What to know
ACIP Recommendations for Vaccination
For additional information: MMWR 2025;74(32):500-507 at https://www.cdc.gov/mmwr/volumes/74/wr/mm7432a2.htm?s_cid=OS_mm7432a2_w.
- Routine annual influenza vaccination is recommended for all persons aged ≥6 months who do not have contraindications.
- If supply is limited, see priority groups in the 2025-26 ACIP statement (https://www.cdc.gov/mmwr/volumes/74/wr/mm7432a2.htm?s_cid=OS_mm7432a2_w).
- For most groups, vaccination should ideally be offered during September or October. Vaccination should continue throughout the season as long as influenza viruses are circulating.
- Timing considerations for specific groups include:
- For most adults (particularly those aged ≥65 years) and during the first or second trimester of pregnancy, vaccination during July and August should be avoided unless there is concern that later vaccination might not be possible.
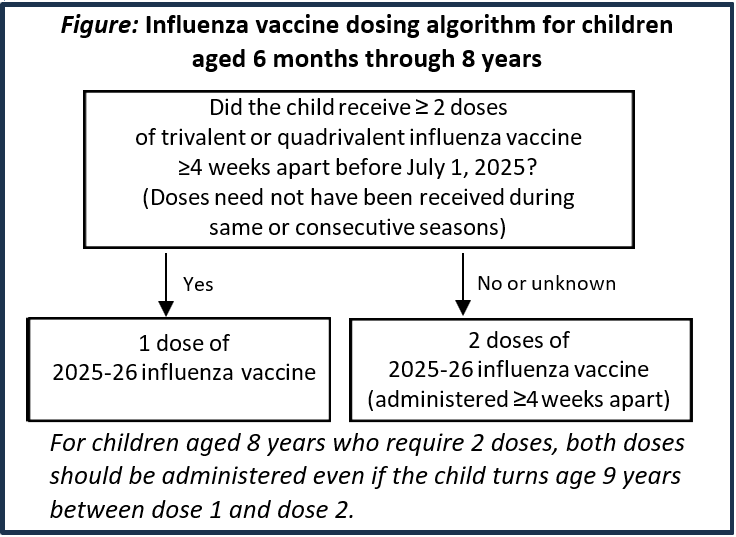
- Children aged 6 months through 8 years who need 2 doses (Figure) should receive dose 1 as soon as vaccine is available.
- Vaccination during July and August can be considered for children of any age who require only 1 dose, particularly if there is concern that later vaccination might not be possible.
- Vaccination in July and August can be considered during the third trimester of pregnancy.
- Available vaccines, approved ages, and dose volumes are listed in Table 1.
- ACIP recommends all recipients receive seasonal influenza vaccines only in single dose formulations that are free of thimerosal as a preservative (Table 1).
- All persons should receive an age-appropriate vaccine, with the exception that solid organ transplant recipients aged 18 through 64 years who are receiving immunosuppressive medication regimens may receive HD-IIV3 or aIIV3 as acceptable options (see Immunocompromised Persons).
- With the exception of Adults Aged ≥65 Years, for whom HD-IIV3, RIV3, and aIIV3 are preferred (see below), there are no preferences for any specific vaccine when more than one age-appropriate product is available.
- LAIV3 is not recommended in pregnancy, for persons with some medical conditions (Table 3), or for persons who have recently taken influenza antiviral medications (see Vaccination and Influenza Antiviral Medications).
- The selected vaccine should be administered at the appropriate dose volume for the recipient's age (Table 1). If a dose less than the necessary volume is inadvertently administered:
- If discovered before the recipient has left the vaccination setting, administer the remaining volume.
- If discovered after the recipient has left the vaccination setting, administer a repeat full dose.
- Clinical settings in which vaccines are administered should be equipped to recognize and manage acute allergic reactions.
- Women who are or who might be pregnant during the influenza season should receive influenza vaccine.
- Any age-appropriate IIV3 or RIV3 should be used and may be given in any trimester.
- LAIV3 should not be used during pregnancy but can be used postpartum.
- Determine doses needed based on child's age at time of first dose of 2025–26 influenza vaccine and number of doses of influenza vaccine received in previous seasons (Figure).
- Persons aged ≥9 years need only one dose.
- ACIP recommends that adults aged ≥65 years preferentially receive any one of the following:
- High-dose inactivated influenza vaccine (HD-IIV3, Fluzone High-Dose),
- Recombinant influenza vaccine (RIV3, Flublok), or
- Adjuvanted inactivated influenza vaccine (aIIV3, Fluad).
- If none of these three vaccines is available at a vaccination opportunity, then any other age-appropriate influenza vaccine should be used.
- Data support greater potential benefit of high-dose inactivated, adjuvanted inactivated, or recombinant vaccines relative to standard-dose unadjuvanted IIVs in this age group, with the most data available for HD-IIV3; but comparisons of these vaccines with one another are limited.
- LAIV3 is not recommended for persons with some chronic medical conditions (Table 3).
- Immunocompromised persons should receive IIV3 or RIV3. LAIV3 should not be used.
- Solid organ transplant recipients aged 18 through 64 years who are receiving immunosuppressive medication regimens may receive HD-IIV3 or aIIV3 as acceptable options (without a preference over other age-appropriate IIV3s or RIV3).
- Immune response might be reduced in persons on certain medications, chemotherapy, or transplant regimens.
- Caregivers and contacts (including those of immunosuppressed persons) may receive any age-appropriate IIV3 or RIV3.
- LAIV3 may be given to caregivers and contacts of persons who are not severely immunocompromised (i.e., who do not require a protected environment).
- Health care personnel or hospital visitors who receive LAIV3 should avoid caring for/contact with severely immunosuppressed persons who require a protected environment for 7 days after vaccination.
- Multiple studies indicate that egg-allergic persons are not at increased risk of severe allergic reactions to egg-based influenza vaccines.
- Any influenza vaccine that is otherwise appropriate for the recipient's age and health status (egg based or non-egg based) can be administered to persons with egg allergy.
- Egg allergy necessitates no additional safety measures for influenza vaccination beyond those recommended for any recipient of any vaccine.
- Clinical settings in which vaccines are administered should be equipped to recognize and manage acute allergic reactions.
- Recommendations for persons with a previous severe allergic reaction to an influenza vaccine are summarized in Tables 3 and 4.
- Clinical settings in which vaccines are administered should be equipped to recognize and manage acute allergic reactions.
- Travelers who wish to reduce risk for influenza should consider vaccination, preferably ≥2 weeks before departure.
- Persons at higher risk for complications of influenza who were not vaccinated during the preceding fall or winter should consider influenza vaccination before departure, if planning to travel to the tropics, with organized tourist groups, on cruise ships, or to the Southern Hemisphere during April-September.
- Southern Hemisphere influenza vaccines might differ in viral composition from Northern Hemisphere formulations.
- Administration of Southern Hemisphere influenza vaccine before Southern Hemisphere travel might be reasonable, but these formulations are generally unavailable in the U.S.
- Influenza antivirals given before or after LAIV3 might reduce its effectiveness. Persons who receive influenza antivirals within the following intervals should be revaccinated with an age-appropriate IIV3 or RIV3 (intervals might be longer in conditions where medication clearance is delayed):
Influenza Antiviral
Estimated window for potential interference
Oseltamivir and Zanamivir
48 hours before to 2 weeks after LAIV3
Peramivir
5 days before to 2 weeks after LAIV3
Baloxavir
17 days before to 2 weeks after LAIV3
- IIV3s and RIV3 may be administered simultaneously or sequentially with other live or inactivated vaccines.
- LAIV3 may be administered simultaneously with other inactivated or live vaccines. If not given simultaneously, then ≥4 weeks should pass between administration of LAIV3 and another live vaccine.
- Injectable vaccines given simultaneously should be administered at separate anatomic sites ≥1 inch apart.
- Consider using non-adjuvanted influenza vaccine if giving another vaccine with non-aluminum adjuvant simultaneously (but vaccination should not be delayed to obtain a nonadjuvanted influenza vaccine).
- Health care providers are required to report to VAERS any adverse event listed by the vaccine manufacturer as a contraindication to further doses of that vaccine and also are required to report adverse events listed here: https://vaers.hhs.gov/docs/VAERS_Table_of_Reportable_Events_Following_Vaccination.pdf. They are encouraged to report any clinically significant adverse event after vaccination to VAERS.
CDC Influenza Information (for more, call 800-232-4636)
U.S. Influenza Vaccines, Age Indications, Dosage and Administration, and Contraindications and Precautions
Table 1: Inactivated Influenza Vaccines (IIV3s) and Recombinant Influenza Vaccine (RIV3)
For package inserts see: https://www.fda.gov/vaccines-blood-biologics/vaccines/vaccines-licensed-use-united-states
For 2025-26 vaccine composition, see https://www.cdc.gov/mmwr/volumes/74/wr/mm7432a1.htm.
| Trade Name (Manufacturer) | Presentations | Approved ages | Volume per dose by age group | Thimerosal as preservative | Comments |
|---|---|---|---|---|---|
| IIV3s: Standard-dose (15 µg HA per virus component in 0.5 mL; 7.5 µg in 0.25 mL) | |||||
| Afluria (Seqirus) | 0.5 mL PFS | ≥3 yrs† | ≥3 yrs—0.5 mL† | No | Egg-based.
MDV no longer recommended. |
| 5.0 mL MDV* | ≥6 mos† | 6 through 35 mos—0.25 mL† | Yes | ||
| ≥3 yrs—0.5 mL† | |||||
| Fluarix (GlaxoSmithKline) | 0.5 mL PFS | ≥6 mos | ≥6 mos—0.5 mL | No | Egg-based. |
| Flucelvax (Seqirus) | 0.5 mL PFS | ≥6 mos | ≥6 mos—0.5 mL | No | Cell culture-based.
MDV no longer recommended. |
| 5.0 mL MDV* | ≥6 mos | ≥6 mos—0.5 mL | Yes | ||
| FluLaval (GlaxoSmithKline) | 0.5 mL PFS | ≥6 mos | ≥6 mos—0.5 mL | No | Egg-based. |
| Fluzone (Sanofi Pasteur) | 0.5 mL PFS | ≥6 mos§ | ≥6 mos—0.5 mL§ | No | Egg-based.
MDV no longer recommended. |
| 5.0 mL MDV* | ≥6 mos§ | ≥6 mos—0.5 mL§ 6 through 35 mos—0.25 or 0.5 mL§ ≥3 yrs—0.5 mL§ |
Yes | ||
| HD-IIV3: High-dose (60 µg hemagglutinin per virus component in 0.5 mL) | |||||
| Fluzone High-Dose (Sanofi Pasteur) | 0.5 mL PFS | ≥65 yrs | ≥65 yrs—0.5 mL | No | One of 3 options preferred for ≥65 years. Egg-based. |
| aIIV3: Standard-dose, with MF59 adjuvant (15 µg hemagglutinin per virus component in 0.5 mL) | |||||
| Fluad (Seqirus) | 0.5 mL PFS | ≥65 yrs | ≥65 yrs—0.5 mL | No | One of 3 options preferred for ≥65 years. Egg-based. |
| RIV3: Recombinant HA (45 µg hemagglutinin per virus component in 0.5 mL) | |||||
| Flublok (Sanofi Pasteur) | 0.5 mL PFS | ≥9 yrs | ≥9 yrs—0.5 mL | No | One of 3 options preferred for ≥65 years. |
Abbreviations: MDV=multidose vial; PFS=prefilled syringe
* ACIP recommends only single-dose seasonal influenza vaccines that are free of thimerosal as a preservative for all recipients.
† The approved dose volume for Afluria is 0.25 mL for children 6 through 35 months and 0.5 mL for persons ≥3 years. However, 0.25-mL prefilled syringes are no longer available, and use of MDVs is no longer recommended.
§ The approved dose volume for Fluzone is either 0.25 mL or 0.5 mL for children 6 through 35 months and 0.5 mL for persons ≥3 years. However, 0.25-mL prefilled syringes are no longer available, and use of MDVs is no longer recommended.
Administration of IIV3s and RIV3
- IIV3s and RIV3 are administered intramuscularly (IM). For adults and older children, the deltoid is the preferred site. For infants and younger children, the anterolateral thigh is the preferred site. For detailed guidance for administration sites and needle length, see the General Best Practice Guidelines for Immunization (see Further Information).
Table 2: Live Attenuated Influenza Vaccine (LAIV3) — 10 6.5-7.5 fluorescent focus units live attenuated virus in 0.2 mL
| Trade name/Manufacturer | Presentations | Approved ages | Volume per dose | Thimerosal as preservative | Comment |
|---|---|---|---|---|---|
| FluMist (AstraZeneca) | 0.2 mL prefilled single-use intranasal sprayer | 2 through 49 yrs | 0.1 mL each nostril (0.2 mL total) |
No | Egg-based |
Administration of LAIV3
- LAIV3 is administered intranasally. Half of the total sprayer contents is sprayed into the first nostril while the recipient is in the upright position. The attached divider clip is removed and the second half is administered into the other nostril.
- If the vaccine recipient sneezes immediately after administration, the dose should not be repeated.
- If nasal congestion is present that might interfere with delivery of the vaccine to the nasopharyngeal mucosa, deferral should be considered, or another age-appropriate vaccine should be administered.
- LAIV3 is available for self- (for recipients ages 18 through 49 years) or caregiver (for recipients ages 2 through 17 years) administration through the FluMist Home program..
Vaccine Abbreviations
- Main influenza vaccine types:
- IIV3= Inactivated Influenza Vaccine
- RIV3= Recombinant Influenza Vaccine
- LAIV3= Live Attenuated Influenza Vaccine
- Prefixes sometimes used for specific vaccines:
- cc for cell culture based IIV (e.g., ccIIV3)
- a for adjuvanted IIV (e.g., aIIV3)
- HD for high-dose IIV (e.g., HD-IIV3)
Table 3: Influenza Vaccine Contraindications and Precautions
Egg based IIV3s
Contraindications:
- History of severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine (other than egg), or to a previous dose of any influenza vaccine (any egg-based IIV, ccIIV, RIV, or LAIV of any valency)
Precautions:
- Moderate or severe acute illness with or without fever
- History of Guillain-Barré syndrome within 6 weeks of receipt of influenza vaccine
ccIIV3
Contraindications:
- History of severe allergic reaction (e.g., anaphylaxis) to ccIIV of any valency, or to any component of ccIIV3
Precautions:
- Moderate or severe acute illness with or without fever
- History of Guillain-Barré syndrome within 6 weeks of receipt of influenza vaccine
- History of severe allergic reaction to a previous dose of any other influenza vaccine (any egg-based IIV, RIV, or LAIV of any valency)
RIV3
Contraindications:
- History of severe allergic reaction (e.g., anaphylaxis) to RIV of any valency, or to any component of RIV3
Precautions:
- Moderate or severe acute illness with or without fever
- History of Guillain-Barré syndrome within 6 weeks of receipt of influenza vaccine
- History of severe allergic reaction to a previous dose of any other influenza vaccine (any egg-based IIV, ccIIV, or LAIV of any valency)
LAIV3
Contraindications:
- History of severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine (other than egg) or to a previous dose of any influenza vaccine (i.e, any egg-based IIV, ccIIV, RIV, or LAIV of any valency)
- Concomitant aspirin or salicylate-containing therapy in children and adolescents
- Children aged 2 through 4 years who have received a diagnosis of asthma or whose parents or caregivers report that a health care provider has told them during the preceding 12 months that their child had wheezing or asthma or whose medical record indicates a wheezing episode has occurred during the preceding 12 months
- Children and adults who are immunocompromised due to any cause, including but not limited to medications, congenital or acquired immunodeficiency states, HIV infection, anatomic asplenia, or functional asplenia (e.g., in sickle-cell anemia)
- Close contacts and caregivers of severely immunosuppressed persons who require a protected environment
- Pregnancy
- Persons with active communication between the cerebrospinal fluid (CSF) and the oropharynx, nasopharynx, nose, or ear or any other cranial CSF leak
- Persons with cochlear implants (due to potential for CSF leak, which might exist for some period after implantation. Providers might consider consultation with a specialist concerning risk of persistent CSF leak if an age-appropriate inactivated or recombinant vaccine cannot be used)
- Receipt of influenza antiviral medication within the previous 48 hours for oseltamivir and zanamivir, 5 days for peramivir, and 17 days for baloxavir (see Vaccination and influenza antiviral medications, above, for additional guidance)
Precautions:
- Moderate or severe acute illness with or without fever
- History of Guillain-Barré syndrome within 6 weeks of receipt of influenza vaccine
- Asthma in persons aged ≥5 years
- Other underlying medical conditions that might predispose to complications after wild-type influenza infection (e.g., chronic pulmonary, cardiovascular [except isolated hypertension], renal, hepatic, neurologic, hematologic, or metabolic disorders [including diabetes mellitus])
Table 4: Contraindications and Precautions for Persons with a History of Severe Allergic Reaction to an Influenza Vaccine
| Vaccine (of any valency) associated with previous severe allergic reaction (e.g., anaphylaxis) | Available 2025–26 influenza vaccines | ||
|---|---|---|---|
| Egg-based IIV3s and LAIV3 | ccIIV3 | RIV3 | |
| Any egg-based IIV or LAIV | Contraindication* | Precaution† | Precaution† |
| Any ccIIV | Contraindication* | Contraindication* | Precaution† |
| Any RIV | Contraindication* | Precaution† | Contraindication* |
| Unknown influenza vaccine | Allergist consultation recommended | ||
*When a contraindication is present, a vaccine should not be administered. In addition to the contraindications based on history of severe allergic reaction to influenza vaccines noted in the Table, each individual influenza vaccine is contraindicated for persons who have had a severe allergic reaction (e.g., anaphylaxis) to any component of that vaccine. Vaccine components can be found in package inserts. Although a history of severe allergic reaction (e.g., anaphylaxis) to egg is a labeled contraindication to the use of egg-based IIV3s and LAIV3, ACIP makes an exception for allergy to egg (see Persons with Egg Allergy).
†When a precaution is present, vaccination should generally be deferred but might be indicated if the benefit of protection from the vaccine outweighs the risk for an adverse reaction. Providers can consider using vaccines for which there is a precaution; however, vaccination should occur in an inpatient or outpatient medical setting with supervision by a health care provider who is able to recognize and manage severe allergic reactions. Providers can also consider consulting with an allergist to help determine which vaccine component is responsible for the allergic reaction.
