What to know
- Global measles activity is increasing.
- U.S. measles-mumps-rubella (MMR) coverage among kindergarteners is below the 95 percent coverage target—much lower in some communities—and is decreasing.
- CDC is creating models to show how measles outbreaks could occur and spread in the U.S.
Summary
What CDC knows
Worldwide, measles cases and outbreaks are on the rise, and U.S. measles-mumps-rubella (MMR) vaccination coverage has been decreasing since the start of the COVID-19 pandemic. For some communities, it has fallen below the 95 percent coverage level needed to prevent measles outbreaks. Some communities in the U.S. have even lower MMR vaccination coverage, putting them at high risk for a measles outbreak.
What CDC is doing
In addition to providing clinical guidance to healthcare providers and technical and communications support and vaccines to health departments, CDC is monitoring the measles situation globally and creating models of how measles could spread in the U.S. These models can be used to help federal, state, local, tribal and territorial health departments prepare for possible measles cases, better understand how to identify communities at highest risk, and manage healthcare resources.
Background
Measles is an extremely infectious and potentially severe rash illness that was very common among children before the measles-mumps-rubella (MMR) vaccine was introduced in 1971. Measles was declared eliminated in the U.S. in 2000, due to high levels of vaccination with the safe and effective MMR vaccine. This year, the U.S. is at greater risk for measles outbreaks because decreased vaccination worldwide has led to more cases internationally. People who are not vaccinated may encounter measles when traveling abroad and return to the U.S. with measles. Additionally, declining U.S. vaccination rates increases susceptibility to outbreaks.
It's important to remember that the overall measles outbreak risk to the general population is low; however, measles cases are increasing globally, increasing the chance of importations into the U.S. and subsequent risk of outbreaks, particularly in communities with low vaccination rates. Below, we describe measles epidemiology, including factors that determine who is likely to get measles, and how big outbreaks could get. We also describe how we are using modeling to explore potential scenarios and to better understand future measles outbreak risk in the United States. Modeling is also used to help highlight recommended preparedness actions for individuals and public health practitioners in state, local, tribal, and territorial health departments.
What is measles, and why are we talking about it right now?
Measles is an extremely infectious and potentially severe rash illness. Measles was declared eliminated in the U.S. in 2000, thanks to a very high percentage of people receiving the safe and effective measles-mumps-rubella (MMR) vaccine.
Before the measles vaccine was introduced, nearly everyone was infected with the measles virus by the time they were 15 years old. It is estimated that 3 to 4 million people in the U.S. were infected, 400—500 people died, 48,000 were hospitalized, and 1,000 suffered encephalitis (swelling of the brain) each year.
U.S. measles outbreak risk depends on two main factors:
- Global measles activity: More cases of measles occurring globally means more chances for importation to the U.S.
- U.S. population susceptibility to measles virus: Since the COVID-19 pandemic, MMR coverage among kindergarteners slipped below the 95% vaccination coverage target for the U.S. to 93%. About 250,000 kindergarteners were not up to date on their MMR vaccines each year since the 2020-2021 school year.

What factors determine measles outbreak likelihood and size?
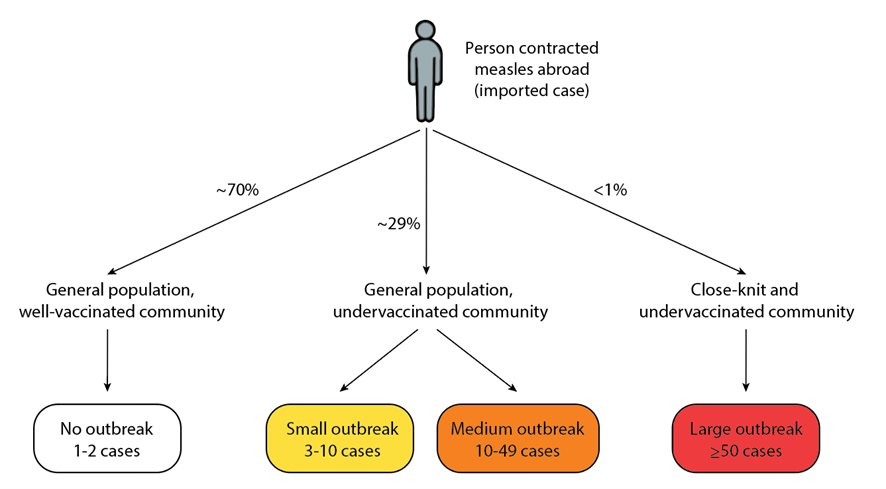
In the U.S., measles outbreaks generally fall into three broad categories of size, based on the susceptibility of those exposed to an imported case of measles:
- No outbreak: If a person infected with measles abroad returns to the U.S. and arrives in the general population in a well-vaccinated setting, this usually does not result in transmission to others and an outbreak. From 2001-2023, 70% of international measles importations did not lead to outbreaks.
- Small to medium outbreak: If a person who acquired measles abroad returns to an undervaccinated setting in the general population, a small- to medium-sized outbreak is likely. The size of the outbreak depends on the strength of public health response, density of the exposure setting, and chance events, such as where the measles exposures occurred and how many unvaccinated individuals were exposed.
- Large outbreak: If a person who acquired measles abroad returns to a close-knit and under vaccinated community with high population density, a large outbreak is likely. From 2001-2023, 88% of outbreaks larger than 50 cases have occurred within these settings.
How does this epidemiologic context inform modeling efforts?
We see from the epidemiologic data that measles outbreaks mostly occur in close-knit and under vaccinated communities. As shown in Figure 3, two populations can have the same vaccination coverage on average, when individuals who are not vaccinated are spread throughout the community, the risk of an outbreak is low. However, if unvaccinated individuals are clustered, the risk of an outbreak within that group of closely associated unvaccinated individuals is high.

How do we model potential measles outbreaks?
CDC’s Center for Forecasting and Analytics (CFA), together with the Division of Viral Diseases (DVD) in the National Center for Immunization and Respiratory Diseases (NCIRD), have been analyzing measles data and creating models to explore potential scenarios and help us better understand measles outbreak risk in the U.S.
How many measles outbreaks might we see in 2024?
By looking at historical data on measles outbreaks, outbreak size, and their distribution since 2001, we anticipate the most likely number of cases in 2024 is around 300, and we estimate there is a 4% chance of >1000 measles cases reported in 2024. Our analysis indicates the number of outbreaks in 2024 is unlikely to be substantially greater than the number of outbreaks in prior years such as 2011, 2014, 2018, and 2019.

How could changing MMR coverage impact the risk of measles outbreaks for schoolchildren?
As vaccination coverage has declined among kindergarteners—with about 250,000 children each year not fully vaccinated against MMR by kindergarten entry since the COVID-19 pandemic began—we analyze how this might affect outbreak risk.
We explore how vaccination coverage affects outbreak risk in a hypothetical school population. We know vaccination coverage can vary widely in schools based on the number of children with medical or non-medical vaccine exemptions.
Fact
This puts children who are unvaccinated for medical reasons—and household members who are immune-compromised or babies who are too young to be vaccinated—at risk of measles and its complications. This can also create a substantial public health response burden, including strain on medical facilities, doctors, nurses, and health departments.
Table 1 below shows an example of a school with 100 children and 1 infectious child, at different levels of MMR coverage. The model, a simplified version of the model used in this paper, assumes that the child with measles goes to school while infectious and there is no vaccination intervention.
| MMR Coverage | # children susceptible | Chance of an outbreak |
|---|---|---|
| 97% | 6 | 16% |
| 95% | 8 | 29% |
| 93% | 10 | 36% |
| 90% | 13 | 51% |
| 85% | 18 | 61% |
| 80% | 22 | 64% |
| 70% | 32 | 78% |
This example illustrates the following conclusions:
- As vaccination coverage declines, the chance of an outbreak increases. Once we decline to 85% MMR coverage and below, an outbreak is likely to occur if a child with measles comes to school while infectious.
- Even at 97% coverage, there is some chance of an outbreak occurring if a child with measles comes to school while infectious. This highlights that while the measles vaccine is very effective, measles is extremely infectious and unvaccinated children remain at risk for measles infection. The best protection against measles is to get vaccinated.
Actions for the Public
- The MMR vaccine is very safe and effective. Two doses of MMR vaccine provide better protection against measles than one dose: two doses of MMR vaccine are about 97% effective at preventing measles; one dose is about 93% effective.
- Measles is extremely infectious and can cause life-threatening illness. Anyone who is not protected against measles is at risk. An unvaccinated person can get measles when traveling abroad or in the U.S. Vaccination also protects those too young for their first measles vaccine or those with medical conditions that are unable to be immunized.
- Parents should get their children vaccinated on schedule with MMR vaccine. Teens and adults should check with their doctors to make sure they are protected against measles.
- International travel: People 6 months and older should be protected against measles before leaving for international trips. Infants under 12 months old who are traveling internationally should get an early dose at 6 through 11 months, then follow the recommended schedule for doses 1 and 2. People 12 months and older should receive 2 doses before travel. Watch your health for 3 weeks after you return. If you or your child gets sick with a rash and fever, call your healthcare provider.
- Possible exposure: If you think that you have measles or have been exposed to someone with measles, isolate yourself from others and call your healthcare provider, urgent care, or emergency room before arriving to be tested. Do not arrive at a healthcare facility without giving advance notice.
