At a glance
Read CDC's 2021 yearly summary of investigations of possible multistate outbreaks caused by Salmonella, Shiga toxin-producing E. coli, and Listeria monocytogenes
Key findings
Possible multistate outbreaks
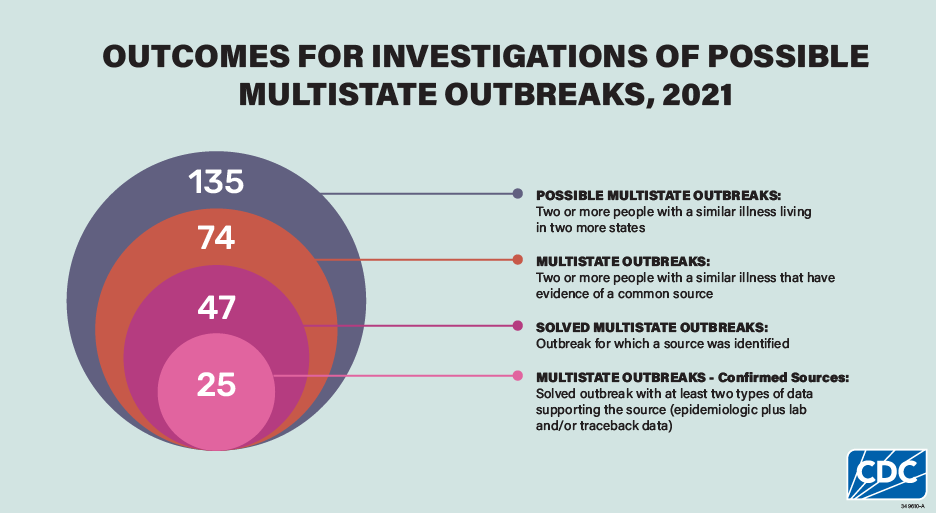
This analysis includes 135 investigations of possible multistate enteric (intestinal) outbreaks during 2021. Some possible outbreaks were excluded from this report because they were determined to be single state or because they were linked to international travel. After investigation, 74 (55%) of these were determined to be multistate outbreaks, and investigators solved 47 (64%) of these outbreaks.
Multistate outbreaks
The number of outbreaks increased from 2020 but was lower than the 82 investigated outbreaks in 2019. The number of outbreaks investigated in 2021 was likely lower than that in 2019 due in part to continued effects of the COVID-19 pandemic on enteric disease outbreak detection and investigation (e.g., decreased resources at local, state, and federal public health agencies, changes in healthcare-seeking behavior, and changed restaurant dining and grocery shopping patterns.) Additionally, changing diagnostic testing practices likely continued to affect enteric disease surveillance and the ability to identify possible outbreaks.
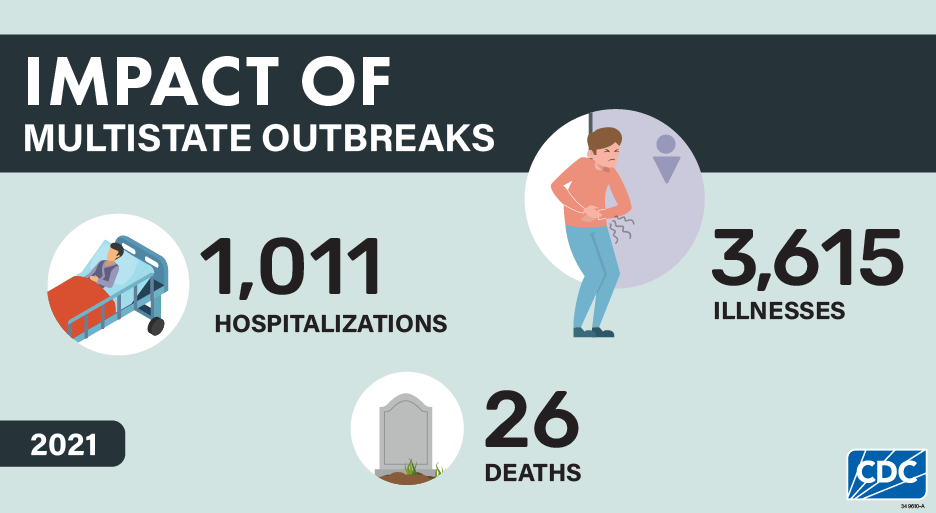
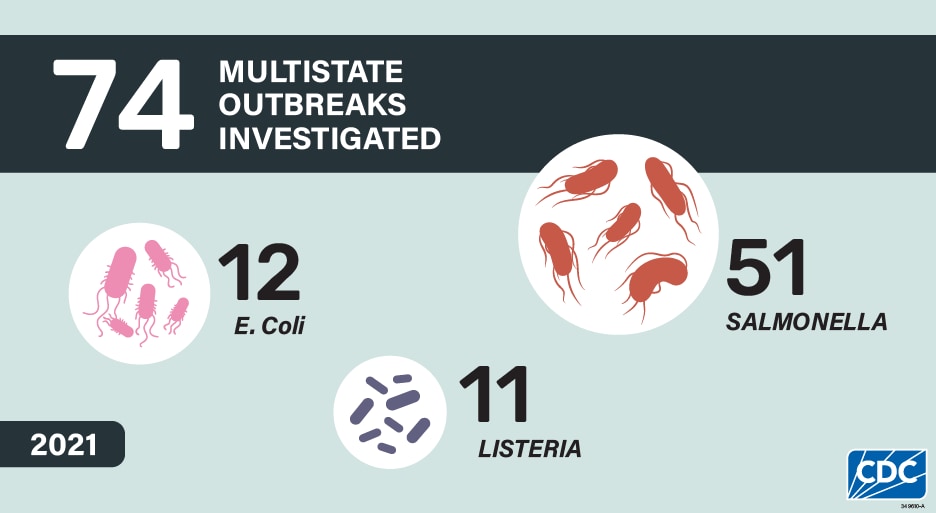
The 74 investigated multistate outbreaks resulted in 3,615 illnesses, 1,011 hospitalizations, and 26 deaths. Consistent with what was seen in previous summaries, Salmonella caused the highest number of multistate outbreaks (51) and illnesses (3,320), comprising 69% of the multistate outbreaks and the overwhelming majority (92%) of illnesses. These numbers substantially underrepresent the true number of illnesses caused by these outbreaks because many people do not seek medical care or do not get tested to see what bacteria could be causing their illness. Without testing, they are not identified as being part of a multistate outbreak.
Solved multistate outbreaks
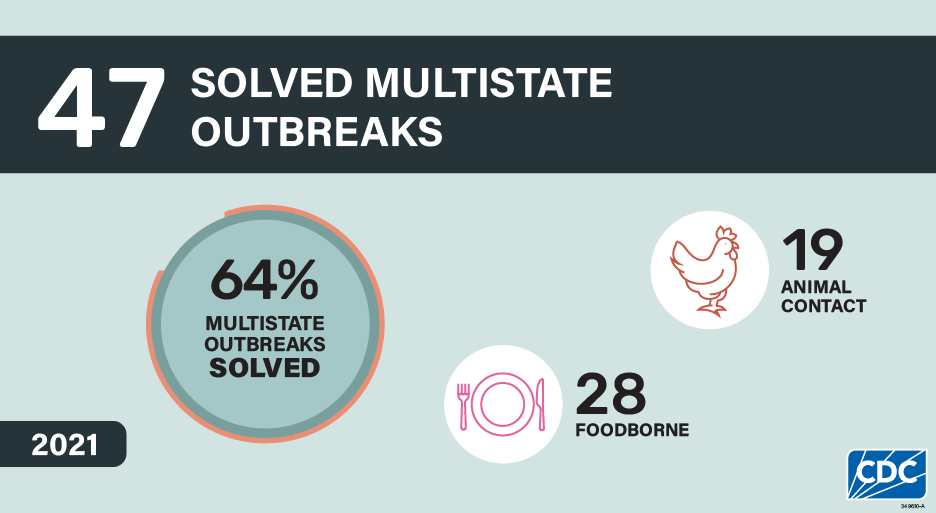
Among the 74 multistate outbreaks, 47 (64%) were solved, meaning a confirmed or suspected source of the outbreak was identified, including 25 (53%) outbreaks with confirmed sources and 22 (47%) with suspected sources. Among the 47 solved outbreaks, 28 (60%) were linked to contaminated foods, and 19 (40%) were linked to animal contact.
Solved multistate outbreaks caused at least 2,047 illnesses. Solved multistate outbreaks linked to contaminated food caused 1,740 illnesses, 496 hospitalizations, and 15 deaths, while multistate outbreaks linked to animal contact caused 1,307 illnesses, 329 hospitalizations, and 3 deaths.
Highlights
Salmonella and songbirds

Why was this outbreak notable?
In 2021, the first documented U.S. multistate outbreak of Salmonella infections in humans associated with songbird contact occurred. An investigation by state and federal public health partners confirmed a link between infected songbirds and human illnesses. People likely became sick by handling sick and dead birds and touching contaminated birdfeeders. Pet dogs and cats can also get sick if they hunt and catch sick birds or have contact with bird droppings; one ill dog tested positive for the outbreak strain, and a cat was reportedly ill after contact with a wild bird. This outbreak highlights a One Health issue, where a preventative action (regularly cleaning birdfeeders) could reduce the health risk to people, pets, and wild birds.
What happened as a result of this outbreak?
CDC and state health and wildlife partners worked together to spread prevention messages. A CDC Investigation Notice detailed the outbreak investigation and provided recommendations about cleaning birdfeeders and keeping pets away from birdfeeders. State health and wildlife partners shared similar recommendations, advising the public about the outbreak and where to report wild bird deaths. For wildlife officials, having CDC involved increased the reach of health messaging to a national level and helped raise awareness of steps that could be taken to prevent Salmonella infections among people, pets, and wild birds.
Salmonella and turtles

Why was this outbreak notable?
This was the first multistate outbreak of Salmonella in the United States linked to a specific supplier of small turtles sold to pet stores. The sale of small turtles (shells less than 4 inches in length) for pets was banned in the United States in the 1970s because they were linked to Salmonella illnesses and outbreaks. This outbreak highlights the persistent challenges related to the illegal sale and distribution of small turtles despite the federal ban and state prohibitions. This outbreak also highlighted the risk of illnesses associated with small turtles, especially to children younger than 5 years of age. Almost half of the illnesses in this outbreak were in children younger than 5 years old.
What happened as a result of this outbreak?
CDC, state health departments, and the Pet Advocacy Network provided advice for pet stores to prevent illness from small turtles. CDC posted an outbreak notice to inform the public about the investigation and the risk associated with small turtles, and provided information on how to be safe around your pet turtle.
Salmonella and frozen breaded stuffed raw chicken products

Why was this outbreak notable?
In 2021, investigators linked an outbreak of 36 Salmonella Enteritidis infections to frozen breaded stuffed raw chicken products. These products have repeatedly been implicated as the source of outbreaks over the past two decades. The breading of frozen breaded stuffed raw chicken products is often browned, which makes them appear cooked. But because they contain raw chicken, these products need to be cooked to an internal temperature of 165F to make them safe to eat. Before this outbreak, producers attempted to reduce the risk of illness by changing packaging to more clearly label the products as raw, warn against using microwaves to prepare them, and provide cooking instructions for conventional ovens only.
What happened as a result of this outbreak?
U.S. Department of Agriculture's Food Safety Inspection Service (USDA FSIS) has announced their intention to declare Salmonella an adulterant in these products at certain levels. Preventing Salmonella illnesses due to consumption of contaminated chicken is a priority for CDC. To inform prevention strategies for regulatory agencies and industry, CDC is preparing a summary of data from investigations of outbreaks linked to frozen breaded and stuffed raw chicken products. CDC also conducted surveys to better understand how people use cooking appliances to prepare frozen stuffed chicken products. CDC found that respondents with lower income or who live in mobile types of homes reported higher use of microwaves and lower use of conventional ovens. Companies could consider implementing additional interventions that rely less on labeling and consumer preparation practices to ensure safety.
Multiple pathogens and leafy greens

Why were these outbreaks notable?
Investigators linked five multistate outbreaks (3 STEC, 1 Listeria, and 1 Salmonella outbreak) and 82 illnesses to consumption of packaged leafy greens, including spinach, romaine, a "power greens" blend, and other packaged salads in 2021. While outbreaks linked to leafy greens have been previously highlighted in past summaries, 2021 was the first time a multistate outbreak was linked to lettuce grown in a controlled environment agriculture (CEA) indoor hydroponic operation. Although the route and source of leafy green contamination was not identified, the outbreak strain of Salmonella was detected in a stormwater retention basin adjacent to the facility and another type of Salmonella was found in an indoor production pond.
What happened as a result of these outbreaks?
This outbreak emphasizes the importance of identifying and mitigating potential routes of contamination during the growth and harvest of leafy greens, whether they are grown hydroponically or with conventional methods. FDA highlighted several requirements and recommendations for CEA indoor hydroponic operations, including ensuring water is of sufficient sanitary quality for its intended use, and conducting root cause analyses. Together, the 2021 investigations illustrate that contaminated leafy greens remain a recurring public health concern and that outbreaks can be caused by a variety of pathogens and types of leafy greens. Prevention of STEC infections linked to consumption of leafy greens continues to be a priority for CDC and FDA.
Salmonella and pre-cut melons and other fruit

Why was this outbreak notable?
In 2021, an outbreak of Salmonella Javiana infections sickened at least 70 people in 5 states and was linked to fresh pre-cut cantaloupe processed at one facility. It is the fourth large multistate Salmonella outbreak linked to pre-cut melons and other pre-cut fruit since 2018. Investigators identified several clusters of illnesses at hospitals, long-term care facilities, and other institutions that serve people at higher risk of serious illness from salmonellosis. This has also been observed in previous pre-cut melon-associated outbreaks.
What happened as a result of these outbreaks?
Given the recurrence of Salmonella outbreaks linked to pre-cut melons, and the population impacted by these outbreaks, additional steps to increase safety of these products may be needed. A better understanding of the factors that lead to contamination of melons in the field and the processing steps that could increase contamination is needed. Implementation of interventions like irradiation or other processing steps to eliminate or reduce any pathogens present on cut melon could be considered, particularly for pre-cut melons served in settings with people at higher risk for severe salmonellosis. CDC plans to analyze data from these outbreaks to identify prevention opportunities.
Salmonella and Italian-style meats

Why were these outbreaks notable?
In 2021, two multistate outbreaks of Salmonella linked to Italian-style meats made with pork sickened 74 people: one was linked to an uncured antipasto assortment and the other to "all natural" salami sticks. In both outbreaks, the implicated foods were produced without added synthetic nitrates or nitrites, which are commonly added to processed meats as a preservative to inhibit the growth of bacteria, enhance color, and extend shelf life. These outbreaks may indicate an emerging food safety issue as manufacturers produce more uncured meats in response to consumer interest in foods produced without synthetic nitrates or nitrites.
What happened as a result of these outbreaks?
USDA FSIS is working with Agricultural Research Service researchers to identify additional approaches to ensure these products are safe, including examining the role of sausages' diameter on drying times needed to kill pathogens. Companies that produce fermented and dried meat products should ensure they have validated processes with sufficient scientific evidence that results in at least a 5-log reduction in Salmonella. In response to recommendations from a National Advisory Committee for Meat and Poultry Inspection subcommittee in 2020, USDA FSIS updated its objectives to include scientific information to inform development of lethality treatments for these products.
Multistate outbreaks linked to food
Of the 47 total solved multistate outbreaks, 28 were found to be linked to contaminated foods. Almost half (46%) had suspected food vehicles and 54% had a confirmed food vehicle.
Among all illnesses related to solved foodborne outbreaks, 6% occurred in children under 5 and 18% occurred in adults over 65 years, age groups at higher risk for severe illness.
These solved multistate foodborne outbreaks were associated with 1,740 illnesses, 496 hospitalizations, and 15 deaths. Ill people in these outbreaks ranged in age from less than 1 year to 101 years, with a median age of 38; 59% were female. Among all illnesses related to solved foodborne outbreaks, 6% occurred in children under 5 and 18% occurred in adults over 65 years, age groups at higher risk for severe illness. When compared with Salmonella or STEC infections, a higher proportion of solved multistate foodborne outbreaks of Listeria infections were in adults over 65 (43%).
Salmonella caused the most multistate foodborne outbreaks (16 outbreaks, 57%), followed by Listeria (8 outbreaks, 29%), and STEC (4 outbreaks, 14%). Foodborne Salmonella outbreaks caused more illnesses (median: 34 illnesses, range: 9–1,040) compared to outbreaks caused by STEC (median: 12 illnesses, range: 10–15) and Listeria (median: 9 illnesses, range: 3–21).
As in previous years, illnesses associated with solved multistate foodborne Listeria outbreaks were more severe: overall, 97% of people in Listeria outbreaks were hospitalized and 15% died, compared to 33% of people hospitalized and 0.3% of people who died in multistate Salmonella outbreaks and 43% of people hospitalized and 2% died in STEC outbreaks.
CDC's Outbreak Response and Prevention Branch (ORPB) assigned food categories for specific foods linked to outbreaks based on the Interagency Food Safety Analytics Collaboration (IFSAC) categorization scheme. Chicken and vegetable row crops were identified as the source of the most solved foodborne outbreaks (5 each) during 2021. Of the five outbreaks associated with chicken, one involved frozen breaded stuffed chicken, one involved pre-cooked chicken, and in three the type of chicken product could not be determined. Leafy greens were the product identified in all five outbreaks due to vegetable row crops. Dairy products and fruit were each identified as the source of three solved foodborne outbreaks. All three outbreaks associated with dairy products involved soft cheeses, with two of them due to queso fresco type cheeses. The three outbreaks associated with fruit were due to contaminated avocadoes, blueberries, and pre-cut cantaloupe. Although root/underground vegetables were the source of just one solved foodborne outbreak, confirmed to be linked to onions, it resulted in the most solved foodborne outbreak-associated illnesses (1,040) of any food category.
Although root/ underground vegetables were the source of just one outbreak, confirmed to be linked to onions, they resulted in the most outbreak-associated illnesses (1,040) of any food category.
| Food Category | Pathogen(s) | Confirmed Source(s) | Suspected Source(s) |
|---|---|---|---|
| Beef | Salmonella (1 suspected) | NA | Beef (1) |
| Chicken | Salmonella (1 confirmed, 3 suspected), Listeria (1 confirmed) | Pre-Cooked Chicken (1), Frozen Stuffed Chicken (1) | Chicken (3) |
| Crustaceans | Salmonella (1 confirmed) | Shrimp Cocktail (1) | NA |
| Dairy | Listeria (1 confirmed, 2 suspected) | Soft Cheese (1) | Soft Cheese (2) |
| Fish | Listeria (1 suspected), Salmonella (1 confirmed) | Seafood (1) | Smoked Fish (1) |
| Fruits | Salmonella (1 confirmed, 2 suspected) | Cut Cantaloupe (1) | Hass Avocados (1), Blueberries (1) |
| Fungi | Listeria (1 suspected) | NA | Enoki Mushrooms (1) |
| Grains-Beans | E. coli (1 suspected) | NA | Cake Mix (1) |
| Nuts-Seeds | Salmonella (1 confirmed) | Vegan Cashew Brie Cheese (1) | NA |
| Other Meat not Poultry | Salmonella (1 confirmed) | Italian-Style Meats (1) | NA |
| Pork | Salmonella (1 confirmed), Listeria (1 suspected) | Salami Sticks (1) | Polish Meat (1) |
| Root Underground Vegetables | Salmonella (1 confirmed) | Onions (1) | NA |
| Turkey | Salmonella (1 confirmed) | Ground Turkey (1) | NA |
| Vegetable Row Crops | Salmonella (1 confirmed), E. coli (1 suspected, 2 confirmed), Listeria (1 confirmed) | Prepackaged Leafy Greens (1), Packaged Salad (1), Fresh Spinach (1), Organic Power Greens (1) | Romaine (1) |
Outbreaks linked to animal contact
Of the 47 solved multistate outbreaks, 19 were linked to contact with animals. These outbreaks were associated with 1,307 illnesses, 329 hospitalizations, and 3 deaths. During 2021, Salmonella caused all outbreaks linked to contact with animals. During 2021, investigators solved all 19 outbreaks linked to animal contact.
The proportion of sick children younger than 5 was higher for solved multistate animal contact outbreaks (26%) than for solved multistate foodborne outbreaks (6%).
Sick people in multistate outbreaks linked to animal contact ranged in age from less than 1 to 97 years, with a median age of 32 years; 26% of illnesses occurred in children younger than 5, and 16% occurred in adults aged 65 and older. The proportion of sick children younger than 5 was higher for solved multistate animal contact outbreaks (26%) than for solved multistate foodborne outbreaks (6%). Over half (58%) were female. Among all multistate animal contact outbreaks, the median percentage of people hospitalized per outbreak was 33%, with a range of 0 to 111 people hospitalized.
During 2021, there were 12 multistate outbreaks, 1,135 illnesses, 274 hospitalizations, and 2 deaths linked to contact with backyard poultry. Animal contact outbreaks linked to contact with backyard poultry outnumbered those linked to all other animal sources combined. Backyard poultry, such as chickens, ducks, geese, and turkeys can carry Salmonella even if they look healthy, appear clean, and show no signs of illness. Contact with backyard poultry is an established risk factor for transmission of Salmonella due to direct contact with birds or their environment.
Turtles were the source of three multistate animal contact outbreaks, causing the second highest number of multistate outbreaks linked to animal contact. Multistate outbreaks linked to turtles caused 109 outbreak-associated illnesses, 38 hospitalizations, and 1 death during 2021. Children under the age of 5 years accounted for 45% of the illnesses associated with these 3 small turtle outbreaks. All three outbreaks associated with turtles were linked specifically to small turtles (shell length <4 inches). A federal law bans the sale and distribution of turtles with shells less than 4 inches long as pets because they have caused many illnesses. However, these turtles can sometimes be found illegally online and at stores, flea markets, and roadside stands. People can get sick from Salmonella by touching turtles, their tank water, their supplies, or the areas where they live and roam.
| Animal Category | Pathogen(s) | Confirmed Source(s) | Suspected Source(s) |
|---|---|---|---|
| Dogs | Salmonella (1 confirmed) | Pigs Ears | NA |
| Multiple | E.coli (1 confirmed) | Cattle/Horses | NA |
| Backyard Poultry | Salmonella (42 confirmed, 8 suspected) | Live Poultry (42) | Live Poultry (8) |
| Cattle | Salmonella (1 confirmed) | Cattle | NA |
| Small Mammals | Salmonella (3 confirmed) | Guinea Pig (1), Hedgehogs (2) | NA |
| Scaled Reptiles | Salmonella (4 confirmed, 2 suspected) | Bearded Dragons (2), Leopard Gecko (1), Snake/Rodent (1) | Bearded Dragons (2) |
| Turtles | Salmonella (4 confirmed, 1 suspected) | Small Turtles (4) | Small Turtles (1) |
What's being done
When investigators find the food or animal source of a multistate outbreak, agencies can take actions, such as issuing outbreak notices or requesting that companies recall contaminated products (FSIS and FDA recall pages). Warning the public quickly about contaminated foods or animal contact outbreaks can prevent illnesses and save lives. Not every outbreak with a confirmed source results in product actions or outbreak notices. Outbreaks may end by the time the source is confirmed, or investigators may determine that the contaminated food is no longer available for sale.
In 2021, CDC issued notices for 20 multistate outbreaks. The 20 outbreaks included 17 linked to contaminated foods (15 with a confirmed source, 1 with a suspected source, 1 linked to an unknown food source,) and 3 linked to animal contact. Among the 15 outbreaks with a confirmed food source, 12 resulted in food recalls. In total, the outbreak notices received nearly 5 million page views, including a large Salmonella outbreak linked to onions which received more than 1 million views.
CDC used Facebook and Twitter to disseminate advice to the public for all 20 outbreaks. Foodborne outbreak messages were the top performing CDC posts in 2021, even when including COVID-19 posts. A Facebook post about a Salmonella outbreak linked to frozen shrimp was CDC's top post for 2021 with 33 million views. CDC notified news media partners about 15 outbreaks and many outbreaks received substantial media coverage.
For more information on how CDC decides to communicate during foodborne outbreaks, please see the Issuing Foodborne Outbreak Notices web page.
Methods
The data sources and methods used for the analyses in this report have been previously described in detail in the previous "Summary of Possible Multistate Enteric (Intestinal) Disease Outbreaks from 2017–2020" and in the MMWR report of 2016 data. Briefly, CDC maintains an internal tracking database in the System for Enteric Disease Response, Investigation, and Coordination (SEDRIC) of investigations coordinated by CDC of possible multistate outbreaks caused by Salmonella, Shiga Toxin–Producing Escherichia coli (referred to as STEC for simplicity throughout this report), and Listeria monocytogenes (referred to as Listeria throughout this report.) These analyses were based on data in SEDRIC, with additional patient age information from PulseNet. An investigation of a possible multistate outbreak was included in this report if it began on or after January 1, 2021 and ended on or before March 31, 2022; or if it began before 2021 but ended during April 1, 2021–March 31, 2022. For outbreaks linked to specific foods, outbreak vehicles were provisionally assigned food categories based on the fourth-level Interagency Food Safety Analytics Collaboration (IFSAC) categorization scheme.
The number of multistate outbreaks reported here will differ from the number of outbreaks reported in CDC's Foodborne Disease Outbreak Surveillance System (FDOSS), which includes both single state and multistate outbreaks and a larger group of pathogens. In addition, the investigation year in this report, which is based on when CDC investigated the possible outbreak, may differ from the outbreak year in FDOSS, which is based on when outbreak-associated illnesses occurred. ORPB provisionally assigned IFSAC food categories to outbreaks in this report. Final IFSAC food category assignments for both single state and multistate outbreaks are made during the annual FDOSS outbreak closeout process.
Acknowledgements
This work would not be possible without the collaboration and critical work of many partners, including local, state, tribal, and territorial health and agriculture departments; the PulseNet database team, CDC; the Outbreak Response and Prevention Branch (ORPB), CDC; Food and Drug Administration Coordinated Outbreak Response and Evaluation Network, Washington, DC; and the U.S. Department of Agriculture Food Safety Inspection Service Office of Public Health Science, Applied Epidemiology Staff, Washington, DC. We would like to also acknowledge Kaylea Nemechek, Lexi Palacios, Benjamin Schneider, Karen Neil, Katherine Marshall, Kathy Benedict, Laura Whitlock, Lauren Gollarza, Sybil Masse and Sarah Collier (ORPB) for their efforts during the writing of this report.
