendments of 1972. In Hanna KI, Editor, Biomedical Politics. National Academy Press; 1991.
- Gaffney A, Woolhandler S, Himmelstein DU. Century-long trends in the financing and ownership of American health care. Milbank Q. 2023;101(2):325–348. PubMed doi:10.1111/1468-0009.12647
- Association of Certified Diabetes Educators. DSMES reimbursement and affordable care. 2022. Accessed December 6, 2023. https://www.adces.org/practice/dsmes-insurance-reimbursement/
- National Diabetes Prevention Program. Engaging federally qualified health centers. Accessed February 12, 2024. https://coveragetoolkit.org/engaging-fqhcs/
- Centers for Disease Control and Prevention. DSMES Toolkit. Accessed April 12, 2024. https://www.cdc.gov/diabetes-toolkit/php/?CDC_AAref_Val=https://www.cdc.gov/diabetes/dsmes-toolkit/index.html
- Negaro SND, Hantman RM, Probst JC, Crouch EL, Odahowski CL, Andrews CM, et al. . Geographic variations in driving time to US mental health care, digital access to technology, and household crowdedness. Health Aff Sch. 2023;1(6):qxad070. PubMed doi:10.1093/haschl/qxad070
- Vogels EA. Some digital divides persist between rural, urban and suburban America. Pew Research Center, August 19, 2021. Accessed Jun 14, 2023. https://www.pewresearch.org/short-reads/2021/08/19/some-digital-divides-persist-between-rural-urban-and-suburban-america/
- US Department of Agriculture. Biden–Harris administration announces $401 million for high-speed internet access in rural areas. July 29, 2022. Accessed June 14, 2023. https://www.usda.gov/media/press-releases/2022/07/28/biden-harris-administration-announces-401-million-high-speed
- Levin B. The end of the Affordable Connectivity Program is almost here, threatening to widen the digital divide. Accessed April 12, 2024. Brookings Institute, February 13, 2024. https://www.brookings.edu/articles/the-end-of-the-affordable-connectivity-program-is-almost-here-threatening-to-widen-the-digital-divide/
- Rhudy C, Schadler A, Talbert JC. Rural/urban disparities in utilization of diabetes self-management training to the fee-for-service Medicare population. 2020. Rural & Underserved Health Research Center Publications. Accessed February 23, 2024. https://uknowledge.uky.edu/ruhrc_reports/11
- Centers for Medicare & Medicaid Services. 5 Things to know about Medicare insulin costs. CMS Product No. 12172, July 2023. Accessed January 10, 2024. https://www.cms.gov/files/document/5-things-medicare-insulin-costs.pdf
- Sparrow A. Lessons From Recent Efforts To Cap The Price Of Insulin. Health Affairs Forefront, September 26, 2023; Accessed December 30, 2023. https://www.healthaffairs.org/content/forefront/lessons-recent-efforts-cap-price-insulin
- Centers for Disease Control and Prevention. Become an Accredited or Recognized DSMES Provider Accessed Feb 24, 2023. https://www.cdc.gov/diabetes-toolkit/php/become-provider/?CDC_AAref_Val=https://www.cdc.gov/diabetes/dsmes-toolkit/accreditation-recognition/index.html
- Indian Health Service. Special diabetes program for Indians. SDPI Report to Congress. 2020 Accessed March 30, 2023. https://www.ihs.gov/sdpi/reports-to-congress/
Tables
| Characteristic | Total, n (%) | High estimated diabetes prevalence, n (%) | Low estimated diabetes prevalence, n (%) | P valuec |
|---|---|---|---|---|
| All counties | 3,141 (100.0) | 790 (25.2) | 2,351 (74.9) | NA |
| Service availability, % | ||||
| DSMES | 1,289 (41.0) | 164 (12.7) | 1,125 (87.3) | <.001 |
| Dialysis | 1,860 (59.2) | 417 (22.4) | 1,443 (77.6) | |
| Rurality, % | ||||
| Urban | 1,166 (37.1) | 150 (12.7) | 1,016 (87.1) | <.001 |
| Rural (all) | 1,975 (62.9) | 640 (32.4) | 1,335 (67.6) | |
| Rural micropolitan | 641 (20.4) | 147 (22.9) | 494 (77.1) | |
| Rural noncore | 1,334 (42.5) | 493 (37.0) | 841 (63.0) | |
| Census region, % | ||||
| Northeast | 217 (6.9) | 2 (0.9) | 215 (99.1) | <.001 |
| Midwest | 1,055 (33.6) | 69 (6.5) | 986 (93.5) | |
| South | 1,422 (45.3) | 675 (47.5) | 747 (52.5) | |
| West | 447 (14.2) | 44 (9.9) | 403 (90.2) | |
| Counties having HPSA status or health care resource, % | ||||
| Whole county HPSA status | 23.2 | 40.1 | 17.4 | <.001 |
| FQHC | 65.5 | 77.3 | 61.6 | <.001 |
| RHC | 74.2 | 86.5 | 70.1 | <.001 |
Abbreviations: DSMES, diabetes self-management education and support; FQHC, federally qualified health center; HPSA, health professional shortage area; RHC, rural health center.
a The PLACES data set does not include information for 2 county equivalents in Alaska, the Chugach Census Area and the Copper River Census Area.
b High prevalence = ≥14.4%; low prevalence = ≤14.3%.
c Calculated by using χ2 or Fisher Exact Test, as appropriate.
| Characteristic | Total, median | High estimated diabetes prevalence (n = 790) | Low estimated diabetes (n = 2,351) | P valuec |
|---|---|---|---|---|
| Total county population | ||||
| Median number of residents | 25,658 | 16,714 | 33,825 | <.001 |
| Demographic characteristic, percentage of population | ||||
| Race or ethnicity | ||||
| Asian/Pacific Islander | 0.9 | 0.6 | 1.0 | <.001 |
| Hispanic | 4.7 | 3.6 | 5.0 | <.001 |
| Non-Hispanic American Indian/Alaska Native | 0.7 | 0.6 | 0.7 | .04 |
| Non-Hispanic Black | 2.3 | 9.7 | 1.8 | <.001 |
| Non-Hispanic White | 82.8 | 62.6 | 85.6 | <.001 |
| Age, ≥65 y | 19.8 | 20.8 | 19.5 | <.001 |
| Resources, median percentage | ||||
| Population <18 y with income below federal poverty level | 17.6 | 27.5 | 15.1 | <.001 |
| Uninsured adults aged 18–64 y | 12.8 | 17.3 | 11.5 | <.001 |
| Unemployment among people in the workforce aged ≥16 y | 6.5 | 7.3 | 6.3 | <.001 |
| Education, high school (% 9th graders who graduated in 4 years) | 88.8 | 82.6 | 90.4 | <.001 |
| Not English fluent | 0.7 | 0.6 | 0.8 | <.001 |
| Broadband access (household) | 79.6 | 71.4 | 81.6 | <.001 |
a The PLACES data set does not include information for 2 county equivalents in Alaska, the Chugach Census Area and the Copper River Census Area.
b High prevalence = ≥14.4%; low prevalence = ≤14.3%. Counties are sorted by prevalence of diabetes among adults, but characteristics pertain to the whole population.
c Calculated by Mann–Whitney test.
| Characteristic | Total | Resource combinations within the county | ||||
|---|---|---|---|---|---|---|
| DSMES & dialysis, n (%) | DSMES only, n (%) | Dialysis only, n (%) | Neither resource, n (%) | P valueb | ||
| All counties | 3,141 | 1,085 (34.5) | 204 (6.5) | 775 (24.7) | 1,077 (34.3) | NA |
| Diabetes prevalence | ||||||
| Top quartile (≥14.4%) | 790 | 129 (16.3) | 35 (4.4) | 288 (36.5) | 338 (42.8) | <.001 |
| Bottom 3 quartiles (≤14.3%) | 2,351 | 956 (40.7) | 169 (7.2) | 487 (20.7) | 739 (31.4) | |
| Rurality | ||||||
| Urban | 1,166 | 663 (56.9) | 32 (2.7) | 266 (22.8) | 205 (17.6) | <.001 |
| Rural (all) | 1,975 | 422 (21.4) | 172 (8.7) | 509 (25.8) | 872 (44.1) | |
| Rural micropolitan | 641 | 281 (43.8) | 29 (4.5) | 235 (36.7) | 96 (15.0) | |
| Rural noncore | 1,334 | 141 (10.6) | 143 (10.7) | 274 (20.5) | 776 (58.2) | |
| Census region | ||||||
| Northeast | 217 | 146 (67.3) | 8 (3.7) | 44 (20.3) | 19 (8.8) | <.001 |
| Midwest | 1,055 | 362 (34.3) | 110 (10.4) | 181 (17.2) | 402 (38.1) | |
| South | 1,422 | 421 (29.6) | 48 (3.4) | 483 (34.0) | 470 (33.1) | |
| West | 447 | 156 (34.9) | 38 (8.5) | 67 (15.0) | 186 (41.6) | |
| Health care resources | ||||||
| Whole County HPSA | ||||||
| Yes | 727 | 56 (7.7) | 42 (5.8) | 187 (25.7) | 442 (60.8) | <.001 |
| No | 2,414 | 1,029 (42.6) | 162 (6.7) | 588 (24.4) | 635 (26.3) | |
| FQHC in county | ||||||
| Yes | 2,058 | 889 (43.2) | 89 (4.3) | 562 (27.3) | 518 (25.2) | <.001 |
| No | 1,083 | 196 (18.1) | 115 (10.6) | 213 (19.7) | 559 (51.6) | |
| RHC in county | ||||||
| Yes | NA | 638 (27.4) | 172 (7.4) | 623 (26.7) | 899 (38.6) | <.001 |
| No | NA | 447 (55.3) | 32 (4.0) | 152 (18.80) | 178 (22.0) | |
| Hospital in county | ||||||
| Yes | 2,466 | 1,067 (43.3) | 180 (7.3) | 667 (27.1) | 552 (22.4) | <.001 |
| No | 675 | 18 (2.7) | 24 (3.6) | 108 (16.0) | 525 (77.8) | |
Abbreviations: DSMES, diabetes self-management education and support; FQHC, federally qualified health center; HPSA, Health Professional Shortage Area; NA, not applicable; RHC, rural health clinic.
a The PLACES data set does not include information for 2 county equivalents in Alaska, the Chugach Census Area and the Copper River Census Area.
b Calculated by χ2 or Fisher Exact Test, as appropriate.
| Availability | Total | Type of health care service | ||||
|---|---|---|---|---|---|---|
| Both hospital & FQHC, n (%) | FQHC only, n (%) | Hospital only, n (%) | Neither, n (%) | P valueb | ||
| Counties health care services | 3,141 | 1,655 (52.7) | 403 (12.8) | 811 (25.8) | 272 (8.7) | NA |
| DSMES in county | ||||||
| Yes | 1,289 | 945 (57.1) | 33 (8.2) | 302 (37.2) | 9 (3.3) | <.001 |
| No | 1,852 | 710 (42.9) | 370 (91.8) | 509 (62.8) | 263 (96.7) | |
Abbreviations: DSMES, diabetes self-management education services; FQHC, federally qualified health center.
a The PLACES data set does not include information for 2 county equivalents in Alaska, the Chugach Census Area and the Copper River Census Area.
b Calculated by χ2.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.