About
CDC researchers use influenza virus activity data from past flu seasons (e.g., influenza-like illness (ILI), influenza hospitalization rates, and influenza deaths) to develop intensity thresholds (ITs) to classify the severity of flu seasons each year.
How CDC Classifies Flu Severity each Season in the United States
CDC classifies influenza (flu) season severity both during the season and at the end of each season. CDC researchers use influenza virus activity data from past flu seasons (e.g., influenza-like illness (ILI), influenza hospitalization rates, and influenza deaths) to develop intensity thresholds (ITs) to classify the severity of flu seasons. By measuring the severity of flu seasons, CDC can use key flu indicator data to guide public health actions, such as targeting prevention and treatment messages to appropriate audiences and make recommendations designed to prevent flu illnesses and death.
The past season severity assessment page is updated at the end of each flu season. CDC also shares in-season severity assessments, which are available weekly throughout the flu season. Past flu season severity assessments are available at Past Flu Season Severity Assessments. In addition to assessing the severity of flu seasons, this methodology may also be used to help monitor the severity during a flu pandemic.
How CDC tracks flu activity
CDC tracks flu activity through key flu indicators, including the percentage of influenza-like illness (ILI) visits to outpatient health clinics, the rates of flu-related hospitalizations, and the percentage of deaths resulting from flu.
How CDC defines "severity"
CDC began using an approach published in 2017 to define flu season severity. CDC first calculates intensity thresholds for three key flu indicators (ILI visits, rates of flu-related hospitalizations, and percentage of deaths resulting from flu) using data from past flu seasons. CDC then classifies the severity of specific flu seasons or a given week during the flu season by determining whether the indicator values during the peak of each flu season crossed their respective ITs.
Data sources used to classify flu severity
U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet): Percent of outpatient visits for flu-like illness out of all outpatient visits by week. ILINet sites that collect age-specific data on the number of influenza-like illness visits and total number of outpatient visits are used for the severity assessment.
Influenza Hospitalization Surveillance Network (FluSurv-NET): Adjusted rate of flu-related hospitalizations per 100,000 people by week. Hospitalization rates are adjusted using data from past seasons on testing practices and the sensitivity of diagnostic tests.
National Center for Health Statistics (NCHS) Mortality Surveillance Data: Percent of flu-coded deaths out of all reported deaths by week.
The data used to assess severity are available for download through the weekly FluView report.
Intensity thresholds and why they are important
An intensity threshold is a statistical value developed using data from past flu seasons that is used to assess how severe a flu season is considered to be by comparing current season data with the IT value from past seasons. In this instance, intensity thresholds are important because they help researchers classify flu severity based on the level of flu activity at the peak of the season. ITs were developed for the overall population and further separated into three age groups: children, adults, and older adults. The ITs used correspond to a 50% (1 in 2), 10% (1 in 10) and 2% (1 in 50) chance of exceedance during a flu season. These threshold values were used to classify flu severity into low, moderate, high, and very high categories and then applied to U.S. seasons from 2003–2004 through 2023–2024, excluding the 2020–2021 season due to limited flu activity.
How researchers classify severity each week during the season
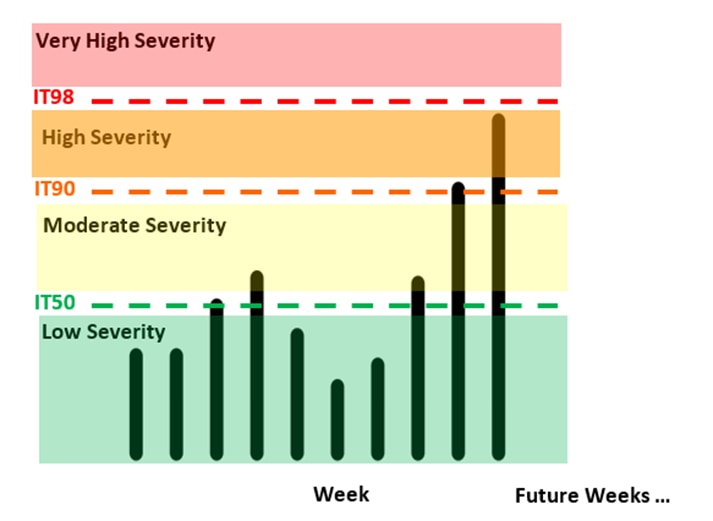
Each week, CDC assesses the flu severity in the United States using the three indicators across all age groups (percent of influenza-like illness (ILI), flu-related hospitalization rate, and percent of flu deaths) and compares the weekly values to intensity thresholds calculated from past seasons. Each indicator is assessed separately. The Moving Epidemic Method is used to translate the data into standardized intensity thresholds for each indicator across all age groups. Using this method, the weekly value of an indicator across all ages is compared to the respective IT for that indicator to determine a severity classification. If the weekly indicator value falls below all thresholds, the week is classified as low severity. If the weekly indicator value is equal to or above the IT50 and below the IT90, the classification would be moderate. If the weekly indicator value is equal to or above the IT90 and below the IT98, the classification would be high. If the weekly indicator value is above the IT98, the classification would be very high. This is then repeated for the next indicator. For each week, the overall weekly assessment of severity is classified based on all three indicators combined. If two or three indicators have the same assessment, then the overall classification is matched to those indicators. If all three of the indicators have different classifications, then the classification in the middle is used for the overall classification. Weekly severity assessments may change because indicator data may not be complete at the time of assessment because of reporting delays and backfill of information.
Figure 1: Illustration of how researchers classify severity for flu weekly
How researchers classify the severity of each flu season
Flu severity is assessed across all ages and for three broad age groups using the following data from each season:
- the percentage of all patient visits to outpatient clinics that are for influenza-like illness (ILI)
- the rate of flu-related hospitalizations, and
- the percentage of deaths resulting from flu
The Moving Epidemic Method is then used to translate the data into standardized intensity thresholds for each indicator by age group. Severity is assessed across all ages and by the three age groups including: children (0-17 years), adults (18-64 years) and older adults (≥65 years). Using this method, the peak value of an indicator by age group and across all ages is compared to the respective IT for that indicator to arrive at a severity classification.
- Severity is classified as "low" if at least 2 of 3 indicators for the overall population peak below the respective systems' lowest IT.
- Severity is classified as "moderate" if at least two indicators for the overall population peak between the respective systems' lowest (50thpercentile) and mid-range ITs (90th).
- Severity is classified as "high" if at least two indicators for the overall population peak between the respective systems' mid-range (90thpercentile) and high ITs (98thpercentile).
- Severity is classified as "very high" if at least two indicators for the overall population peak above the respective systems' highest IT (98thpercentile).
How severity varies by age group
Seasonal severity can vary by age group. Older adults (65 years and older) experienced four seasons that were classified as high severity (2003–2004, 2012–2013, 2014–2015, and 2017-2018), the most with a classification of high severity among any of the age groups assessed. In contrast, children (0-17 years) were the only age group to experience two seasons that were classified as having very high severity (2003-2004, 2009-2010). This age group has also experienced three seasons classified as having high severity, 2017-2018, 2019-2020, and the 2022-2023 seasons. Adults (18-64 years) experienced two seasons that were classified as high severity (2017–2018 and 2019-2020).
How the COVID-19 pandemic affected the methodology for assessing severity
When COVID-19 mitigation measures, such as school closures, lockdowns, and mask wearing, were implemented in March 2020, flu-like illness activity decreased. Because of this, the period during the 2019-2020 flu season that was most impacted by the emergence of the virus that causes COVID-19 was excluded from the threshold calculation and severity assessment for that season. The 2020-2021 season was also excluded in its entirety since there was minimal flu activity that year. Additionally, most pneumonia-coded deaths during this timeframe were related to COVID-19. The number of pneumonia and influenza (P&I) combined deaths increased during the pandemic, but this increase is unlikely to reflect flu activity. To avoid bias, counts of NCHS ICD-coded flu deaths were used instead of P&I deaths to calculate mortality thresholds and assess severity.
