Key points
- Kyasanur Forest Disease (KFD) is a viral disease mostly found in southern India and diagnosed in 400-500 people each year.
- Spread to people primarily occurs through tick bites or contact with infected animals.
- KFD can be fatal.
- There is a vaccine available for people at risk for KFD.

What it is
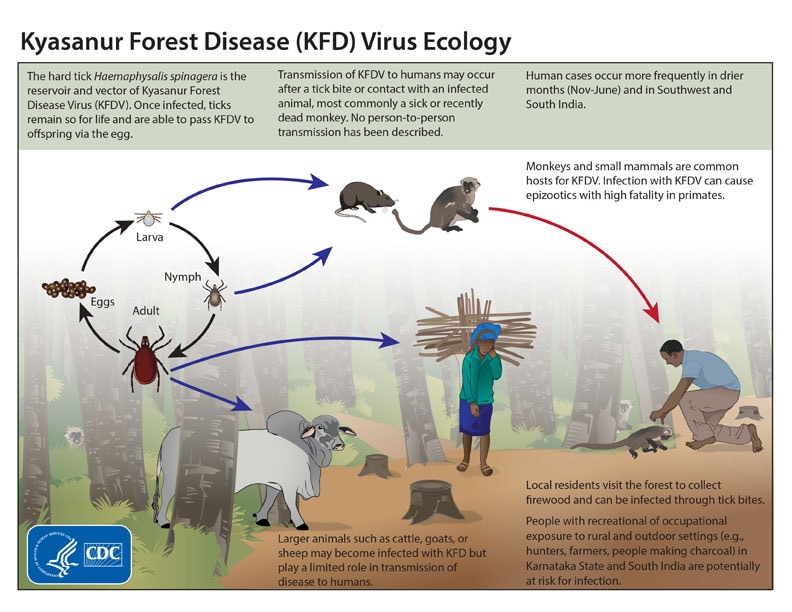
Kyasanur Forest Disease (KFD) is a serious disease caused by the KFD virus that was first identified in the Kyasanur Forest of India. Hard ticks (Hemaphysalis spinigera) spread the KFD virus to people and to animals like monkeys and rodents. It's found in Karnataka, Tamil Nadu, Kerala, Goa, and Maharashtra states of India.
Signs and symptoms
People with KFD usually start having symptoms three to eight days after being infected with the virus. Some people may not have any symptoms at all, while others may have a sudden onset of chills, fever, and headache. Severe muscle pain, vomiting, gastrointestinal symptoms, and bleeding can follow three or four days after symptoms begin.
Most patients recover one to two weeks after symptoms begin. About 10 to 20 percent of patients experience a second wave of symptoms, including severe headache, mental disturbances, shakes (tremors), and problems seeing.
Healthcare providers diagnose KFD using blood tests.
Risk factors
Hunters, herders, forest workers, and farmers in the Karnataka, Tamil Nadu, Kerala, Goa, and Maharashtra states of India, where laboratory confirmed cases of KFD have been reported, are at higher risk for getting KFD. This is because they are more likely to be bitten by infected ticks. People are more likely to get KFD during the dry season of November to June.
Travelers visiting a location with a history of KFD spread are at risk of infection.

How it spreads
- People get KFD from infected tick bites or exposure to an infected animal.
- Infected ticks can live on livestock, but livestock rarely spread KFD to people.
- KFD does not spread between people.
Prevention
To prevent KFD:
- Use insect repellent containing DEET to prevent tick bites.
- Consider getting the KFD vaccine if you live in or are traveling to an area where KFD is found.
- Avoid contact with dead or sick animals, particularly monkeys.
Treatment and recovery
There is no cure for KFD.
Supportive care is crucial, including fluid balance, providing oxygen, managing blood pressure, and treating additional infections.
With quick medical care, many patients recover from KFD without complications. However, about three to 10 percent of people with the disease will die.
- Boshell J. Kyasanur Forest Disease: Ecologic Considerations. American Journal of Tropical Medicine and Hygiene. 1969; 18(1): 67-80.
- Kasabi GS, Murhekar MV, Yadav PD, et al. Kyasanur Forest Disease, India, 2011-2012. Emerging Infectious Diseases. 2013; 19(2): 278-281.
- Kyasanur forest disease virusExternal. Material Safety Data Sheet (MSDS), Public Health Agency of Canada.
- Mourya DT, Yadav PD, Mehla R, et al. Diagnosis of Kyasanur forest disease by nested RT-PCR, real-time RT-PCR and IgM capture ELISA. Journal of Virological Methods. 2012; 186: 29-54.
- Work TH. Kyasanur forest disease. A new virus disease in India. Summary of preliminary report on investigations of the Virus Research Center on an epidemic disease affecting forest villagers and wild monkeys of Shimoga Districk, Mysore. Indian Journal of Medical Sciences. 1957; 11:341-342.
- Work TH, Trapido H, Narasimha MDP, et. al. Kyasanur forest disease III. A preliminary report on the nature of the infection and clinical manifestations in human beings. Indian Journal of Medical Sciences. 1957; 11:619-645.
- Kaushal H, Kumar Meena V, Das S. et al. Pathogenicity and virulence of Kyasanaur Forest disease: A comprehensive review of an expanding zoonotic threat in southwestern India. Virulence. 2025 Dec;16(1):2580154.
