Key points
- Suspected cases of measles must be laboratory confirmed.
- People without presumptive evidence of immunity should be vaccinated or revaccinated.
- Please contact your state or local health department to determine where to send specimens for testing.
Testing indications for measles in low prevalence settings
Ongoing measles activity in other countries will result in sporadic cases of measles in the United States. Evaluation and interpretation of measles diagnostic results can be complex, particularly in measles elimination settings.
Timing of specimen collection
Detection of specific IgM antibodies in a serum specimens collected within the first few days of rash onset can provide presumptive evidence of a current or recent measles virus infection.
Testing limitations
Because no assay is 100% specific, serologic testing of non-measles cases using any assay will occasionally produce false positive IgM results. Serologic tests can also result in false-negative results when serum specimens are collected too early with respect to rash onset.
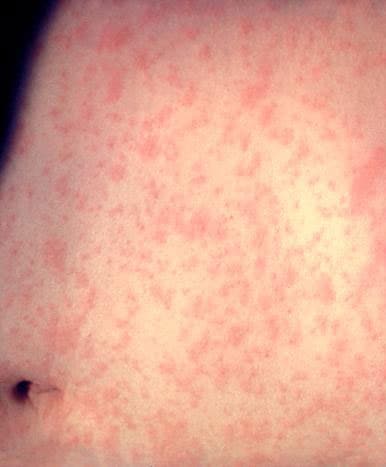
In countries such as the United States where endemic circulation of measles has been eliminated, most suspected cases are not measles, and rash and fever are more likely due to a number of other rash–causing illnesses such as:
- Parvovirus B19
- Enteroviruses
- Human herpesvirus–6 (roseola)
The presence of rheumatoid factor (RF) can also result in a false positive IgM. Indirect enzyme immunoassays (EIAs) appear to be more affected by RF than IgM capture assays.
Patients with throat or ear infections occasionally develop a rash following administration of antibiotics. Subsequent serologic specimens sent for measles IgM testing may result in a false positive test.
Evidence of immunity
Laboratory evidence of immunity is based on testing to detect measles IgG.
People without presumptive evidence of immunity based on documented MMR doses who have negative or equivocal results for measles IgG should be vaccinated or revaccinated. In some cases, vaccination is not possible, and testing with a second line diagnostic assay may be necessary to determine the patient's immune status.
Commercial EIAs
CDC has evaluated the performance of several commercial EIAs used to detect measles IgG.1Some of the commercial, manually processed EIAs are slightly more sensitive than high-throughput automated IgG test platforms that are typically used by large commercial laboratories.
Contact CDC or the state public health laboratory for information on second line assays.
Instructions for blood collection
Blood for serologic testing of measles at CDC is collected as described in the Infectious Disease Laboratories Test Directory entry for each test, listed below:
Testing infants or small children
Blood for serologic testing of infants or small children can be collected by finger/heel stick.
Capillary tubes can be utilized for infants. Capillary tubes require the submitter to have access to a hematocrit centrifuge. Clinical laboratories should have 50 or 100 µL capillary tubes that are typically used for a variety of tests, such as hematocrits or total lipids on newborns. At least 3 of the 50 µL hematocrit capillary tubes should be collected and spun in a hematocrit centrifuge.
Submitting specimens to CDC
Contact health department first
Available tests
The following tests are available for laboratory confirmation of measles:
- A capture IgM EIA (non-quantitative) that incorporates a recombinant measles virus nucleocapsid protein as the antigen is used to detect measles IgM.
- A commercial, indirect EIA (non-quantitative) assay is used for detection of IgG.
- Viral detection methods include standard methods of culturing virus in appropriate cell lines and techniques, such as real time RT-PCR to detect measles viral RNA.
Support from CDC measles laboratory
During outbreaks of measles, the CDC measles laboratory can assist with testing for any suspected case of measles.
- To expedite confirmation of measles from highly suspicious cases (recent travel, classic measles signs and symptoms)—particularly in a setting with many potential exposures—the following can be sent to CDC while testing is underway at the state public health or local clinical laboratory:
- An aliquot of serum
- Nasopharyngeal or throat swab
- An aliquot of serum
- Direct requests for measles serologic testing that are strictly for rule-out purposes (low index of suspicion, does not meet clinical case definition, no travel or contact with cases) to either:
Prior communication with CDC's Viral Vaccine-Preventable Diseases Branch (VVPDB) regarding suspected cases of measles that require assistance is preferred.
Specimen submission form
A completed CDC Specimen Submission Form (50.34) must be submitted with each specimen with the following information provided:
- Patient identification number and/or name
- Patient date of birth
- Travel history
- Date(s) of MMR vaccination (if known)
- Clinical signs and symptoms
- Date of onset
- Date of specimen collection
- Any available preliminary results
Test turnaround-time for IgG and IgM serology
Serum specimens for measles serologic testing (IgG, IgM) are delivered by courier to the STATT (Specimen Triage and Tracking Team) laboratory at CDC and then delivered to the VVPDB measles lab (Unit #81).
The turnaround–time for testing specimens for IgM and IgG is 7 working days after the delivery of specimens to the measles reference lab by the STATT laboratory. When situations require immediate notification of a result, please inform the laboratory upon submission of the specimen. Contact Dr. Stephen Crooke 404-718-4003 or Dr. Paul Rota 404-639-4181. Provide a telephone number, email address, and fax number.
IgG avidity and PRN assays
IgG avidity testing and a plaque reduction neutralization (PRN) assay are available at CDC. They are used when case classification requires additional methods to confirm measles infection, usually when the result obtained for IgM is suspected of being a false negative or a false positive.2
These assays may be offered when confirmation by RT-PCR was not successful or a molecular specimen was not available.
Contact information
Avidity testing and the PRN assay require specialized reagents and their use is limited to unusual cases, typically in an outbreak setting, when cases with mild or a non-classic presentation of measles are detected. A single serum can be tested for IgG avidity; however, specimens must have detectable IgG.
Test turnaround-time for IgG avidity
The turnaround–time for testing specimens for IgG avidity is 30 working days after the delivery of the specimens to the measles reference lab by the STATT laboratory.
Both an acute and a convalescent phase serum are recommended for PRN testing. There is no established turnaround–time for measles PRN testing.
- Latner DR, Sowers SB, Anthony K, Colley H, Badeau C, Coates J, Wong P, Fakile Y, Interiano C, Pannell KB, Leung-Pineda V, Patel MM, Rota PA, Limbago BM, Hickman CJ. Qualitative Variation among Commercial Immunoassays for Detection of Measles-Specific IgG. J Clin Microbiol. 2020;58(6):e00265-20.
- Sowers SB, Rota JR, Hickman CJ, Mercader S, Redd S, McNall RJ, Williams N, McGrew M, Walls ML, Rota PA, and Bellini WJ. Diagnostic Laboratory Immunology: High Concentrations of Measles Neutralizing Antibodies and High-Avidity Measles IgG Accurately Identify Measles Reinfection Cases. Clin Vaccine Immunol. 2016;23(8):707-16.
- Cremer NE, Cossen CK, Shell G, Diggs J, Gallo D, and Schmidt NJ. Enzyme immunoassay vs plaque neutralization and other methods for determination of immune status to measles and varicella-zoster viruses and vs complement fixation for serodiagnosis of infections with those viruses. J Clin Microbiol. 1985;21:869-873.
- Erdman DD, Anderson LJ, Adams DR, Stewart JA, Markowitz LE, and Bellini WJ. Evaluation of monoclonal antibody-based capture enzyme immunoassays for detection of specific antibodies to measles virus. J Clin Microbiol. 1991;29:1466-1471.
- Hummel KB, Erdman DD, Heath J, and Bellini WJ. Baculovirus expression of the nucleoprotein gene of measles virus and utility of the recombinant protein in diagnostic enzyme immunoassays. J Clin Microbiol. 1992;30:2874-2880.
- Helfand RF, Heath JL, Anderson LJ, Maes EF, Guris D, and Bellini WJ. Diagnosis of measles with an IgM capture EIA: The optimal timing of specimen collection after rash onset. J Infect Dis. 1997;175:195-199.
- Ratnam S, Tipples G, Head C, Fauvel M, Fearon M, and Ward BJ. Performance of indirect immunoglobulin M (IgM) serology tests and IgM capture assays for laboratory diagnosis of measles. J Clin Microbiol. 2000;38:99-10.
- Hickman CJ, Sowers SB, Mercader S, McGrew M, Williams NJ, Beeler JA et al. Laboratory characterization of measles virus infection in previously vaccinated and unvaccinated individuals. J Infect Dis. 2011;204(Supplement 1):S549-558.
- Rota JR, Hickman CJ, Sowers SB, Rota PA, Mercader S, and Bellini WJ . Two case studies of modified measles in vaccinated physicians exposed to primary measles cases: High risk of infection but low risk of transmission. J Infect Dis. 2011;204(Supplement 1):S559-563.
- Cremer NE, Cossen CK, Shell G, Diggs J, Gallo D, and Schmidt NJ. Enzyme immunoassay vs plaque neutralization and other methods for determination of immune status to measles and varicella-zoster viruses and vs complement fixation for serodiagnosis of infections with those viruses. J Clin Microbiol. 1985;21:869-873.
- Erdman DD, Anderson LJ, Adams DR, Stewart JA, Markowitz LE, and Bellini WJ. Evaluation of monoclonal antibody-based capture enzyme immunoassays for detection of specific antibodies to measles virus. J Clin Microbiol. 1991;29:1466-1471.
- Hummel KB, Erdman DD, Heath J, and Bellini WJ. Baculovirus expression of the nucleoprotein gene of measles virus and utility of the recombinant protein in diagnostic enzyme immunoassays. J Clin Microbiol. 1992;30:2874-2880.
- Helfand RF, Heath JL, Anderson LJ, Maes EF, Guris D, and Bellini WJ. Diagnosis of measles with an IgM capture EIA: The optimal timing of specimen collection after rash onset.J Infect Dis. 1997;175:195-199.
- Ratnam S, Tipples G, Head C, Fauvel M, Fearon M, and Ward BJ. Performance of indirect immunoglobulin M (IgM) serology tests and IgM capture assays for laboratory diagnosis of measles. J Clin Microbiol. 2000;38:99-10.
- Hickman CJ, Sowers SB, Mercader S, McGrew M, Williams NJ, Beeler JA et al. Laboratory characterization of measles virus infection in previously vaccinated and unvaccinated individuals. J Infect Dis. 2011;204(Supplement 1):S549-558.
- Rota JR, Hickman CJ, Sowers SB, Rota PA, Mercader S, and Bellini WJ . Two case studies of modified measles in vaccinated physicians exposed to primary measles cases: High risk of infection but low risk of transmission.J Infect Dis. 2011;204(Supplement 1):S559-563.
