At a glance

Success stories: EHE in action
Read the inspirational stories below to learn how jurisdictions are using EHE resources to address unique challenges facing their communities.
Find out how EHE resources are supporting promising practices to reach people that access HIV care in STI clinics.
Post-exposure prophylaxis (PEP) is emergency medicine that can prevent HIV when a possible exposure has occurred. But it must be taken as soon as possible within 72 hours after exposure. Health officials in Philadelphia found that many people who could benefit from PEP did not use it. Many were unaware of the strategy. Fortunately, Ending the HIV Epidemic (EHE) initiative funding made it possible to implement a program in Philadelphia to boost access to and use of PEP.
“We saw missed opportunities to prevent HIV with PEP,” said Dr. Kathleen Brady, Philadelphia’s Director of HIV Health. “EHE funding helped us seize these opportunities. In a short time, we’ve turned the idea of expanding PEP use into reality.”
Strategies for Expanding PEP Use
In 2022, the Philadelphia Department of Health and partners at the University of Pennsylvania Health System established a PEP Center of Excellence (COE). The Center provides a 24/7, clinician-staffed PEP Hotline to assess callers for PEP eligibility and provide prescriptions to those eligible for it.
Hotline callers also get help finding a pharmacy that is open and stocked with PEP medications. Additionally, dedicated PEP navigators help with overcoming insurance coverage barriers, when needed.
To spread the word about PEP, the COE integrated hotline information into Philadelphia's sexual health website, phillykeeponloving.com. They also created a series of digital "Don't Worry, Just Hurry" ads that appear on dating apps and in relevant web searches.
These efforts are paying off. In the hotline’s first 21 months, nearly 500 people called in. More than 200 callers were eligible for PEP based on clinical indication, and because they either resided in Philadelphia or were exposed to HIV there. Among those eligible, 95% picked up prescriptions and took the first dose within the 72-hour window.
“When people need PEP, they need it right away,” said Emily McNamara, who coordinates the COE. “We work to reach people in those specific moments.”

EHE resources provided the boost South Carolina’s Department of Public Health (DPH) needed to accelerate pre-exposure prophylaxis (PrEP) delivery efforts.
"We've been offering PrEP for years, but the community told us many people don't know about it," said Tony Price, prevention program manager for DPH's STI, HIV, and Viral Hepatitis Program. "EHE funding opened the door for us to get the message out and help people access PrEP."
Strategies for Expanding Access to PrEP
DPH partners worked with eight community-based organizations to deliver PrEP in every South Carolina county. Funded partners must hire PrEP navigators to assist clients with staying engaged while receiving PrEP services. Thanks to these services, in 2023, South Carolina screened nearly 10,000 clients for PrEP. More than 1,800 people were referred to a PrEP provider for a prescription.
DPH also hosts an annual PrEP Awareness Week with community partners. In 2023, more than 20 colleges and universities participated in community events during PrEP Awareness Week. From Spartanburg in the state’s northwest to coastal Charleston, these events included HIV testing, and distributed PrEP information.
“Student partnerships are critical for our college events,” said DPH PrEP Program Manager Dr. Tia Robinson. “Students know how to encourage their peers to get tested, and some have become powerful campus PrEP champions.”
Building PrEP awareness among women is another DPH priority. Efforts to reach this key group include ensuring that PrEP brochures are distributed at family planning clinics.
Year-round, DPH also sponsors digital and outdoor marketing to increase PrEP awareness. For example, they created bus wraps (advertising placed on bus surfaces) and billboards. “People need to see a message multiple times before it penetrates,” said Price. “Now PrEP messaging literally circulates around our streets.”
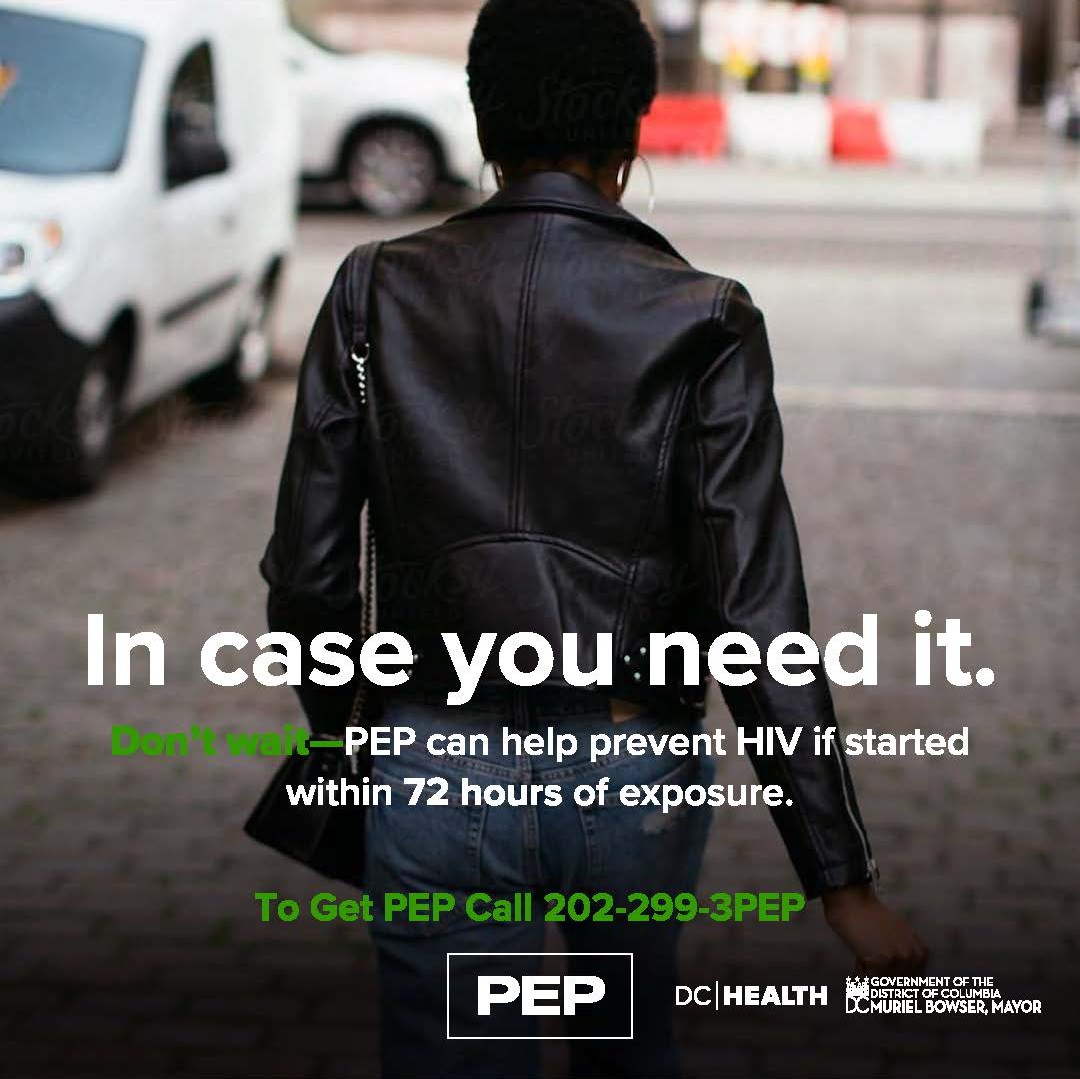
Taking HIV medicine after a potential HIV exposure is known as post-exposure prophylaxis (PEP). If taken within 72 hours of possible exposure, PEP can help prevent HIV infection. Unfortunately, many people are unaware of this strategy or cannot access or afford the necessary medications. In Washington, D.C., health officials used EHE funding to help more people benefit from PEP.
Strategies for Increasing Accessibility of PEP
In March 2021, DC’s HIV/AIDS, Hepatitis, STD, and TB Administration (HAHSTA) launched its PEP Hotline, (202) 299-3PEP (3737). With EHE funding, HAHSTA recruited academic partners to help answer hotline calls, 24/7.
“HIV exposures most frequently happen on Friday and Saturday night,” said Jason Beverley, a nurse practitioner overseeing HAHSTA’s clinical care services. “Our partners keep the PEP Hotline open, even when the clinic is closed.”
Hotline responders are clinicians who can immediately offer eligible callers a prescription. This ensures people who need PEP, can start it within 72 hours of an exposure. HAHSTA further facilitates the PEP process by contracting directly with pharmacies to fill PEP prescriptions. They also streamline insurance billing and connect patients to assistance programs.
To raise awareness of the hotline, HAHSTA launched focused social media and marketing campaigns. Community partners with deep ties to key populations also helped HAHSTA promote the hotline.
More than 400 people started PEP during the hotline’s first 18 months. During the year before the hotline’s launch, about 30 people started PEP. After finishing their PEP medications, 4 in 10 hotline users transitioned to pre-exposure prophylaxis (PrEP) for ongoing HIV prevention.
“I’m proud of the PEP Hotline,” said Beverley. “It eases people’s fears and reduces the burden of HIV in our communities.”
Lowering rates of HIV and sexually transmitted infections (STIs) is a top priority for the Baltimore City Health Department (BCHD). In 2020, COVID-19 forced clinics to limit or suspend in-person services—including HIV and STI testing.
In response, BCHD used EHE funding to embrace non-traditional service delivery methods. Partnering with I Want the Kit, BCHD delivered thousands of test kits and helped link people to care.
Strategies for breaking down barriers to HIV and STI testing and care
BCHD partnered with I Want the Kit to increase the distribution of HIV self-tests and STI mail-in tests. In 2020, they processed over 1,800 HIV self-tests and over 5,500 chlamydia/gonorrhea mail-in tests.
BCHD and I Want the Kit implemented a user-friendly testing process. The kits included sample collection swabs and tubes, discreet packaging, simple instructions, information on STIs, and pre-paid mailing materials. This made it easier for people to collect and submit samples.
BCHD partnered with the University of Maryland's STAR TRACK program to develop a youth at-home HIV and STI testing program. The discreet box contains free HIV and/or STI test kits and educational materials on sexual health. Recipients order online or receive a kit through STAR TRACK's mobile van.
For increased privacy, BCHD and I Want the Kit provided USPS mailbox locations through QR codes included in test kits.
Elizabeth Gilliam, MD, MSC, Medical Director of STI Services, Baltimore City Health Department Sexual Health Clinics
Yukari Manabe, MD, Johns Hopkins Center for Innovative Diagnostics for Infectious Diseases
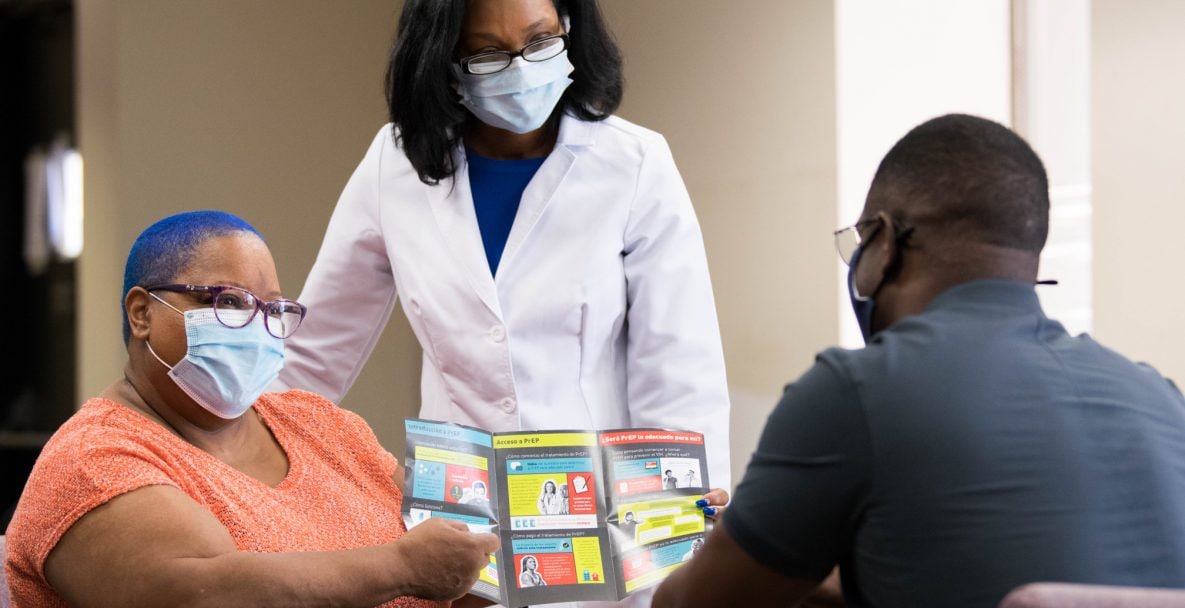
T.O. Vinson is a health center operated by the DeKalb County Board of Health in the Atlanta, Georgia area. In recent years, staff heard some clients were reluctant to try game-changing HIV prevention options like pre-exposure prophylaxis, or PrEP.
With support from EHE, T.O. Vinson launched a new PrEP program. This program expanded the reach of the healthcare system by enabling registered nurses (RNs) to connect more people in DeKalb County to vital HIV prevention options.
Strategies for connecting people to PrEP
The Georgia Department of Public Health published a new protocol allowing RNs to evaluate and order PrEP for eligible patients. EHE resources were used to train RNs at T.O. Vinson to offer PrEP through the new protocol.
During patient discussions, nurses can now offer PrEP to patients at T.O Vinson. Discussions often include helping patients acknowledge they are at risk for HIV and that their health is worth protecting.
Through EHE, T.O. Vinson hired new staff to educate people considering PrEP, and provide critical education, support, and follow-up care after a PrEP prescription.
DeKalb County and the Georgia Department of Public Health launched a print and social media advertising campaign promoting PrEP. The ads, posted in English and Spanish, were widely visible on Atlanta's public transit system and in a local mall.
Dr. Sentayehu Bedane, Countywide Services Manager, DeKalb County Board of Health
Dr. Gregory Felzien, Medical Advisor, Georgia Department of Public Health
Ebonee Gresham, RN, MSN, Clinical Nurse Coordinator, T.O. Vinson Health Center
Darlene McDougle, Public Health Educator, T.O. Vinson Health Center
In Louisiana's East Baton Rouge Parish, the rate of people living with HIV is triple the national average. But the parish is driving efforts to end the HIV epidemic.
With support from EHE, leaders came together to confront HIV. They harnessed the power of the emergency room to diagnose HIV earlier and get people with HIV into treatment. Community leaders also shared strategies and resources to connect people at risk with critical HIV prevention, treatment, and support services.
Strategies for expanding HIV diagnosis, treatment, and prevention
With EHE resources, the Louisiana Department of Health hired community health workers to take services into the community. They distributed condoms and information about PrEP, screened individuals for HIV, hepatitis C, and syphilis, and linked people to care.
Ochsner Medical Center – Baton Rouge began an opt-out testing program and receives support through EHE.
East Baton Rouge Parish hired a Rapid Start Navigator to connect people with HIV to appropriate care quickly.
East Baton Rouge Parish also hired an EHE Coordinator to develop a blueprint for ending the parish's HIV epidemic. This involved meeting with staff to learn about existing HIV prevention efforts, identifying opportunities or interventions with the greatest impact, and working closely with staff to organize a workshop to determine the parish's HIV prevention and care priorities.

Isaac Gilliard, Lead Community Health Worker, East Baton Rouge Parish, Louisiana Department of Health
Susan Green, Emergency Department Director, Ochsner Medical Center – Baton Rouge
Mathilde Silverberg, Ending the HIV Epidemic Coordinator, East Baton Rouge Parish
Access to traditional, in-person healthcare services, including HIV testing, were disrupted by COVID-19. EHE and Minority HIV/AIDS Fund investments were needed to bridge service gaps.
With these investments, CDC launched a project to mail 100,000 HIV self-tests to members of communities most affected by HIV. CDC closed the online ordering portal after all 100,000 self-tests were distributed in just eight months. A follow-up program, Together TakeMeHome, aims to deliver up to 1 million free HIV self-tests over five years.
Strategies for delivering HIV self-testing
CDC created an online portal where people could place an order for in-home HIV Test kits at no cost. To increase awareness, CDC promoted HIV self-testing through the Let's Stop HIV Together campaign and placed advertisements on digital platforms.
CDC tailored communications for priority populations on channels known to be effective in reaching them. Priority populations included Black/African American and Hispanic/Latino gay and bisexual men, Black cisgender women, and transgender women. CDC also worked with Together Ambassadors, Together PACT partners, and social media influencers to raise awareness of the project.
CDC partnered with influencers to promote awareness of HIV self-testing, including New York City-based musician and social media influencer Teraj. Teraj highlighted the importance of knowing one's HIV status and linked to CDC's Let's Stop HIV Together campaign. He engaged personally through comments and direct messages to help people access needed resources. CDC continues to support local self-testing programs.

Pollyanna Chavez, Division of HIV Prevention, CDC
Emily Lilo, Division of HIV Prevention, CDC
During COVID-19, HIV clinics and people seeking HIV-related services had to adapt to a new reality. Telehealth became a crucial and transformative way for some HIV clinics to provide a lifeline to patients. Telehealth is the distribution of health-related services and information via phone, tablet, or computer.
In rural Kentucky, two organizations created successful telehealth models using EHE funding. These organizations show how forward-thinking strategies can strengthen health systems, build meaningful connections with people with HIV, and save lives.
Strategies for using telehealth to provide treatment and support for people with HIV
LivWell Community Health Services in Paducah, KY launched a HIPAA-compliant telehealth platform. LivWell worked with patients to overcome technological and socioeconomic barriers. This included remotely measuring vital signs and arranging visits to other health or laboratory clinics that were open and accessible. Since then, 89% of LivWell's patients have been seen via telehealth and 95% of their patients are virally suppressed.
The Matthew 25 AIDS Services clinic in Bowling Green, KY implemented a hybrid in-person/telehealth program. Patients arrived in-person to give blood and take vital signs and were virtually connected to an off-site provider. State-of-the-art equipment allowed for remote examination of the lungs, heart, skin, and oral cavity. In 2020, 90% of Bowling Green's active patients were virally suppressed. In 2021, that number increased to 94%.

Donna Reeder, LivWell Community Health Services Executive Director
Andrea Leonard, Ryan White HIV/AIDS Program Part B Manager, LivWell Community Health Services
Cyndee Burton, Matthew 25 AIDS Services Founder and Administrator
Ashley Lynch, Medical Office Manager, LivWell Community Health Services
In 2021, health officials in Atlanta, Georgia identified several rapidly growing clusters of new HIV diagnoses. These clusters predominantly included young Hispanic and Latino gay and bisexual men. The growth of the clusters suggested considerable gaps in HIV prevention services for young gay and bisexual men.
Area health departments used EHE funding to close these prevention gaps. As a result, culturally informed, community-based interventions built bridges with Hispanic and Latino gay and bisexual men.
Strategies for addressing growing HIV clusters
Local and state health officials visited service providers, clinics, bars, and nightclubs to learn from the community the barriers to HIV prevention. They learned few area healthcare providers spoke Spanish. HIV prevention and other health campaigns and materials were mostly in English. Existing Spanish materials did not reflect local needs and values.
Officials ensured providers and materials reflected community needs. The state's application for the federal Ryan White program was translated into Spanish. Educational materials and Spanish-language social media campaigns for Hispanic and Latino communities were created with the specific community needs and values in mind. And bilingual health providers and support staff were hired.
A collective response included local health departments and affected communities. Community organizations, local service providers, and members of academic institutions met regularly to discuss the response. County health departments used federal resources to develop a unified prevention and care infrastructure. The state and CDC created a dashboard to help officials visualize and understand HIV cluster data.
Dorian Freeman, clinical infectious disease program director for GNR Public Health
Gilda Pedraza, Executive Director of the Latino Community Fund (LCF) Georgia
Eric Rangel, Board President at Latino LinQ
Dr. Carlos Saldana, Fulton County Board of Health
Eleanor Garlow, Georgia Department of Public Health
Expanding access to pre-exposure prophylaxis (PrEP) is critical to EHE's success. With CDC support, NASTAD works to address structural and social barriers to accessing and using PrEP.
In 2020-2021, COVID-19-related healthcare disruptions made it more challenging to get or stay on PrEP. To increase PrEP access and uptake, NASTAD used EHE funding to help EHE jurisdictions design and implement telePrEP programs. These programs were tailored to each jurisdiction's needs and barriers.
Strategies for bridging gaps in PrEP access
NASTAD launched the TelePrEP Learning Collaborative, a virtual learning community for staff in EHE jurisdictions developing telePrEP programs. Through the collaborative, jurisdiction staff could seek specialized technical and capacity building assistance. Participants saw their telePrEP services strengthened or expanded.
Building on the success of its program, NASTAD created the TelePrEP Online Learning Series. This platform grants all EHE jurisdictions access to regularly updated PrEP resources. Staff in jurisdictions across the country can review materials for their specific programs on their own schedules.
The TelePrEP Learning Collaborative led to new and enduring participant relationships with each other and with NASTAD. These relationships enable jurisdictions to share best practices as they design and implement telePrEP and expand PrEP access. NASTAD continues to share new resources and PrEP access updates and holds routine virtual office hours to support ongoing efforts.

Javontae Lee Williams, MPH, Program Manager, Philadelphia Department of Public Health
Nicholas Sanders, Senior Program Manager of Prevention Services, Damien Center
Nicole Elinoff, Senior Manager, Prevention, NASTAD
Find the latest news and announcements.
