Key points
- How to implement personal protective equipment (PPE) use in nursing homes to prevent spread of multi-drug resistant organisms (MDROs).
For Awareness
Updates: Recommendations for Enhanced Barrier Precautions are being reviewed as part of updates to the 2007 Guideline for Isolation Precautions. Once a draft is finalized by the Healthcare Infection Control Practices Advisory Committee (HICPAC), it will be posted in the federal register for a public comment period before being returned to HICPAC for additional review. Further information about HICPAC, the guideline development and public comment process, and future meetings is available at: Healthcare Infection Control Practices Advisory Committee (HICPAC).
Updates as of July 12, 2022
Key Points:1
- Multidrug-resistant organism (MDRO) transmission is common in skilled nursing facilities, contributing to substantial resident morbidity and mortality and increased healthcare costs.
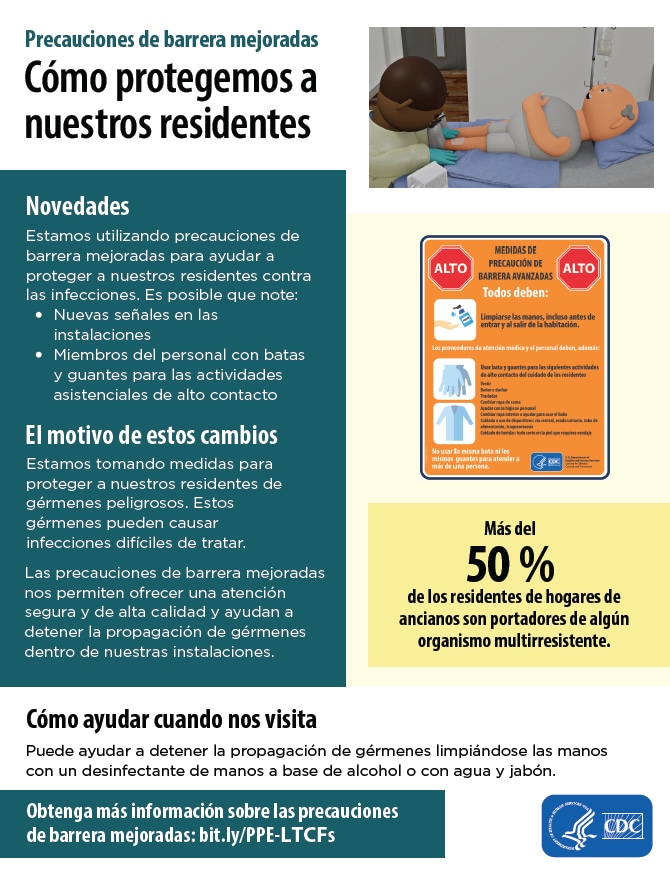
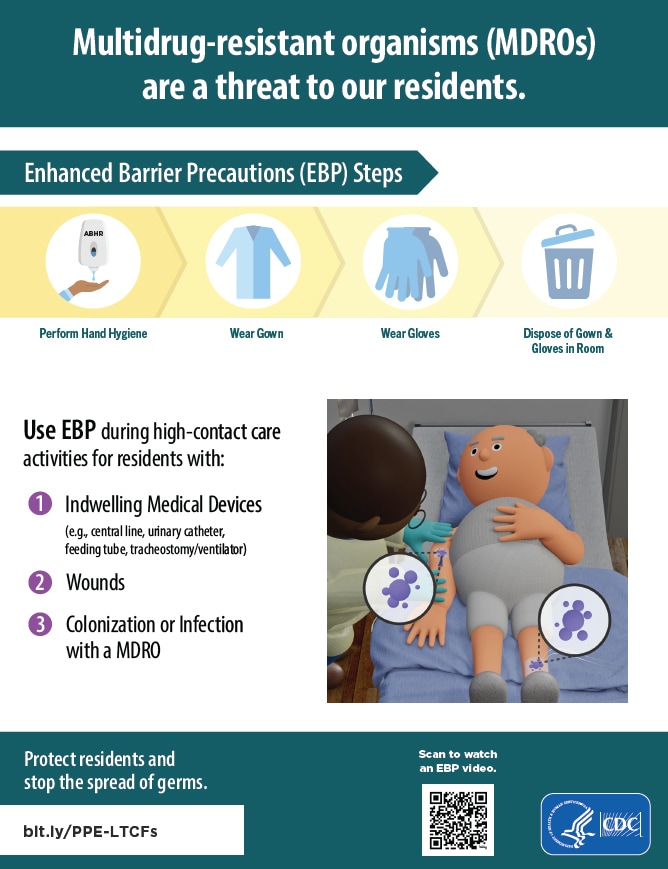
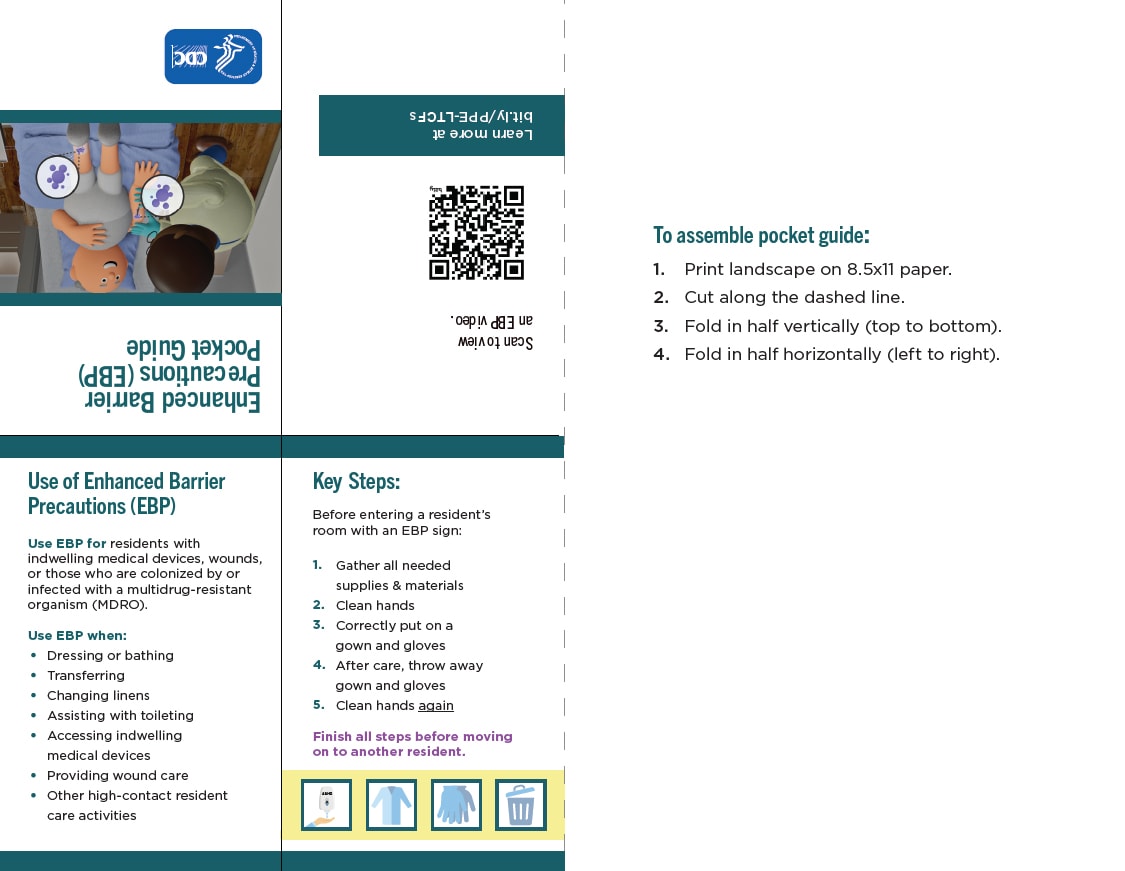
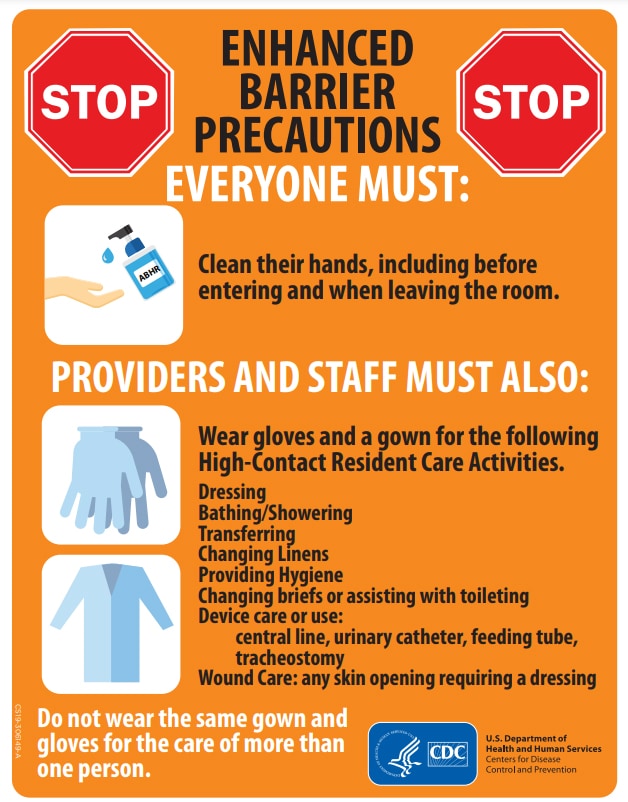
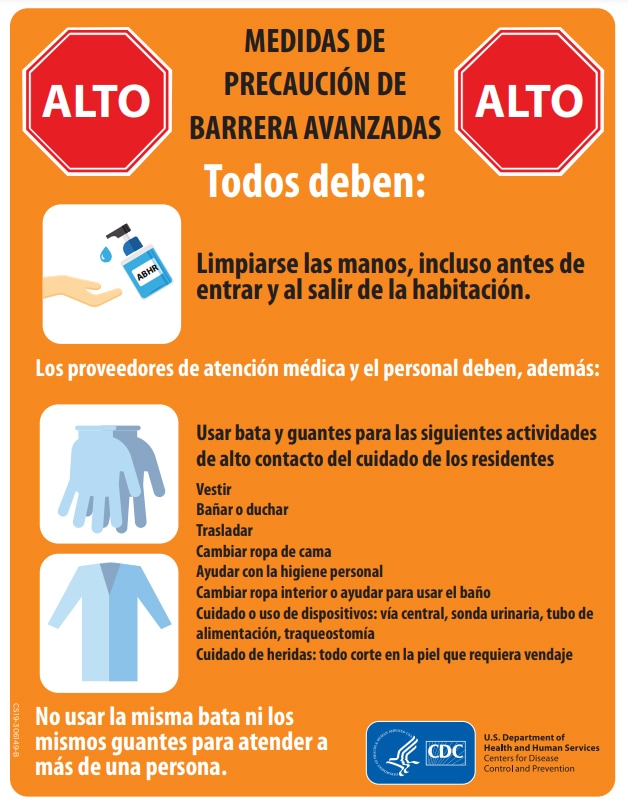
- Enhanced Barrier Precautions (EBP) are an infection control intervention designed to reduce transmission of resistant organisms that employs targeted gown and glove use during high contact resident care activities.
- EBP may be indicated (when Contact Precautions do not otherwise apply) for residents with any of the following:
- Wounds or indwelling medical devices, regardless of MDRO colonization status
- Infection or colonization with an MDRO.
- Wounds or indwelling medical devices, regardless of MDRO colonization status
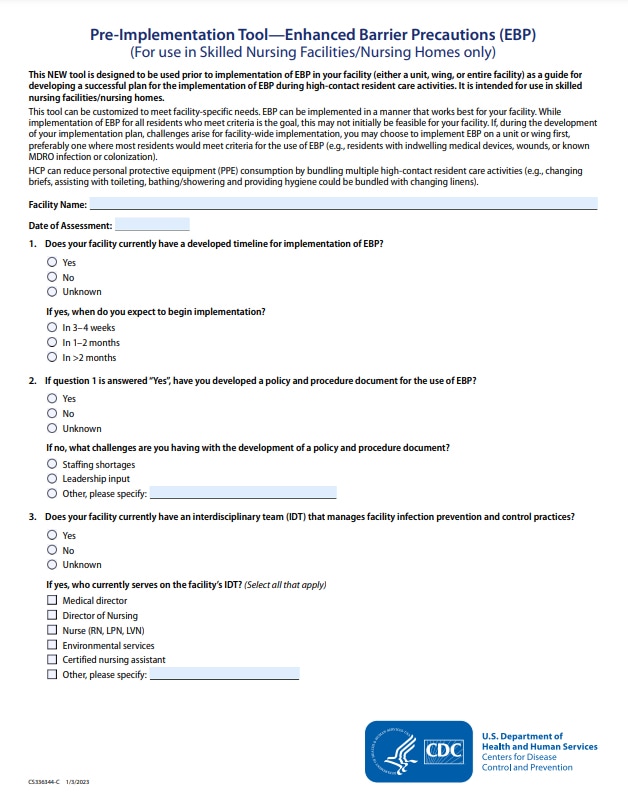
- Effective implementation of EBP requires staff training on the proper use of personal protective equipment (PPE) and the availability of PPE and hand hygiene supplies at the point of care.
- Standard Precautions, which are a group of infection prevention practices, continue to apply to the care of all residents, regardless of suspected or confirmed infection or colonization status.
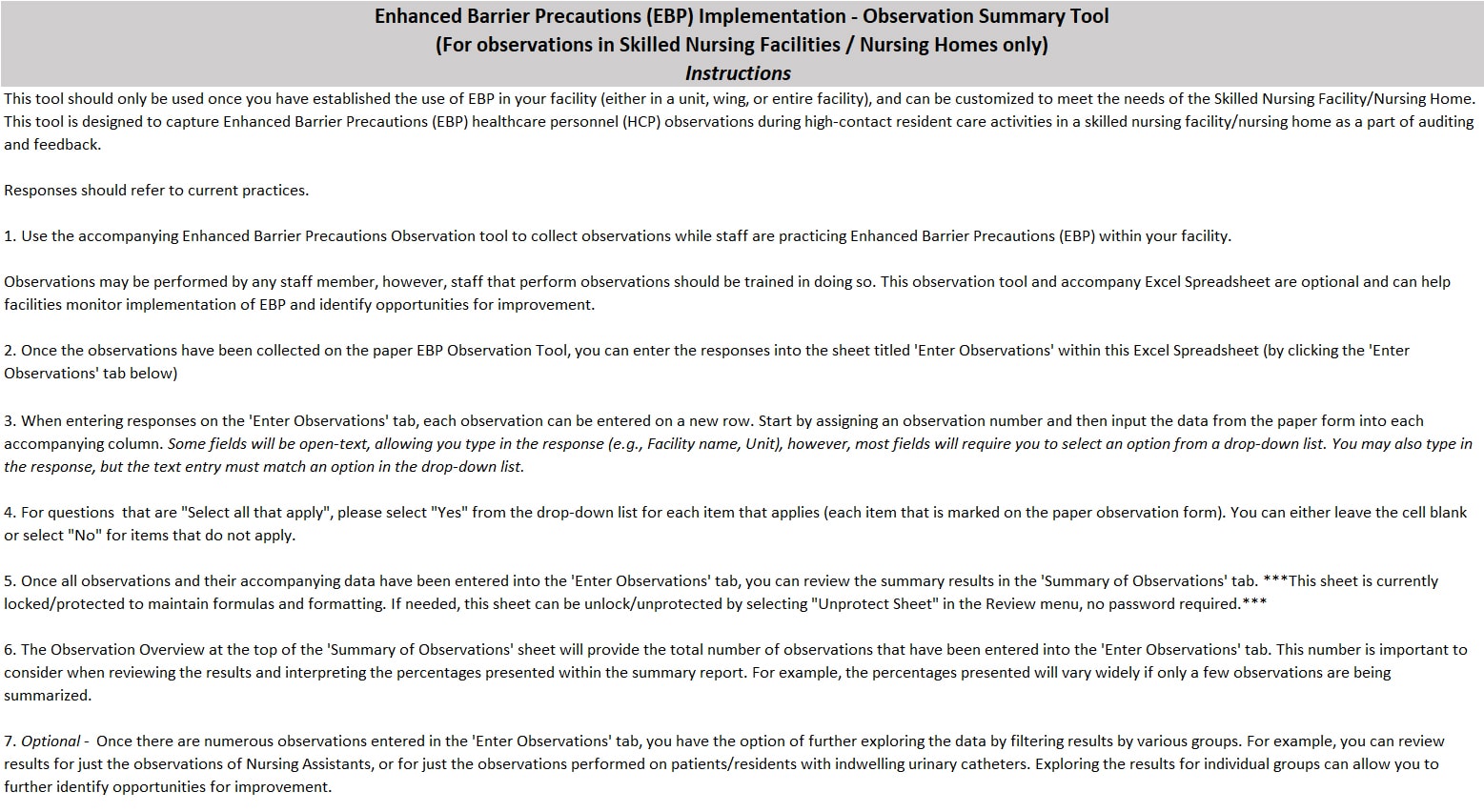
Enhanced Barrier Precautions in Nursing Homes - Video, Posters, Pocket Guide
Videos
Posters
Pocket guide
Background
Residents in nursing homes are at increased risk of becoming colonized and developing infection with MDROs2. As described further in Consideration for the Use of Enhanced Barrier Precautions in Skilled Nursing Facilities, more than 50% of nursing home residents may be colonized with an MDRO, nursing homes have been the setting for MDRO outbreaks, and when these MDROs result in resident infections, limited treatment options are available123456789. Implementation of Contact Precautions, as described in the CDC Guideline for Isolation Precautions, is perceived to create challenges for nursing homes trying to balance the use of PPE and room restriction to prevent MDRO transmission with residents' quality of life. Thus, many nursing homes only implement Contact Precautions when residents are infected with an MDRO and on treatment.
Focusing only on residents with active infection fails to address the continued risk of transmission from residents with MDRO colonization, who by definition have no symptoms of illness. MDRO colonization may persist for long periods of time (e.g., months) which contributes to the silent spread of MDROs.10
With the need for an effective response to the detection of serious antibiotic resistance threats, there is growing evidence that the traditional implementation of Contact Precautions in nursing homes is not implementable for most residents for prevention of MDRO transmission.
This document is intended to provide guidance for PPE use and room restriction in nursing homes for preventing transmission of MDROs, including as part of a public health response. For the purposes of this guidance, the MDROs for which the use of EBP applies are based on local epidemiology. At a minimum, they should include resistant organisms targeted by CDC but can also include other epidemiologically important MDROs910.
Examples of MDROs Targeted by CDC include:
- Pan-resistant organisms
- Carbapenemase-producing carbapenem-resistant Enterobacterales
- Carbapenemase-producing carbapenem-resistant Pseudomonas spp.
- Carbapenemase-producing carbapenem-resistant Acinetobacter baumannii
- Candida auris
Additional epidemiologically important MDROs may include, but are not limited to:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- ESBL-producing Enterobacterales
- Vancomycin-resistant Enterococci (VRE)
- Multidrug-resistant Pseudomonas aeruginosa
- Drug-resistant Streptococcus pneumoniae
This document is not intended for use in acute care or long-term acute care hospitals and does not replace existing guidance regarding use of Contact Precautions for other pathogens (e.g., Clostridioides difficile, norovirus) in nursing homes.
Description of Precautions
Standard Precautions
A group of infection prevention practices that apply to the care of all residents, regardless of suspected or confirmed infection or colonization status. They are based on the principle that all blood, body fluids, secretions, and excretions (except sweat) may contain transmissible infectious agents. Proper selection and use of PPE, such as gowns and gloves, is one component of Standard Precautions, along with hand hygiene, safe injection practices, respiratory hygiene and cough etiquette, environmental cleaning and disinfection, and reprocessing of reusable medical equipment. Use of PPE is based on the staff interaction with residents and the potential for exposure to blood, body fluids, or pathogens (e.g., gloves are worn when contact with blood, body fluids, mucous membranes, non-intact skin, or potentially contaminated surfaces or equipment are anticipated). More detail about Standard Precautions is available as part of the Core Infection Prevention and Control Practices for Safe Healthcare Delivery in all Settings.
Contact Precautions
One type of Transmission-Based Precaution that are used when pathogen transmission is not completely interrupted by Standard Precautions alone. Contact Precautions are intended to prevent transmission of infectious agents, like MDROs, that are spread by direct or indirect contact with the resident or the resident's environment.
Contact Precautions require the use of gown and gloves on every entry into a resident's room. The resident is given dedicated equipment (e.g., stethoscope and blood pressure cuff) and is placed into a private room. When private rooms are not available, some residents (e.g., residents with the same pathogen) may be cohorted, or grouped together. Residents on Contact Precautions should be restricted to their rooms except for medically necessary care and restricted from participation in group activities.
Because Contact Precautions require room restriction, they are generally intended to be time limited and, when implemented, should include a plan for discontinuation or de-escalation.
More detail about Transmission-Based Precautions, including descriptions of Droplet Precautions and Airborne Precautions are available in the CDC Guideline for Isolation Precautions. In addition, other infections (e.g. norovirus, C. difficile, and scabies) and conditions for which Contact Precautions are indicated are summarized in Appendix A – Type and Duration of Precautions Recommended for Selected Infections and Conditions of the guideline.
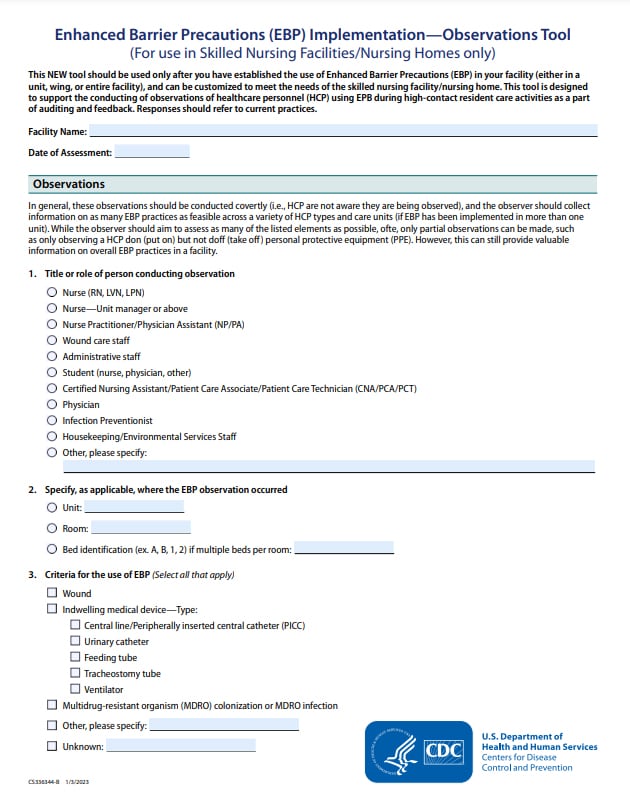
Enhanced Barrier Precautions
Expand the use of PPE and refer to the use of gown and gloves during high-contact resident care activities that provide opportunities for transfer of MDROs to staff hands and clothing1112131415. MDROs may be indirectly transferred from resident-to-resident during these high-contact care activities. Nursing home residents with wounds and indwelling medical devices are at especially high risk of both acquisition of and colonization with MDROs356. The use of gown and gloves for high-contact resident care activities is indicated, when Contact Precautions do not otherwise apply, for nursing home residents with wounds and/or indwelling medical devices regardless of MDRO colonization as well as for residents with MDRO infection or colonization.
Examples of high-contact resident care activities requiring gown and glove use for Enhanced Barrier Precautions include:
- Dressing
- Bathing/showering
- Transferring
- Providing hygiene
- Changing linens
- Changing briefs or assisting with toileting
- Device care or use: central line, urinary catheter, feeding tube, tracheostomy/ventilator
- Wound care: any skin opening requiring a dressing
In general, gown and gloves would not be required for resident care activities other than those listed above, unless otherwise necessary for adherence to Standard Precautions. Residents are not restricted to their rooms or limited from participation in group activities. Because Enhanced Barrier Precautions do not impose the same activity and room placement restrictions as Contact Precautions, they are intended to be in place for the duration of a resident's stay in the facility or until resolution of the wound or discontinuation of the indwelling medical device that placed them at higher risk.
Table: Summary of PPE Use and Room Restriction When Caring for Residents Colonized or Infected with MDROs in Nursing Homes
| Precautions | Applies to: | PPE used for these situations: | Required PPE | Room restriction |
|---|---|---|---|---|
| Standard Precautions | All residents | Any potential exposure to:
|
Depending on anticipated exposure:
gloves, gown, or facemask or eye protection (Change PPE before caring for another resident) |
None |
| Enhanced Barrier Precautions | All residents with any of the following:
|
During high-contact resident care activities:
|
Gloves and gown prior to the high-contact care activity
(Change PPE before caring for another resident) (Face protection may also be needed if performing activity with risk of splash or spray) |
None |
| Contact Precautions | All residents infected or colonized with a MDRO in any of the following situations:
All residents who have another infection (e.g., C. difficile, norovirus, scabies) or condition for which Contact Precautions is recommended in Appendix A (Type and Duration of Precautions Recommended for Selected Infections and Conditions) of the CDC Guideline for Isolation Precautions |
Any room entry | Gloves and gown
(Don before room entry, doff before room exit; change before caring for another resident) (Face protection may also be needed if performing activity with risk of splash or spray) |
Yes, except for medically necessary care |
Decisions regarding the use of additional practices to prevent the spread of MDROs can be determined in conjunction with public health. These strategies might differ depending on the prevalence or incidence of the MDRO in the facility and region. Visit state-based HAI prevention to find contact information for your state health department HAI program.
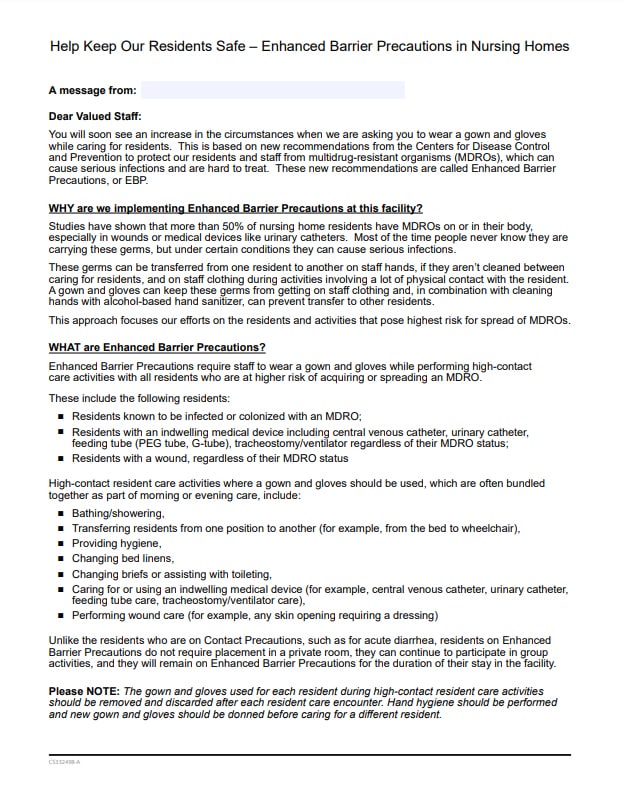
Implementation
When implementing Contact Precautions or Enhanced Barrier Precautions, it is critical to ensure that staff have awareness of the facility's expectations about hand hygiene and gown/glove use, initial and refresher training, and access to appropriate supplies. To accomplish this:
- Post clear signage on the door or wall outside of the resident room indicating the type of Precautions and required PPE (e.g., gown and gloves)
- For Enhanced Barrier Precautions, signage should also clearly indicate the high-contact resident care activities that require the use of gown and gloves
- For Enhanced Barrier Precautions, signage should also clearly indicate the high-contact resident care activities that require the use of gown and gloves
- Make PPE, including gowns and gloves, available immediately outside of the resident room
- Ensure access to alcohol-based hand rub in every resident room (ideally both inside and outside of the room)
- Position a trash can inside the resident room and near the exit for discarding PPE after removal, prior to exit of the room or before providing care for another resident in the same room
- Incorporate periodic monitoring and assessment of adherence to determine the need for additional training and education
- Provide education to residents and visitors
Note: Prevention of MDRO transmission in nursing homes requires more than just proper use of PPE and room restriction. Guidance on implementing other recommended infection prevention practices (e.g., hand hygiene, environmental cleaning, proper handling of wounds, indwelling medical devices, and resident care equipment) are available in CDC's free online course — The Nursing Home Infection Preventionist Training. Nursing homes are encouraged to have staff review relevant modules and to use the resources provided in the training (e.g., policy and procedure templates, checklists) to assess and improve practices in their facility.
Resources
- Consideration for the Use of Enhanced Barrier Precautions in Skilled Nursing Facilities
- Dumyati G, Stone ND, Nace DA, Crnich CJ, Jump RL. Challenges and Strategies for Prevention of Multidrug-Resistant Organism Transmission in Nursing Homes. Current Infectious Disease Reports 2017;19:18.
- McKinnell JA, Singh RD, Miller LG, et al. The SHIELD Orange County Project: Multidrugresistant Organism Prevalence in 21 Nursing Homes and Long-term Acute Care Facilities in Southern California. Clinical Infectious Diseases 2019;69:1566-73.
- Mody L, Bradley SF, Galecki A, Olmsted RN, Fitzgerald JT, Kauffman CA, Saint S, Krein SL. Conceptual model for reducing infections and antimicrobial resistance in skilled nursing facilities: focusing on residents with indwelling devices. Clin Infect Dis. 2011 Mar 1;52(5):654-61. doi: 10.1093/cid/ciq205. Review.
- Rossow J, Ostrowsky B, Adams E, et al. Factors Associated With Candida auris Colonization and Transmission in Skilled Nursing Facilities With Ventilator Units, New York, 2016–2018. Clinical Infectious Diseases 2020.
- Pacilli M, Kerins JL, Clegg WJ, et al. Regional Emergence of Candida auris in Chicago and Lessons Learned From Intensive Follow-up at 1 Ventilator-Capable Skilled Nursing Facility. Clinical Infectious Diseases 2020;71:e718-e25.
- Lin MY, Froilan MC, Lolans K, et al. The Importance of Ventilator Skilled Nursing Facilities (vSNFs) in the Regional Epidemiology of Carbapenemase-Producing Organisms (CPOs). Open Forum Infectious Diseases; 2017: Oxford University Press US. p. S137-S8.
- Mody L, Kauffman CA, Donabedian S, Zervos M, Bradley SF. Epidemiology of Staphylococcus aureus Colonization in Nursing Home Residents. Clinical Infectious Diseases 2008;46:1368-73
- CDC Containment Strategy Responding to Emerging AR Threats
- Clinicians: Information about CRE | HAI | CDC
- Roghmann MC, Johnson JK, Sorkin JD, Langenberg P, Lydecker A, Sorace B, Levy L and Mody L. Transmission of Methicillin-Resistant Staphylococcus aureus (MRSA) to Healthcare Worker Gowns and Gloves During Care of Nursing Home Residents Infect Control Hosp Epidemiol. 2015 Sep;36(9):1050-7. doi: 10.1017/ice.2015.119
- Blanco N, Pineles L, Lydecker AD, Johnson JK, Sorkin JD, Morgan DJ; VA Gown and Glove Investigators, Roghmann MC. Transmission of Resistant Gram-Negative Bacteria to Health Care Worker Gowns and Gloves during Care of Nursing Home Residents in Veterans Affairs Community Living Centers Antimicrob Agents Chemother. 2017 Sep 22;61(10). pii: e00790-17. doi: 10.1128/AAC.00790-17.
- Mody L, Bradley SF, Galecki A, Olmsted RN, Fitzgerald JT, Kauffman CA, Saint S, Krein SL. Conceptual model for reducing infections and antimicrobial resistance in skilled nursing facilities: focusing on residents with indwelling devices.external icon Clin Infect Dis. 2011 Mar 1;52(5):654-61. doi: 10.1093/cid/ciq205. Review.
- Pineles L, Morgan DJ, Lydecker A, et al. Transmission of Methicillin-Resistant Staphylococcus aureus to Health Care Worker Gowns and Gloves During Care of Residents in Veterans Affairs Nursing Homes. American Journal of Infection Control 2017;45:947-53.
- Blanco N, Johnson JK, Sorkin JD, et al. Transmission of Resistant Gram-Negative Bacteria to Healthcare Personnel Gowns and Gloves During Care of Residents in Community-Based Nursing Facilities. Infection Control and Hospital Epidemiology 2018;39:1425-30.
- Lydecker AD, Osei PA, Pineles L, et al. Targeted Gown and Glove Use to Prevent Staphylococcus aureus Acquisition in Community-Based Nursing Homes: A Pilot Study. Infection Control & Hospital Epidemiology 2020:1-7.