Key points
- Chromoblastomycosis is a skin infection caused by fungi that live in soil and on wood and plants.
- People get chromoblastomycosis through scrapes in the skin often caused by thorns.
- Chromoblastomycosis is most common in tropical and subtropical areas, but cases have been reported in the United States.
- Without treatment, chromoblastomycosis can cause limb swelling, difficulty walking, skin cancer, and scarring of the skin.
- These physical effects can lead to social stigma.
Overview
Chromoblastomycosis is a fungal infection usually affecting the skin. It is typically caused by fungi in the soil and on wood and plants.
The World Health Organization designated chromoblastomycosis as a neglected tropical disease. It is most common among populations that are socially and economically marginalized in tropical and subtropical areas. However, it is possible to get infected anywhere, including in the United States, but this is not common.
Chromoblastomycosis may cause swelling and unsightly enlargement of infected limbs. Rarely, chromoblastomycosis can lead to skin cancer or affect other organs like the brain. The physical effects of infection can lead to disability and stigma.
There are no surveillance programs for chromoblastomycosis, and many cases are never diagnosed. The global burden of disease is unknown.
Signs and symptoms
Chromoblastomycosis is usually a skin infection. It can also affect the innermost layer of skin called subcutaneous tissue.
Symptoms can include:
- Dark wart-like bumps most commonly on the legs and arms
- Flattened patches or scarring of patches of skin
- Pain and itching may occur, especially in severe disease
Infections can slowly spread to other parts of the body over months or years. Left untreated, it can lead to severe limb swelling and large bumps which may limit the movement of these areas. Sometimes, infected limbs can have an unpleasant smell.
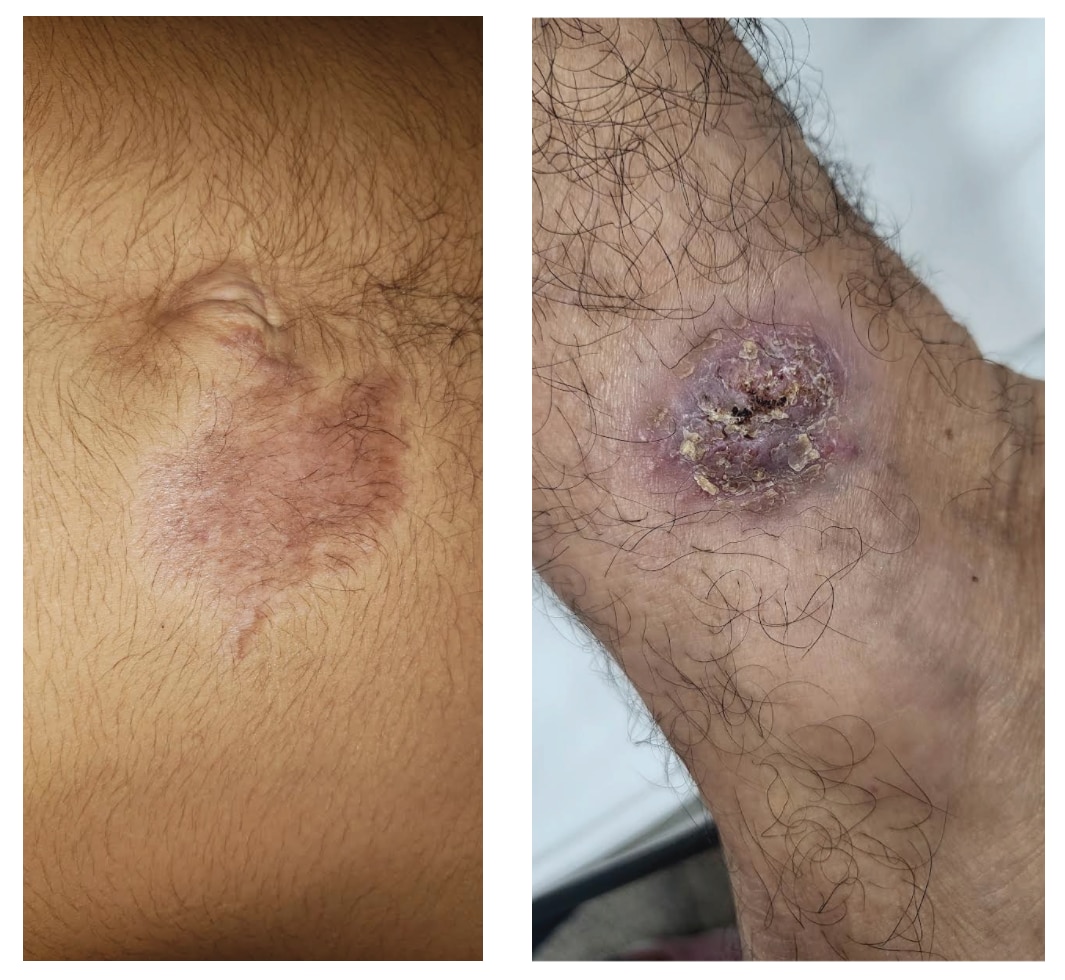
Photo credit: Conceicão de Maria Pedrozo e Silva de Azevedo from Universidade Federal do Maranhão, Maranhão, Brazil.
Risk factors
In areas where chromoblastomycosis common
Chromoblastomycosis is mostly seen in tropical and subtropical regions. In areas where it is common everyone is at risk. Health status and underlying conditions do not appear to impact risk.
People who work or do activities outdoors (such as farmers, gardeners, forestry workers, vendors of farm products) are most at risk.
In the United States
In the United States, chromoblastomycosis is very rare but it is still possible to get infected. People can also get infected during travel. Unlike in endemic areas, people living in the United States that get infected, usually have a weakened immune system.
Causes
Chromoblastomycosis is caused by a break in the skin allowing the fungus to enter. Injuries that can cause chromoblastomycosis include:
- Being pricked by thorns
- A scrape from a sharp surface (like wood or concrete)
- Insect stings and bites
However, most people do not remember when they were infected or had an injury.

Prevention
Preventing chromoblastomycosis is difficult. Wearing protective clothing, shoes, and other gear when outdoors may reduce the chance of injury that can cause an infection.
Early diagnosis and treatment can help prevent severe disease, disability, and long-term complications.
Testing and diagnosis
Chromoblastomycosis can look like other infectious and noninfectious skin conditions. A lab test is needed to diagnosis chromoblastomycosis.
To test for chromoblastomycosis, a healthcare provider may collect a scrape or small tissue sample (skin biopsy). They may examine the biopsy under a microscope or send this to be cultured.
No blood tests are currently used to diagnose chromoblastomycosis.
Treatment and recovery
Chromoblastomycosis is usually treated with antifungals taken by mouth. Two commonly used medications are itraconazole and terbinafine. Treatment is usually given for 3-6 months. Sometimes, several years of medication are needed in severe disease.
Often, surgery to remove the affected area is needed in addition to antifungal therapy. Other treatment methods include local application of heat, cryotherapy, and photodynamic therapy.
